|
Abstract
Cornual ectopic pregnancy is a rare form of ectopic pregnancy but has catastrophic presentation when diagnosis is missed. It is usually misdiagnosed as degenerated myoma at uterine fundus but can be differentiated by positive pregnancy test, absence of intrauterine gestational sac and diagnostic laparoscopy when necessary. In this case, we present a case of cornual ectopic pregnancy diagnosed by serial serum beta subunit of human chorionic gonadotropin, vaginal ultrasound and diagnostic laparoscopy, which was managed by evacuation of the cornual ectopic by laparotomy, excision of the tube and then suturing the pedicle adjacent to the uterine wall.
Keywords: Beta subunit of human chorionic gonadotropin; Cornual ectopic pregnancy; Vaginal ultrasound.
Introduction
Ectopic pregnancy is defined as implantation of the fertilized ovum in tissue other than the endometrium.1 Although cornual ectopic pregnancy is a rare event which represents about 2% to 4% of all tubal pregnancies,2 the risk of maternal mortality of this type is about 2% to 2.5%. Cornual pregnancies usually present signs and symptoms with advanced gestational age; this is because the gestational sac is surrounded by the thick myometrial walls in contrast to the weak thin-walled fallopian tube. If rupture occurs, this area is so well vascularized by anastomosis of the uterine and ovarian vessels so that hemorrhage can be profuse. The therapy for this condition usually consists of either hysterectomy or cornual resection as the treatment of choice,3,4 but many cases have recently been treated by successful endoscopic surgeries without apparent complications in the hands of experienced surgeons,5 thus the next pregnancy must be managed by elective cesarean section at 36 to 37 weeks to prevent any expected uterine rupture.
Case Report
A 40-year-old female patient presented to the gynecological clinic at King Hussein Medical Center on 07/10/2012 with chief complaints of mild lower abdominal pain and vaginal spotting of two days duration. Her last menstrual period was on 15/08/12 which was regular and of normal pattern, not did the patient use any method of contraception. She has four live sons and four live daughters who were the product of full term normal vaginal deliveries, her past medical and surgical histories were insignificant. On examination, she was cachectic, pale, with pulse of 84 beats per minute, blood pressure of 130/85 mmHg, temperature 37.20ºC, and respiratory rate of 26 per minute. Abdominal examination revealed mild tenderness on the left lower abdomen, while rebound tenderness was negative with no palpable masses.
On vaginal examination, the cervix was closed with no vaginal bleeding. Cervical excitation was also negative, but there was tenderness on the left lower abdomen on bimanual examination. By transvaginal ultrasound examination, there was a bulky empty uterus with a 3.8 × 4 cm hypoechoic lesion in the left part of the uterine fundus with internal echogenic line and rim of hypoechoic fluid; no free fluid was detected in the Douglas pouch.
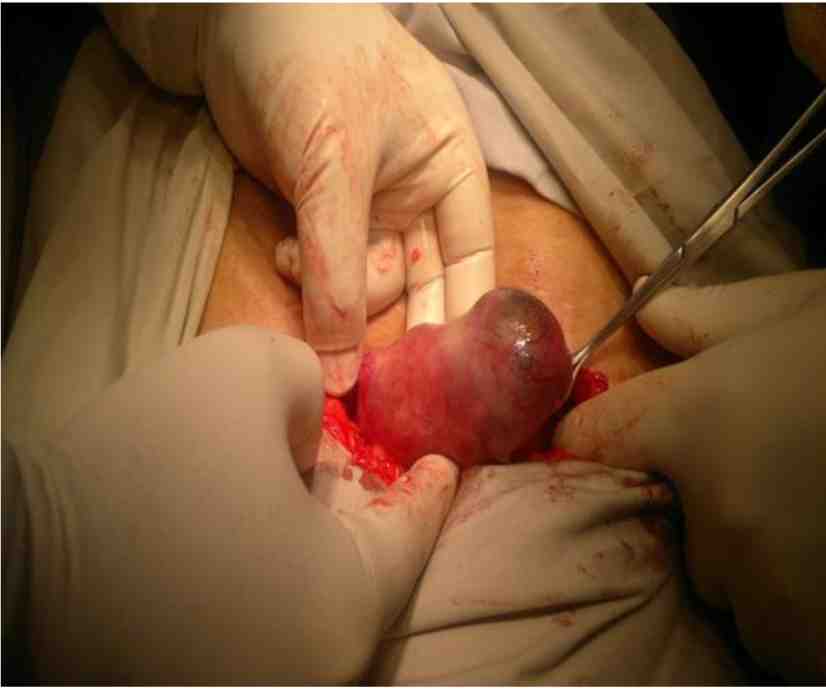
Figure 1: Laparotomy revealing a left intact, tense and shiny cornual mass.
