|
Abstract
High-resolution ultrasound has been used as an important tool in the diagnosis, management and monitoring of both acute and chronic peripheral nerve injuries. According to literature, it demonstrated high sensitivity and specificity for the detection of specific pathologies and its ability to differentiate between them. Literature has been reviewed, summarizing the specific finding of such modality in various peripheral neuropathies and with a specific focus over its role in evaluation and management of traumatic peripheral neuropathies.
Keywords: Ultrasonography; Evaluation; Management; Peripheral nervous system.
Introduction
Peripheral nervous system injuries can result in multiple pathologies, with involvement of single or multiple nerve units and subsequent sensory and/or motor impairment.1 Certain biological mechanisms were involved in injuries recovery such as axonal regeneration and/or re-myelination with resultant re-innervation of the targeted organ.2 This review aim to discuss the various peripheral neuropathies with a main focus on traumatic peripheral nerve injuries elaborating the different applications of ultrasound imaging in relation to the management and clinical assessment of such injuries.
Peripheral Neuropathies: Types and Classification
Etiologies of peripheral neuropathy ranges from acute, chronic to congenital anomalies; including various systemic illnesses and idiopathic pathologies.1,3-7 Trauma is one of the most common causes of acute peripheral neuropathy.1
In a study involving 5,777 trauma patients, Noble et al.8 showed a 3% prevalence of traumatic peripheral nerve injuries that involved either upper and/or lower extremities; in which 54% required surgical intervention.8 Similarly in a retrospective study by Taylor et al, an incidence of 2% for traumatic nerve injuries in either upper or lower extremities was reported with the highest rate of such pathologies associated with crush injuries.9 A study by Seddon led to clinical identification and classification of such injuries into a three graded system (neurapraxia, axonotmesis and neurotmesis).10 This was later adapted into a five grade system by Sunderland,11 and recently has been updated to include a sixth grade; a combination of any of the five degrees of injury can be present together.12,13
Findings of High Resolution Ultrasound Imaging In Various Peripheral Neuropathies
The concept of utilizing ultrasonography to evaluate peripheral nerves dates back to Solbiati et al; in which they evaluated this modality to assess the recurrent laryngeal nerve and to diagnose its associated palsy, particularly in cases of infiltrating thyroid or parathyroid pathologies.14 Focused imaging of the nerves, which is suspected to be involved and subsequent identification of the changes in their structure or lack of continuity, has helped in selecting the most appropriate management strategy and thereby has associated with improved outcome.15-20
The study conducted by Fornage et al. had helped in the differentiation between normal versus pathological conditions of peripheral nerves. The normal appearance of the nerves (Fig. 1) was shown to have echogenic fibrillar exterior texture; whereas, the pathological conditions ranged from masses to inflammatory conditions and was linked to a hypo-echoic with distal sound enhancement as well as thickening of the nerve.21 Silvestri, et al. utilized the same concept and found that in the peripheral nerves examined, hypo-echoic areas were separated by hyper-echoic bands. On histological examination, they showed that the hypo-echoic areas corresponded to the neuronal fascicles. This pattern was essential to differentiate the nerves from the surrounding tendons.22
Further analysis of the sonographic imaging has aided better delineation of the peripheral nerves, demonstrating that the echogenic appearance of peripheral nerves lies between that of the corresponding muscle and tendon with muscles having more hypo-echoic appearance relative to peripheral nerves. This evolved to the identification of the echogenic exterior texture in longitudinal sections parallel to the axis of the nerve, whereas, cross sections produce a more reticular appearance.15
Figure 1: Cross-sectional sonographic view of normal femoral nerve showing hyperechoic echo texture with few intraneural fascicles and associated hypoechoic background.
