|
Abstract
Objective: To describe the epidemiology of acute pancreatitis in a tertiary care center in Oman.
Methods: A retrospective study evaluated all adults (>18 yrs) who presented with first attack of acute pancreatitis to SQUH from 1st of January 2006 to 31st of December 2012.
Results: One hundred seventy-four patients were found. The mean age of the cohort was 44 ± 11 years. 54% (n=95) were male and 45% (n=79) were female. Majority of the cases were mild (n=131) compared to moderate (n=29) and severe (n=14). Sixty six percent (n=116) of the cases were secondary to alcohol and biliary tract diseases. Alcoholic pancreatitis occurred in 53% of the males whereas biliary pancreatitis occurred in 51% of the females. Pancreatitis recurred in 40% (n=71) of the cases, especially in alcoholic pancreatitis. 56 patients (32%) had complications, especially in the severe cases.
Conclusion: The data about acute pancreatitis in Oman was similar to the Western countries. Pancreatitis occurred in males more than females. Alcoholic pancreatitis was more common in males, whereas biliary pancreatitis was more common in females. Alcoholic pancreatitis re-occurred in nearly half of the cases. Severe cases were associated with more complications and recurrence.
Keywords: Acute Pancreatitis; Oman.
Introduction
Acute pancreatitis is an inflammatory process that occurs acutely in the pancreatic tissue. It is believed to occur as a result of intra-pancreatic activation and auto-digestion of the pancreases by the pancreatic enzymes.1,2 Although the majority of these attacks are mild, where the patient recovers within seven days, about 20% are severe and can end up with severe consequences.3
Various studies reported incidence of acute pancreatitis ranging from 10 to 50/100,000 population per anum in Europe, while the incidence in the USA is ranging from 17 to 30/100,000 population per annum.4 Despite being a well-known disease, there are very few reports of acute pancreatitis from the Middle East.
To date, there are no available data about the pattern and incidence of acute pancreatitis in Oman. Hence, we assessed the pattern of acute pancreatitis in a tertiary care center in Oman.
Methods
This is a retrospective study, which was conducted from January 1, 2006 until December 31, 2012 at SQUH. The hospital has computerized medical record for all the patients. The medical record numbers of all the patients who presented with acute pancreatitis were obtained electronically.
Inclusion criteria consisted of the diagnosis of acute pancreatitis, which was based on clinical features and an elevated serum amylase level of more than 300 or an elevated serum lipase more than 2-3 times from baseline. Exclusion criteria comprised of the age <18yrs, chronic pancreatitis, congenital anomalies of pancreas, pancreatic cancer, cirrhosis and patient with cystic fibrosis. Demographic data on age and sex were obtained. The clinical progress and biochemical data during the course of the attack were studied together with the management and outcome. Laboratory data were analyzed in relation to the severity of the acute occurrence according to Ranson’s criteria.5 The occurrence was considered severe in three or more of the parameters were presented during the first 48 hours of admission.
Descriptive statistics were used to describe the data. The analysis was performed using the SPSS statistical program version 20 (SPSS for Windows, Rel. 20.0.0. 2011. Armonk, NY: SPSS Inc) for categorical variables, frequencies and percentages reported.