Serum beta subunit of human chorionic gonadotropin on 08/10/12 was 718 mIU/mL. On 10/10/12 it was 497 mIU/mL while on 12/10/12 it was 338 mIU/mL. Serial packed cell volume was done and there was no change in the results. Vital signs were stable. Based on the previous finding, it was decided to do diagnostic laparoscopy which revealed left intact cornual mass about 4 × 4 cm in size with no free blood in the Douglas pouch. Laparotomy through low transverse incision was done and revealed a left intact, tense and shiny cornual mass with no active bleeding (Fig. 1). A longitudinal incision along the tube was done with the evacuation of the tubal contents (Fig. 2). The size of the mass was decreased and the left tube was clamped and excised. The pedicle was sutured with 0-Vicryl (Fig. 3), and hemostasis was secured. The specimens were then sent for histopathology.

Figure 2: Evacuation of tubal contents through a longitudinal incision along the tube.
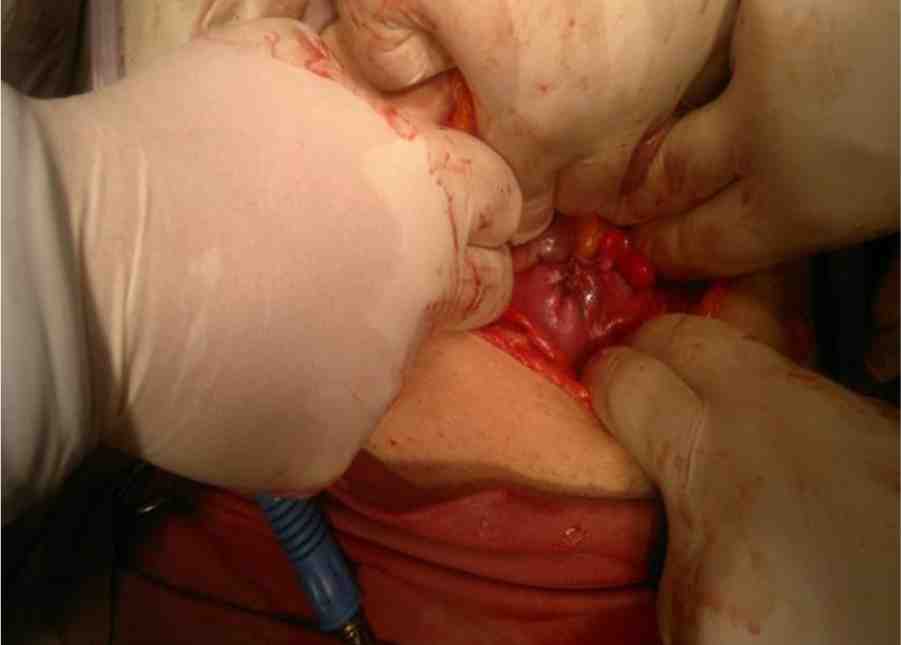
Figure 3: 0-Vicryl suture of the pendicle.
Discussion
Most ectopic pregnancies usually occur in the fallopian tube and account for approximately 90% of all ectopic pregnancies, and is followed by the less common cornual pregnancies accounting for about 2% to 4%. Early recognition of the case is key for timely diagnosis and management in order to prevent the most common obstetrical emergency and the leading cause of death in early pregnancy.6 The morbidity and mortality of cornual ectopic pregnancy is directly related to the length of gestational age and this type of pregnancy in particular can be discovered with advanced gestational age even up to 16 weeks due to the adjacent supporting myometrial walls and good blood supply, particularly that coming from the uterine artery.6,7 The mortality rate for all ectopic pregnancies is roughly 9% to 14% and for this, it is considered a leading cause of death in the first trimester of pregnancy. The diagnosis of the cornual ectopic pregnancy is usually delayed as this part of the tube has good muscular and vascular support which results in good distensibility and thus causing less pain. Similar to other types of ectopic pregnancies, the risk factors for cornual ectopic pregnancy include previous pelvic inflammatory disease, previous pelvic surgery, uterine anomalies, the use of assisted reproductive techniques, and previous ipsilateral salpingectomy,8 but none of these risk factors were present in the above mentioned patient.