On the other hand, Nerve enlargement has been shown to occur at an early stage of several neuropathies, suggesting a potential application of ultrasound in early diagnosis.23 A study by Beekman R et al. found that nerve enlargement at multiple sites extended to the median, ulnar, radial and brachial plexus in patients with multifocal motor neuropathy.24 Furthermore, such findings were not accompanied by any electro-physiological or clinical abnormalities.25
High-resolution sonography has been demonstrated to delineate the precise location, type and extent of post-operative complication such as hematoma or collection, in addition to enable assessment of the disease status of adjacent tissues surrounding the nerve.26
High-resolution sonography has also been shown to have utility for the evaluation of brachial plexus pathology.27 In a study of 28 patients by Graif et al, ultrasound was able to detect abnormalities in 20 patients, which the cause of these pathological changes was trauma, benign and malignant primary tumors as well as secondary tumors; or nerve injury following irradiation therapy.27
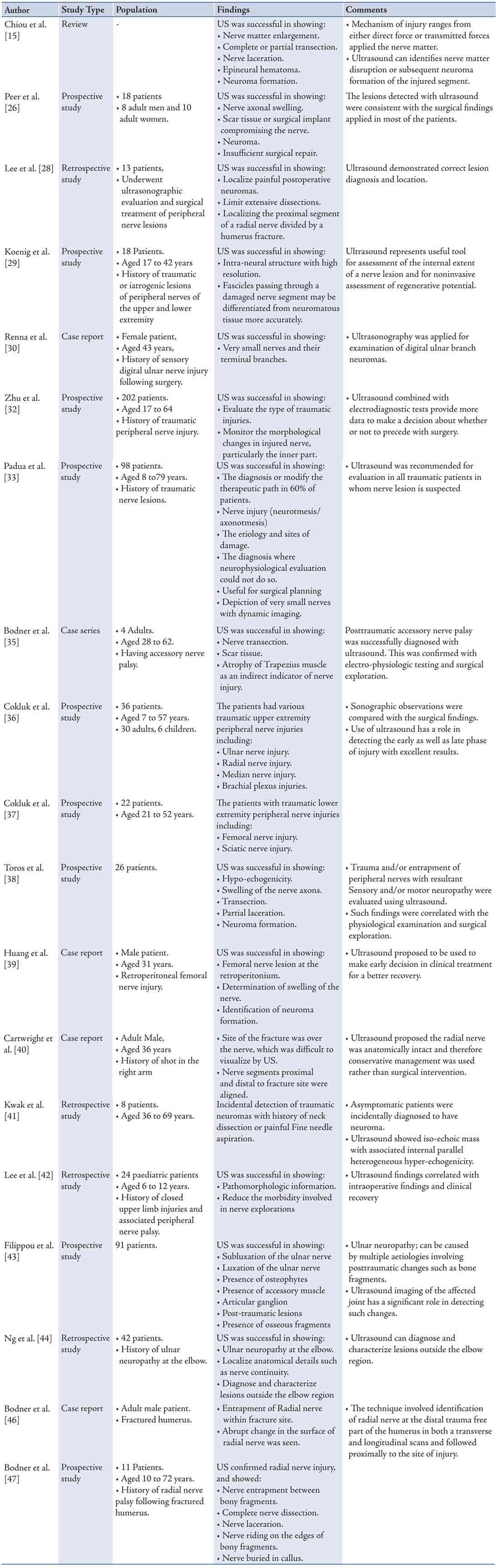
Table 1: Summarizes the relevant literature related to the use of ultrasound in the evaluation of traumatic peripheral nerve injuries.
Role of High Resolution Ultrasound Imaging In Traumatic Peripheral Neuropathies
The use of ultrasound as a diagnostic modality has aided the field of surgical intervention directed towards peripheral nerves. In particular, it has demonstrated utility for confirming and/or excluding the presence of such injury when suspected.28,29 Table 1 summarizes the pertinent literature regarding ultrasound evaluation of traumatic neuropathies.