Results
The total number of patients with acute pancreatitis during the study period was 174 (93 of them were males, 55%, and 81 were females, 45%). The age ranged between 18-93 years with the mean age of 47. The cases were divided into 4 age groups (group 1: 18-29 years, group 2: 30-44 years, group 3: 45-59 years and group 4 ≥60 years) and the frequency of acute pancreatitis was 40% in group 1, 72% in group 2, 35% in group 3 and 31% in group 4. According to Ranson’s criteria, 89% of the patients had mild-moderate attack, while only 11% had severe course of the disease. There was no statistical difference between the gender and severity of acute pancreatitis. The etiology of acute pancreatitis in 66% of the cases was secondary to alcohol and biliary tree disease. Whereas it was unknown in 21% of the cases, and the remaining 12% were secondary to: hyperlipidemia, post cholecystectomy, drugs (azathioprine, HAART), hypercalcemia, post ERCP, viral, SLE and trauma. (Figure 1 and table 1)
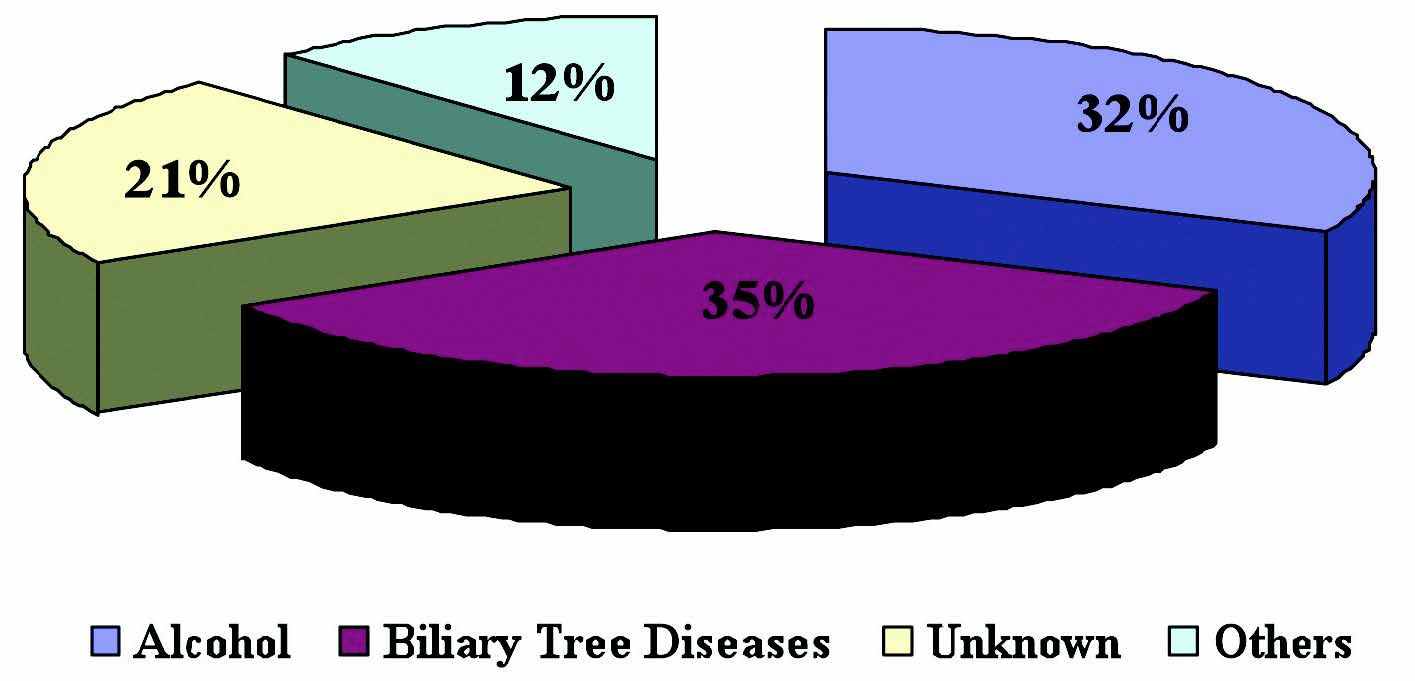
Figure 1: Causes of Acute Pancreatitis.
Table 1: Other Causes of Acute Pancreatitis.
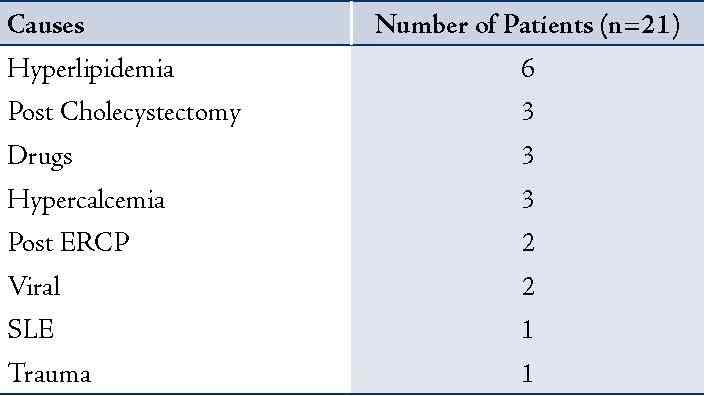
It is important to mention that despite the variety in the causes of acute pancreatitis, this didn’t influence the severity of the disease. The following diagram (Figure 2) explains the relationship between gender and causes in detail and the most striking result is that alcohol is the most common cause of acute pancreatitis in males compared to biliary tree disease in females.