In the case presented herein, the patient of 40 years of age presented early in pregnancy with gestational age of about 7-8 weeks complaining of mild lower abdominal pain and vaginal spotting, which can be considered as earlier presentation of cornual ectopic pregnancy. The second important fact is the beta subunit of human chorionic gonadotropin level which is considered low in comparison with the gestational age. This can be explained by separation of the gestational sac in spite of the finding of intact cornual ectopic pregnancy later on during laparotomy. The repeated values of beta subunit of human chorionic gonadotropin show decreased levels with plateau which increase the suspicion of cornual ectopic pregnancy. This is then confirmed by diagnostic laparoscopy and treated by cornual wedge resection through laparotomy which is considered to be the standard treatment for cornual ectopic pregnancy.6 After evacuation of its contents, the patient is discharged on the second postoperative day in good general condition and followed up until the beta subunit of human chorionic gonadotropin levels return back to normal.
The treatment options for cornual ectopic pregnancy include laparotomy (as in this case), laparoscopic cornual resection or cornuostomy, and conservative treatment which include the use of methotrexate, either locally at the site of ectopic or systemically as single intramuscular injection. The first method can be achieved by laparoscopic injection of methotrexate at the site of cornual ectopic at a dose of around 1-1.5 mg/kg with securing of hemostasis.9 The conservative treatment is selected if the patient is hemodynamically stable, the beta subunit of human chorionic gonadotropin value is less than 5000 mIU/mL, gestational age less than 6 weeks, absent heart activity in the gestational sac, adnexal mass less ≤4 cm and the amount of hemoperitoneum is less than 100 mL.10 The success rate of this method is approximately 65% with the advantage of preserving the tube and avoiding the required surgery with no major side effects.10 The patient treated by this method is usually followed up by serial quantative levels of beta subunit of human chorionic gonadotropin, complete blood count and liver function test, as well as transvaginal ultrasound.
Conclusion
Overall, cornual ectopic pregnancy is one of the most dangerous type of ectopic pregnancies with high maternal mortality. The availability of high resolution ultrasound, serial quantative beta subunit of human chorionic gonadotropin levels with high index of suspicion are essential for the diagnosis which is confirmed by diagnostic laparoscopy and treated by cornual wedge resection.
Acknowledgements
The author reported no conflict of interest and no funding was received for this work.
References
1. Beck WW. Ectopic pregnancy. In: Battistini M, Beck WW, Fang J, Nanda K, Rhoa M, eds. NMobstetrics and gynecology. 4th edition. Baltimore: Williams & Wilkins, 1997: 315-24.
2. Lin EP, Bhatt S, Dogra VS. Diagnostic clues to ectopic pregnancy. Radiographics 2008 Oct;28(6):1661-1671.
3. Intapibool S. Unruptured left cornual pregnancy: case report. J Med Assoc Thai 2005 Aug;88(8):1137-1139.
4. Stewart EA, Yeh J. The fallopian tubes and ectopic pregnancy. In: Ryan KJ, Berkowitz RS, Barbieri RL, eds. Kistner’s gynecology. 6th edition. St. Louis: Mosby-Year Books, 1995: 166-86.
5. Moon HS, Choi YJ, Park YH, Kim SG. New simple endoscopic operations for interstitial pregnancies. Am J Obstet Gynecol 2000 Jan;182(1 Pt 1):114-121.
6. Troiano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology 2004 Oct;233(1):19-34.
7. Chan LY, Fok WY, Yuen PM. Pitfalls in diagnosis of interstitial pregnancy. Acta Obstet Gynecol Scand 2003 Sep;82(9):867-870.
8. Soriano D, Vicus D, Mashiach R, Schiff E, Seidman D, Goldenberg M. Laparoscopic treatment of cornual pregnancy: a series of 20 consecutive cases. Fertil Steril 2008 Sep;90(3):839-843.
9. Ross R, Lindheim SR, Olive DL, Pritts EA. Cornual gestation: a systematic literature review and two case reports of a novel treatment regimen. J Minim Invasive Gynecol 2006 Jan-Feb;13(1):74-78.
10. Dhar H, Hamdi I, Rathi B. Methotrexate treatment of ectopic pregnancy: experience at nizwa hospital with literature review. Oman Med J 2011 Mar;26(2):94-98.
|