Ultrasound examination identified a traumatic neuroma just before the ulnar nerve branched into sensory termini and excluded neurotmesis.30
The use of high-resolution ultrasound in the operative exploration and surgical identification of nervous tissue was evaluated well. Work of Lee FC, et al. have demonstrated the beneficial role of such modality in the intraoperative detection and localization of various surgical pathologies like neuromas or nerve entrapment following surgical ligation of surrounding nervous structures.28 Their work showed that the use of ultrasound have aided the exclusion of any presence of nerve injuries when other modalities of diagnosis, for example clinical, electro-physiological and/or radiological diagnoses, have failed to do so (Table. 1). Other efforts showed the essential role of high-resolution ultrasound when used intra-operatively to localize the site (intraneural and/or perineural), type, and extent of nervous injuries making the operative intervention goal oriented with less invasive and time consuming (Table. 1).29
Ultrasound is an effective tool for routine examination of peripheral nerve disorders and complemented neurophysiological assessment.31-33 This imaging modality has been successfully applied for the diagnosis of the formation of traumatic neuromas, which are non-neoplastic masses of proliferating cells that include fibroblasts, neurons and Schwann cells. Traumatic neuromas may develop because of surgical procedure or trauma (e.g; Motor vehicle accident, fall, etc.).25,26 The concept, that ultrasound could be the method of choice for diagnosing traumatic neuromas,34 was illustrated by a case report of a traumatic neuroma in an adult woman who received median nerve and associated tendon repair following a suicide attempt. Although electro-diagnostic testing was normal, ultrasonographic imaging demonstrated a hypo-echoic, focal swelling close to the median nerve that was consistent with the presence of a neuroma. Furthermore, a report of an ultrasound examination of accessory nerve lesions due to trauma in four cases, showed the feasibility of using this technique for the detection of pathological changes in the nerve following surgical procedures.35
In addition, Ultrasound was able to diagnose traumatic peripheral neuropathies from penetrating or non-penetrating causes in both the upper and lower limbs.36,37 Likewise, ultrasound examination for peripheral neuropathy of the upper limb, which caused clinically diagnosed sensory or motor deficiency, showed a number of diagnostic features including loss of nerve continuity, axonal swelling together with a hypo-echoic nerve, presence of a neuronal stump, and partial nerve severance with an absence of the normal fascicular nerve pattern; wherein surgical exploration had confirmed these diagnoses.38 The power of ultrasound imaging to diagnose traumatic neuromas is high where commonly the ultrasound show that the nerve distal to the neuroma is enlarged.39,40
In cases of fine needle aspiration biopsy, ultrasound was able to detect traumatic neuromas in the neck in the absence of any clinical signs of neuromas. It also detected an iso-echoic mass with an internal hyper-echogenic lesion, which had a heterogeneous parallel pattern.41 A retrospective analysis of 24 pediatric cases with closed upper limb injuries following bone fractures and subsequent development of peripheral nerve motor and sensory palsy, reviewed the application of ultrasound in eight of these patients. Ultrasound revealed a 50% laceration of a radial nerve in one patient and radial nerves, which were constricted and buried in fracture callus, in two other patients. Based on these sonographic findings, these three patients underwent surgery that confirmed the ultrasound diagnoses. On the basis of ultrasound assessment, a conservative management plan was followed in the other five patients. The nerves in these patients were shown to be intact; although nerves were swollen, kinked close to the fracture site, or adjacent to an orthopaedic metal screw or wire, which impaired their function. Recovery of nerve function following surgery or conservative management was observed after around 12 weeks.42
In a study by Filippou et al, high-resolution ultrasonography was found to be more useful than nerve conduction studies in localizing ulnar neuropathy, whether localized at the elbow, outside the elbow or due to previous trauma.43 There was a good correlation between ultrasonic measurement of the cross sectional area of the ulnar nerve at the sulcus and distal nerve conduction study results.44 A recent review of clinical trials addressing the application of ultrasonography in ulnar neuropathy at the elbow concluded that an increased cross sectional area of the ulnar nerve at the elbow was the most reliable parameter that was diagnostic of an abnormality.45
In other literatures, this modality was compared to other imaging techniques, where the benefits of ultrasound over MRI were shown in the diagnosis of entrapment of the radial nerve following fracture of humerus.46,47
This led to meticulous evaluation of high-resolution ultrasound together with other modalities, especially magnetic resonance imaging, in the evaluation of peripheral nerves in cases of trauma or any suspected pathology.