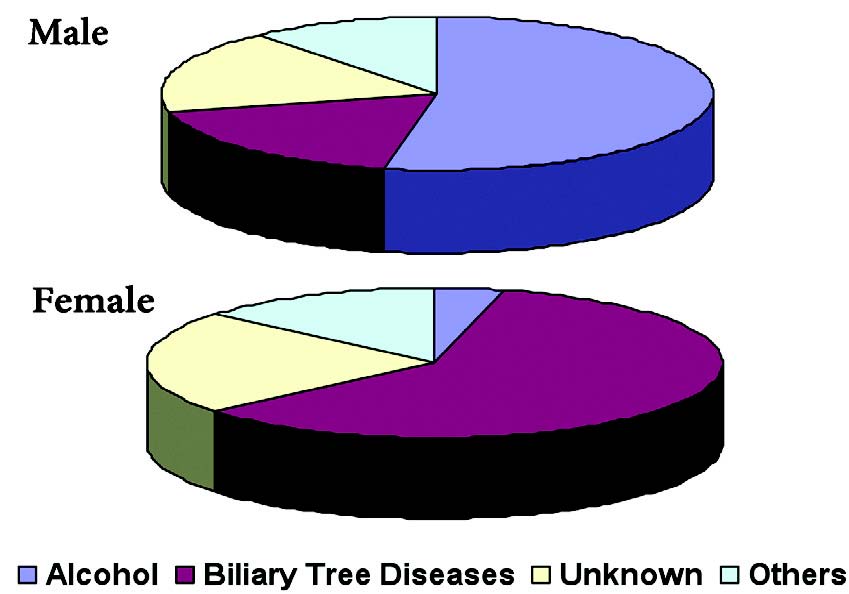
Figure 2: Causes of Acute Pancreatitis as per Gender.
Out of the 174 patients, 82 (47%) underwent CT abdomen in which 30 of them appeared to have mild acute pancreatitis as per Balthazar’s scoring, compared to the 47 patients who had mild disease as per Ranson’s criteria. On the other hand, 16 patients were labeled to have moderate disease by CT compared to 22 moderate cases as per Ranson’s critera. For the severe cases, 11 of them had severe disease by CT compared to 13 severe cases labeled as per Ranson’s criteria
There was a relapse of pancreatitis in 70 patients (40%). Those with mild, moderate and severe pancreatitis are likely to have recurrence in 45%, 37% and 64%, respectively. Further analysis was done to find the association between different causes and recurrence and this was illustrated in Figure 3. Table 2 shows the complications associated with acute pancreatitis in the 56 patients (32%).
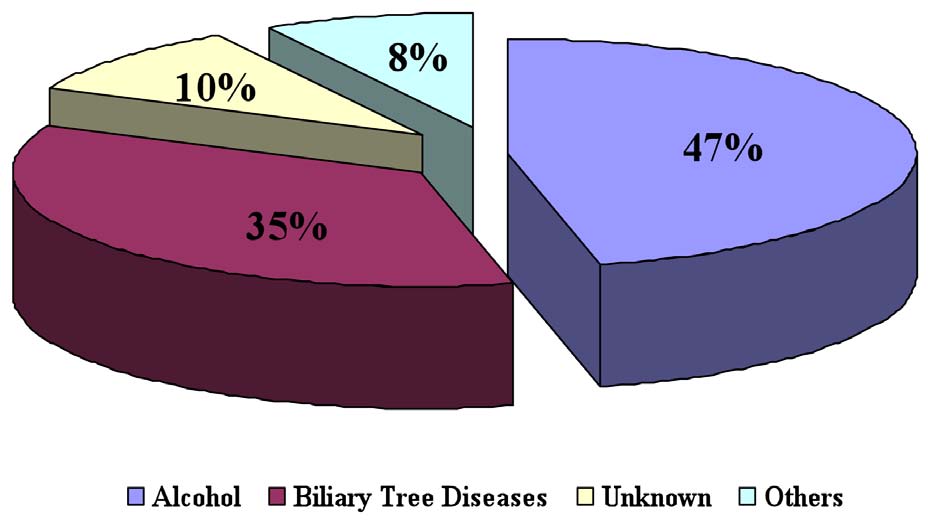
Figure 3: Recurrence of Acute Pancreatitis as per Causes
Table 2: Complications of Acute Pancreatitis.
