|
Abstract
This is a case of bilateral cavernous sinus thrombosis in a five-and-a-half-year-old boy who presented with bilateral proptosis with difficulty in swallowing and excessive salivation. Clinical features along with contrast-enhanced computed tomography and hemogram diagnosed the case as bilateral cavernous sinus thrombosis and retropharyngeal abscess with third cranial nerve palsy. The patient was treated with standard regimen successfully. Cavernous sinus thrombosis is a very rare complication of retropharyngeal abscess.
Keywords: Cavernous sinus; Retropharyngeal abscess; Thrombosis; Third nerve palsy.
Introduction
Cavernous sinus thrombosis (CST) occurs due to spread of infections from nasal furuncles (most commonly followed by sinusitis, dental abscess, orbital cellulitis, etc.). Before the availability of antimicrobial agents, mortality from CST was near 100%, but it markedly decreased to approximately 20% to 30% during the antibiotic era. Nevertheless, the threat of death and serious morbidity continues to necessitate early recognition, diagnosis, and treatment of CST to minimize risks to the patient.1 However, CST due to spread of infection from retropharyngeal abscess is very rare.
Case Report
A 5-year-6 month-old male child was admitted with history of high-grade intermittent fever in the range of 102-103ºF along with difficulty in swallowing, excessive salivation, and drowsiness for three weeks and bulging of left eye for three days and right eye for two days before admission. There was no history of seizure, facial palsy, diminished vision, or any other neurological deficit. There was no history of ear discharge, nasal furuncle, dental abscess or features suggestive of sinusitis. He had been on oral amoxicillin 50 mg/kg/day and paracetamol 15 mg/kg/dose for the past two weeks with persistence of fever and other symptoms. On admission, the child was drowsy with temperature of 104ºF. Neck stiffness and Kernig’s sign were absent. The child was found pale and malnourished. Pharynx was congested and swollen with excessive salivation and difficulty in swallowing.
There was proptosis of both eyes, right eye (RE) more than left eye (LE) with normal ocular movements and pupillary reaction. A provisional diagnosis of probable CST was made and the patient was investigated accordingly. Hemoglobin was 7.5 gm%, total count in peripheral smear was 34,900/mm3 with 66% polymorphs. Blood culture was sent. CSF examination by lumbar puncture was noncontributory. Contrast-enhanced computed tomography (CECT) of the brain and orbit revealed bilaterally dilated cavernous sinus along with enhancing hypodense lesion in retropharyngeal wall and parasellar region suggestive of CST with retropharyngeal abscess (RPA) (Fig. 1). Other investigations including blood level of protein C, protein S, antithrombin III, factor V Leiden were noncontributory. Echocardiography was normal. Intravenous vancomycin 15 mg/kg/dose IV 6 hourly for 3 weeks along with injection of dexamethasone (0.15 mg/kg/dose) were given and tapered over the next two weeks. Blood culture grew Staphylococcus aureus sensitive to vancomycin. Supportive therapy was given with IV fluids and the patient improved dramatically.
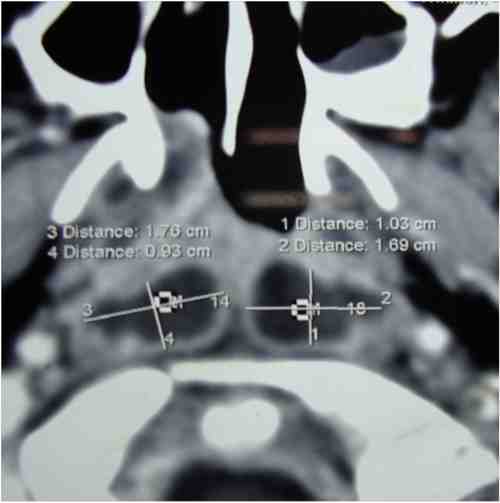
Figure 1: Showing hypodense shadow in the retrophayngeal region.
Detailed ophthalmologic evaluation was possible after one week which revealed complete recovery of proptosis in both eyes but there was ptosis of left upper eyelid along with restricted ocular movements medially and upwards causing deviation of the eye down and out. Pupil in the LE was dilated and fixed. Both consensual and direct light reflexes were present in the RE but there was no reaction to light in the LE (Fig. 2). Direct ophthalmoscopy showed normal fundi. Visual acuity was 6/6 in both eyes. A final diagnosis of CST with retropharyngeal abscess along with left 3rd nerve palsy was made. The patient was discharged after two weeks and followup was done at regular intervals. At three-month followup, there was complete recovery of ocular movements in the LE but both direct and consensual pupillary reactions were absent.