Conclusion
This article showed ultrasound as an extremely important tool in the diagnosis, management and monitoring of both acute and chronic peripheral nerve injury. Numerous studies in different indications have now demonstrated high sensitivity and specificity for the detection of specific pathologies and the ability to differentiate between them. Therefore, ultrasound represents a powerful tool in enabling appropriate planning for treatment, preventing unnecessary surgery where conservative management is sufficient and thus improving overall outcomes in patients with peripheral neuropathy.
Acknowledgements
This study was funded by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University.
References
1. National Institute of Neurological Disorders and Stroke (NINDS). Peripheral Neuropathy Fact Sheet. [article online] [updated September 19 cA Afhwnn.
2. Sanders VM, Jones KJ. Role of immunity in recovery from a peripheral nerve injury. J Neuroimmune Pharmacol 2006 Mar;1(1):11-19.
3. Boulton AJ, Vinik AI, Arezzo JC, Bril V, Feldman EL, Freeman R, et al; American Diabetes Association. Diabetic neuropathies: a statement by the American Diabetes Association. Diabetes Care 2005 Apr;28(4):956-962.
4. Collins M, Periquet-Collins I. Nonsystemic vasculitic neuropathy: update on diagnosis, classification, pathogenesis, and treatment. 2009.
5. Collins MP, Dyck PJ, Gronseth GS, Guillevin L, Hadden RD, Heuss D, et al; Peripheral Nerve Society. Peripheral Nerve Society Guideline on the classification, diagnosis, investigation, and immunosuppressive therapy of non-systemic vasculitic neuropathy: executive summary. J Peripher Nerv Syst 2010 Sep;15(3):176-184.
6. England JD, Gronseth GS, Franklin G, Miller RG, Asbury AK, Carter GT, et al; American Academy of Neurology; American Association of Electrodiagnostic Medicine; American Academy of Physical Medicine and Rehabilitation. Distal symmetric polyneuropathy: a definition for clinical research: report of the American Academy of Neurology, the American Association of Electrodiagnostic Medicine, and the American Academy of Physical Medicine and Rehabilitation. Neurology 2005 Jan;64(2):199-207.
7. Lewis RA, ed. Chronic inflammatory demyelinating polyneuropathy and other immune-mediated demyelinating neuropathies. Seminars in neurology; 2005: Copyright© 2005 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA.
8. Noble J, Munro CA, Prasad VS, Midha R. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma 1998 Jul;45(1):116-122.
9. Taylor CA, Braza D, Rice JB, Dillingham T. The incidence of peripheral nerve injury in extremity trauma. Am J Phys Med Rehabil 2008 May;87(5):381-385.
10. Seddon H. Three types of nerve injury. Brain 1943;66(4):237-288 .
11. Sunderland S. A classification of peripheral nerve injuries producing loss of function. Brain 1951 Dec;74(4):491-516.
12. Siemionow M, Brzezicki G. Chapter 8: Current techniques and concepts in peripheral nerve repair. Int Rev Neurobiol 2009;87:141-172.
13. Mackinnon SE. New directions in peripheral nerve surgery. Ann Plast Surg 1989 Mar;22(3):257-273.
14. Solbiati L, De Pra L, Ierace T, Bellotti E, Derchi LE. High-resolution sonography of the recurrent laryngeal nerve: anatomic and pathologic considerations. AJR Am J Roentgenol 1985 Nov;145(5):989-993.
15. Chiou H-J, Chou Y-H, Chiou S-Y, Liu J-B, Chang C-Y. Peripheral Nerve Lesions: Role of High-Resolution US1. Radiographics. 2003;23(6):e15-e.