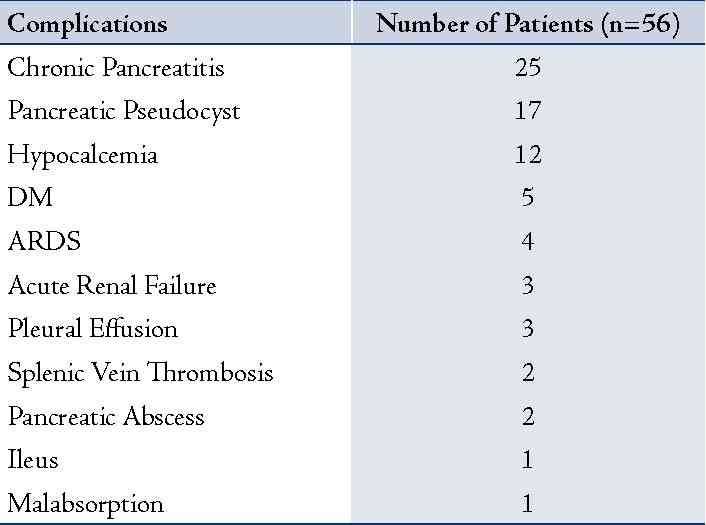
Nine out of the 14 severe cases (64%) had complications compared to 14 out of the 29 moderate cases (48%) and 33 out of the 131 mild cases (25%). Fortunately, there was no death among the 174 patients secondary to acute pancreatitis in our study.
Discussion
Acute pancreatitis is a common disease and constitutes a great medical problem in western society with morbidity of 20-30% and mortality of 8-20%.6,7,8
In the present report, it was found that acute pancreatitis is more common in males than females and can affect all ages, which was also reported in other studies.9,10 Alcohol and biliary tree disease constituted the most common causes of acute pancreatitis, whereas in 21% of the cases the cause was unknown. These findings are consistent with other reports from the western countries.11,12 We also found that alcohol was the main cause in men, while biliary tree disease was the main cause in females. It is well known that hormonal influence, especially estrogen, plays an important part in gallstones formation in females, hence increases the risk for pancreatitis.13 Then, it was inspected on whether gender had any role in the severity of the disease, but there was no significant difference with p value >0.050 and this is similar to a previous study published by Lankisch PG etl.9 In addition, causes of acute pancreatitis didn’t influence the severity of the disease. The later relationship was not fully explored or investigated in previous studies.
As per the revised Atlanta classification of acute pancreatitis,14 acute pancreatitis was defined clinically when at least 2 out of 3 features are encountered: (a) abdominal pain suggestive of pancreatitis (pain in the epigastric area which often radiates to the back), with the beginning of such pain considered to be the onset of acute pancreatitis; (b) level of serum lipase and amylase are three or more times than the normal range, (c) findings on computer tomography (CT), magnetic resonance (MR) imaging, or transabdominal ultransonographic (US) studies, which are characteristic of acute pancreatitis. There is no need for contrast material–enhanced CT if acute pancreatitis’ diagnosis is based on the first 2 diagnostic criteria with no systemic sign of severe systemic inflammatory response syndrome (SIRS) or persistent organ failure.
There is also a CT scoring system called Balthazar Scoring (CTSI), which can be used to stage the severity of the pancreatitis and to look for any necrosis, supportive or hemorrhagic pancreatitis.15 When CT diagnosis was compared with the clinical/biochemistry diagnosis of acute pancreatitis, it was found that 11 out of the 13 severe cases were correctly labeled by CT vs. 16 out of 22 moderate cases and 30 out of 47 mild cases. This shows that the use of CT is more indicated in the severe cases and its use is not recommended in the mild-moderate cases, not only because of the lower sensitivity but also to avoid unnecessary radiation.
In terms of recurrence, patients with alcohol pancreatitis had recurrence in 46% of the cases compared to the other causes and this was explored in a randomized controlled trial by Isto and colleagues for the frequent presentations of pancreatitis among alcoholic patients.16 Moreover, those patients with severe pancreatitis are more likely to have recurrence i.e. 9 out 14 (64%) compared to 37% in the mild cases.