Figure 2: Left 3rd nerve palsy in a 5 year, 8 month old male child.
Discussion
CST is a rare but potentially fatal complication of dental infections, sinusitis, and orbital cellulitis. The most common causes are infections of sphenoid and ethmoid sinuses, otitis media and maxillary infections.1
The typical manifestations of CST that the patient had were bilateral exophthalmos and proptosis, chemosis, and left 3rd nerve palsy. The presentation of bilateral proptosis of the eyes is pathognomonic for CST. The cranial nerve palsies are explained by the anatomical course of these nerves as they pass through and in vicinity of the cavernous sinus. Children with RPA most commonly present with restricted neck movements, fever and cervical lymphadenopathy, and rarely with respiratory distress or stridor. The symptoms of RPA in the presented case were difficulty in swallowing and excessive salivation.
The first choice for diagnosing CST is high-resolution CT with a slice thickness of 3 mm or less,2 though MRI can be more useful for detecting complications like involvement of pituitary gland. The direct signs of CST are enlargement and expansion of cavernous sinus with lateral wall flattening or convexity, present in this case rather than normal concavity. In addition there may be multiple or single large filling defect highly suggestive of thrombus. Thus, CECT confirmed the diagnosis of both CST and RPA.
In this patient, the source of infection for the CST is retropharyngeal abscess. Retropharyngeal space is located immediately posterior to the pharynx, larynx and trachea,3 and extends superiorly to the base of the skull and inferiorly to the mediastinum at the level of tracheal bifurcation.4 The retropharyngeal space may have a communication with the cavernous sinus through a branch of veins around the internal carotid artery which drains into the internal jugular vein via the pterygoid venous plexus.5 This is supported by the fact that Eagleton demonstrated a clot in a cavernous sinus autopsy microscopically where infection progressed through the carotid venous plexus.6 The causative organism was Staphylococcus aureus which is the case in 60% to 70% of the cases. Rarer causes include Streptococcus pneumoniae, anaerobic organism as well as Aspergillus.1
The patient received the standard regimen of treatment that included intravenous sensitive antibiotics and steroids. No anticoagulants were given. According to a Cochrane review, though anticoagulant treatment for cerebral sinus thrombosis appeared to be safe and was associated with a potentially important reduction in the risk of death or dependence, evidence is limited and did not reach statistical significance.7 Although mortality following CST has been reduced following use of antibiotics, morbidity remains high and complete recovery is rare. Roughly one-sixth of patients are left with some degree of visual impairment and one-half with cranial nerve deficits. These mortality and morbidity rates may be due to delayed diagnosis without prompt surgical drainage and antibiotic administration.1
Conclusion
To conclude, the risk of CST should be considered in children with retropharyngeal abscess for early detection and prompt management of this potentially fatal complication.
Acknowledgements
Department of Pediatric Medicine and Ophthalmology and Radiology, Calcutta National Medical College and Hospital, Kolkata for helping in diagnosing & managing the case promptly.
References
1. Ebright JR, Pace MT, Niazi AF. Septic thrombosis of the cavernous sinuses. Arch Intern Med 2001 Dec;161(22):2671-2676.
2. Schuknecht B, Simmen D, Yüksel C, Valavanis A. Tributary venosinus occlusion and septic cavernous sinus thrombosis: CT and MR findings. AJNR Am J Neuroradiol 1998 Apr;19(4):617-626.
3. Page NC, Bauer EM, Lieu JE. Clinical features and treatment of retropharyngeal abscess in children. Otolaryngol Head Neck Surg 2008 Mar;138(3):300-306.
4. Wang LF, Kuo WR, Tsai SM, Huang KJ. Characterizations of life-threatening deep cervical space infections: a review of one hundred ninety-six cases. Am J Otolaryngol 2003 Mar-Apr;24(2):111-117.
5. Standring S, Collings P, Healy JC, Wigley C. Intracranial region. In: Standring S editor. Gray’s Anatomy. 40th ed.Spain: Churchil Livingstone Elsevier; 2008.p.429-430.
6. Eagleton WP. The carotid venous plexus as the path of infection in thrombophlebitis of the cavernous sinus, its relation to retropharyngeal and sphenoidal suppuration. Arch Surg 1927;15(2):275-287 .
7. Stam J, de Bruijn SFTM, deVeber G. Anticoagulation for cerebral sinus thrombosis. Cochrane Database of Systematic Reviews 2002, Issue 4. Art. No.: CD002005.
|