16. Renna R. Erra C, Almeida V, Padua L. Ultrasound study shows nerve atrophy in post herpetic neuralgia. Clin Neurol Neurosurg 2012;114(10):1343-1344.
17. Martinoli C, Bianchi S, Gandolfo N, Valle M, Simonetti S, Derchi LE. US of nerve entrapments in osteofibrous tunnels of the upper and lower limbs. Radiographics 2000 Oct;20(Spec No)(suppl 1):S199-S213, discussion S213-S217.
18. Bianchi S, Montet X, Martinoli C, Bonvin F, Fasel J. High-resolution sonography of compressive neuropathies of the wrist. J Clin Ultrasound 2004 Nov-Dec;32(9):451-461.
19. Filippou G, Mondelli M, Greco G, Bertoldi I, Frediani B, Galeazzi M, et al. Ulnar neuropathy at the elbow: how frequent is the idiopathic form? An ultrasonographic study in a cohort of patients. Clin Exp Rheumatol 2010 Jan-Feb;28(1):63-67.
20. Grechenig W, Mayr J, Peicha G, Boldin C. Subluxation of the ulnar nerve in the elbow region–ultrasonographic evaluation. Acta Radiol 2003 Nov;44(6):662-664.
21. Fornage BD. Peripheral nerves of the extremities: imaging with US. Radiology 1988 Apr;167(1):179-182.
22. Silvestri E, Martinoli C, Derchi LE, Bertolotto M, Chiaramondia M, Rosenberg I. Echotexture of peripheral nerves: correlation between US and histologic findings and criteria to differentiate tendons. Radiology 1995 Oct;197(1):291-296.
23. Zaidman CM, Al-Lozi M, Pestronk A. Peripheral nerve size in normals and patients with polyneuropathy: an ultrasound study. Muscle Nerve 2009 Dec;40(6):960-966.
24. Beekman R, van den Berg LH, Franssen H, Visser LH, van Asseldonk JT, Wokke JH. Ultrasonography shows extensive nerve enlargements in multifocal motor neuropathy. Neurology 2005 Jul;65(2):305-307.
25. Chiou HJ, Chou YH, Chiou SY, Liu JB, Chang CY. Peripheral nerve lesions: role of high-resolution US. Radiographics: a review publication of the Radiological Society of North America. Inc. 2003 Nov-Dec;23(6):e15.
26. Peer S, Bodner G, Meirer R, Willeit J, Piza-Katzer H. Examination of postoperative peripheral nerve lesions with high-resolution sonography. AJR Am J Roentgenol 2001 Aug;177(2):415-419.
27. Graif M, Martinoli C, Rochkind S, Blank A, Trejo L, Weiss J, et al. Sonographic evaluation of brachial plexus pathology. Eur Radiol 2004 Feb;14(2):193-200.
28. Lee FC, Singh H, Nazarian LN, Ratliff JK. High-resolution ultrasonography in the diagnosis and intraoperative management of peripheral nerve lesions. J Neurosurg 2011 Jan;114(1):206-211.
29. Koenig RW, Schmidt TE, Heinen CP, Wirtz CR, Kretschmer T, Antoniadis G, et al. Intraoperative high-resolution ultrasound: a new technique in the management of peripheral nerve disorders. J Neurosurg 2011 Feb;114(2):514-521.
30. Renna R, Erra C, Almeida V, Padua L. Ultrasound study shows nerve atrophy in post herpetic neuralgia. Clin Neurol Neurosurg 2012 Dec;114(10):1343-1344.
31. Padua L, Liotta G, Di Pasquale A, Granata G, Pazzaglia C, Caliandro P, et al. Contribution of ultrasound in the assessment of nerve diseases. European journal of neurology: the official journal of the European Federation of Neurological Societies. 2012 Jan;19(1):47-54. PubMed PMID: 21554493.
32. Zhu J, Liu F, Li D, Shao J, Hu B. Preliminary study of the types of traumatic peripheral nerve injuries by ultrasound. Eur Radiol 2011 May;21(5):1097-1101.