Another major outcome of the study was the complications of acute pancreatitis. It was found that 9 out of the 14 severe cases had complications, 64% compared to 48% in the moderate cases and 25% in the mild cases. This is a logical sequence in term that severely affected patients with acute pancreatitis had more morbidities compared to mild-moderate cases. The latter was reported also by C Bassi and colleagues.17
There was no death among the 174 patients secondary to acute pancreatitis in our study and this could be attributed to many factors such as early diagnosis of the disease, prompt management and perhaps a small number of patients.
This study is not without limitations. Due to its retrospective nature, we couldn’t look at the association of antibiotic use vs. non antibiotic use in the severe cases and the outcome of that. The study was conducted in one center, so it was impossible to draw a conclusion that our study was representative of the pattern of acute pancreatitis in Oman. Another big obstacle for our study was the incorrect labeling of the diagnosis, i.e. abdominal pain was labeled as pancreatitis in many cases and sometimes there was no diagnosis written in Health Information System (HIS) of the hospital.
Conclusions
Pancreatitis affects males more than females. In males it is often related to alcohol, whereas in females it is often related to biliary tree disease. The pattern of acute pancreatitis in our study at SQUH was, to some extent, similar to the Western countries. Severe cases were associated with more complications and recurrence. Furthermore, larger prospective cohort studies are needed.
Acknowledgements
The authors declare no conflicting interest with respect to the authorship and/or publication of this article, and no funding was received on this work.
References
1. Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd ed. Saint Louis, MO: Saunders; 2009.
2. Beers MH, et al, eds. The Merck Manual of Diagnosis and Therapy. 18th ed. Whitehouse Station, NJ: Merck Research Laboratories; 2006.
3. Steinberg W, Tenner S. Acute pancreatitis. N Engl J Med 1994 Apr;330(17):1198-1210.
4. Thomson SR, Hendry WS, McFarlane GA, Davidson AI. Epidemiology and outcome of acute pancreatitis. Br J Surg 1987 May;74(5):398-401.
5. Ranson JH. Diagnostic standards for acute pancreatitis. World J Surg 1997 Feb;21(2):136-142.
6. Cortfield AP. Cooper. MJC, Williamson RCN. Acute Pancreatitis: a Lethal disease of increasing incidence. Gut 1985;26:7240-7249.
7. Jacobs ML, Daggett WM, Civette JM, Vasu MA, Lawson DW, Warshaw AL, et al. Acute pancreatitis: analysis of factors influencing survival. Ann Surg 1977 Jan;185(1):43-51.
8. Satiani B, Stone HH. Predictability of present outcome and future recurrence in acute pancreatitis. Arch Surg 1979 Jun;114(6):711-716.
9. Lankisch PG, Assmus C, Lehnick D, Maisonneuve P, Lowenfels AB. Acute pancreatitis: does gender matter? Dig Dis Sci 2001 Nov;46(11):2470-2474.
10. James H. Grendell. Acute Pancreatitis. Textbook of Internal Medicine (3rd edition) William N. Kelly 1997. Chapter. 123:793-802.
11. Wang GJ, Gao CF, Wei D, Wang C, Ding SQ. Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol 2009 Mar;15(12):1427-1430.
12. Thomson SR, Hendry WS, McFarlane GA, Davidson AI. Epidemiology and outcome of acute pancreatitis. Br J Surg 1987 May;74(5):398-401.
13. Chen A, Huminer D. The role of estrogen receptors in the development of gallstones and gallbladder cancer. Med Hypotheses 1991 Nov;36(3):259-260.
14. Sarr MG, Banks PA, Bollen TL, et al. Revision of the Atlanta classification of acute pancreatitis. Acute Pancreatitis Classification Workgroup, April 2008. http://www.pancreasclub.com/resources/AtlantaClassification.
15. Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology 2002 Jun;223(3):603-613.
16. Nordback I, Pelli H, Lappalainen-Lehto R, Järvinen S, Räty S, Sand J. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology 2009 Mar;136(3):848-855.
17. Bassi C, Falconi M, Butturini G, Pederzoli P. Early complications of severe acute pancreatitis. Surgical Treatment: Evicdence-bases and problem-oriented. Holzheimer RG, Mannick JA. 2001.
|