33. Padua L, Di Pasquale A, Liotta G, Granata G, Pazzaglia C, Erra C, et al. Ultrasound as a useful tool in the diagnosis and management of traumatic nerve lesions. Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology. 2013 Feb 1. PubMed PMID: 23380690.
34. Chen KH, Lee KF, Hsu HC, Huang WC, Hsiao KY, Fang KM. The role of high-resolution ultrasound in the diagnosis of a traumatic neuroma in an injured median nerve. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 2009 Sep;88(9):771-4. PubMed PMID: 19692793.
35. Bodner G, Harpf C, Gardetto A, Kovacs P, Gruber H, Peer S, et al. Ultrasonography of the accessory nerve: normal and pathologic findings in cadavers and patients with iatrogenic accessory nerve palsy. Journal of ultrasound in medicine: official journal of the American Institute of Ultrasound in Medicine. 2002 Oct;21(10):1159-63. PubMed PMID: 12369671.
36. Cokluk C, Aydin K. Ultrasound examination in the surgical treatment for upper extremity peripheral nerve injuries: part I. Turk Neurosurg 2007 Oct;17(4):277-282.
37. Cokluk C, Aydin K. Ultrasound examination in the surgical treatment of lower extremity peripheral nerve injuries: part II. Turk Neurosurg 2007 Jul;17(3):197-201.
38. Toros T, Karabay N, Ozaksar K, Sugun TS, Kayalar M, Bal E. Evaluation of peripheral nerves of the upper limb with ultrasonography: a comparison of ultrasonographic examination and the intra-operative findings. J Bone Joint Surg Br 2009 Jun;91(6):762-765.
39. Huang Y, Zhu J, Liu F. Ultrasound in diagnosis of retroperitoneal femoral nerve injury: a case report. J Plast Reconstr Aesthet Surg 2013 Feb;66(2):e50-e52.
40. Cartwright MS, Yoon JS, Lee KH, Deal N, Walker FO. Diagnostic ultrasound for traumatic radial neuropathy. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 2011 Apr;90(4):342-3. PubMed PMID: 20531154. Pubmed Central PMCID: 2964388.
41. Kwak JY, Kim EK, Kim MJ, Son E. Sonographic features of traumatic neuromas after neck dissection. J Clin Ultrasound 2009 May;37(4):189-193.
42. Lee J, Bidwell T, Metcalfe R. Ultrasound in pediatric peripheral nerve injuries: can this affect our surgical decision making? A preliminary report. J Pediatr Orthop 2013 Mar;33(2):152-158.
43. Filippou G, Mondelli M, Greco G, Bertoldi I, Frediani B, Galeazzi M, et al. Ulnar neuropathy at the elbow: how frequent is the idiopathic form? An ultrasonographic study in a cohort of patients. Clin Exp Rheumatol 2010 Jan-Feb;28(1):63-67.
44. Ng ES, Vijayan J, Therimadasamy AK, Tan TC, Chan YC, Lim A, et al. High resolution ultrasonography in the diagnosis of ulnar nerve lesions with particular reference to post-traumatic lesions and sites outside the elbow. Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology. 2011 Jan;122(1):188-93. PubMed PMID: 20541969.
45. Beekman R, Visser LH, Verhagen WI. Ultrasonography in ulnar neuropathy at the elbow: a critical review. Muscle Nerve 2011 May;43(5):627-635.
46. Bodner G, Huber B, Schwabegger A, Lutz M, Waldenberger P. Sonographic detection of radial nerve entrapment within a humerus fracture. Journal of ultrasound in medicine: official journal of the American Institute of Ultrasound in Medicine. 1999 Oct;18(10):703-6. PubMed PMID: 10511303.
47. Bodner G, Buchberger W, Schocke M, Bale R, Huber B, Harpf C, et al. Radial nerve palsy associated with humeral shaft fracture: evaluation with US–initial experience. Radiology 2001 Jun;219(3):811-816.
|