Peripheral intravenous (IV) cannulation is one of the most common clinical procedures performed on children. However, attempts to insert the canula are not always successful. Clinical studies indicate that only 53%–75.6% of children are successfully cannulated on the first attempt.1–5 A cross-sectional cohort study reported that IV cannulation was successful in 90% of 300 children in Brazil, regardless of the number of attempts needed, with cannulation unsuccessful in the remaining 10%.6 Furthermore, an average of two attempts was required per child to secure IV access, with successful IV cannulation potentially taking more than half an hour.7
Difficult IV access (DIVA), also known as difficult vascular access, is widely described in the literature. A panel of experts has defined DIVA as “a clinical condition in which multiple attempts and/or special interventions are anticipated or required to achieve and maintain peripheral venous access”.8 Various risk factors for DIVA in children have been reported, including patient-related, disease-related, and treatment-related factors [Table 1].8–14 Unfortunately, DIVA in children can negatively affect both the patient and his/her parents, including considerable psychological distress or pain.1,15–17 In some cases, children may experience long-term emotional consequences such as anticipatory or procedure-related distress.16–20 In addition, DIVA may also result in other negative consequences, including delays in treatment and an increased risk of IV-related complications, such as extravasation and infiltration, which subsequently increase morbidity and mortality, prolong hospital stay, and increase costs.5,21–25
Due to these potentially detrimental effects, early recognition of DIVA risk in children is an important opportunity to improve management, including decision-making regarding the value of IV access and the level of expertise needed to perform cannulation. Early recognition can also help identify children who might benefit from advanced venous visualization technologies reported to improve peripheral IV access success rates.2,22–24,26 Previous research has been conducted to develop scoring tools that improve peripheral IV access success rates, primarily focusing on DIVA risk factors and the skill level required of the healthcare provider for the successful placement of the IV cannula.8–10,12,27
In 2008, Yen et al,9 published a DIVA score tool assessing for prematurity, neonatal stay, and the visibility and palpability of the veins. During scoring, additional weight was given to younger ages (i.e., less than one year), and the absence of venous palpability and visibility as indicators of cannulation failure.9 In 2011, this scoring tool was assessed and validated with the results confirming that vein visibility, vein palpability, and age were the main variables affecting DIVA.12 The researchers excluded prematurity and history of neonatal stay from the tool as both variables were found to have no significant effect when predicting DIVA.12
To the best of the authors’ knowledge, no studies have yet been published to assess the prevalence of DIVA and associated risk factors in children in Oman or other countries in the Gulf region. Furthermore, when conducting this study, no studies were found to assess the effectiveness of existing DIVA prediction tools in Omani children. Hence, this study aimed to explore the prevalence and factors contributing to DIVA in children attending a tertiary hospital in Oman. The findings of this study were then used to develop a prediction tool to estimate the likelihood of successful IV cannulation in pediatric patients.
Methods
This cross-sectional study was conducted from September to December 2015 at Sultan Qaboos University Hospital in Muscat, Oman. This hospital has a total bed capacity of 700 beds distributed between wards and ambulatory areas. It provides unique and specialized medical services and facilities in the country, such as renal and bone marrow allogenic transplantation and a cord blood bank. An average of 12 000 children presented to the hospital’s emergency department (ED) between 2014 and 2019. When conducting this study, there were 72 pediatric inpatient beds in the hospital, excluding critical care units such as the neonatal and pediatric critical care units, with an average of 5000 admissions annually. Similarly, there were 12 beds in the pediatric day care unit (PDCU), with an average of 4000 admissions annually. In total, over 22 000 pediatric patients are treated in the hospital annually.
Peripheral cannulation is a routine nursing procedure at the hospital and is performed as needed. However, only nurses and healthcare providers who have been trained and certified for IV access are allowed to perform IV-related procedures such as phlebotomy and cannulation. Based on a retrospective data review, the prevalence of DIVA was reported to be about 25%. The necessary sample size for the current study was calculated to be 450 children with a precision of 4% and a 95% CI. However, this was increased to 500 children to adjust for dropouts and refusals to participate. Thus, a sample of children aged ≤ 18 years who required cannulation by nurses or other healthcare providers in the ED, PDCU, and pediatric inpatient wards was recruited. Only hemodynamically stable children who required cannulation and were admitted to the hospital’s ED, PDCU, and/or pediatric inpatient wards were included in the study. Children admitted to the neonatal and pediatric intensive care unit were excluded.
A data collection tool was designed based on relevant literature.1–4,6–10,12 The tool was presented to nurses experienced in pediatric care. Experienced nurses were allowed to review the tool and provide their feedback. The tool was edited accordingly until a final version was agreed. The final version of the tool consisted of five sections. The first section collected information regarding each child’s sociodemographic characteristics, including age and gender. The second section was mainly related to the child’s clinical characteristics, including diagnosis, weight, history of prematurity, history of neonatal stay, and dehydration. These data were obtained from the children’s electronic hospital records by participating nurses. However, data regarding the history of prematurity and neonatal stay were not always available in the electronic patient records; therefore, nurses asked the child’s parents for this information.
The third section was procedure-related and collected information related to the nurses’ assessment of the procedure and the child’s veins, including the number of IV access attempts, number of IV access sites identified, vein visibility, vein palpability, and the presence of vein scarring from previous IV access attempts. The fourth section assessed cooperation status with the IV access procedure on the part of children and their parents. Information in this section was also determined based on the nurses’ assessment. The fifth and final section of the data collection tool assessed information regarding the nurses’ or healthcare providers’ overall experience in nursing and specific experience with regard to
IV access.
An IV cannulation attempt was defined as the period between “when the needle first touches the skin until the needle is removed from the skin”.12 A successful attempt was defined as “an IV attempt in which a saline flush was able to be injected without compromising the vein, and the IV is secured in place, ready for use”.12 In turn, DIVA was defined as a situation in which two or more cannulation attempts were needed to secure IV access.12 The number of cannulation sites referred to the number of IV sites the nurse/health care provider was able to find, based on their physical assessment, which would lead to successful IV access. Child cooperation was determined based on the level of physical restraint required to secure IV access.28 Parent cooperation referred to the degree of cooperation with the nurse/healthcare provider exhibited by the child’s parents during the IV access procedure. The data collection tool was made available online using a Google form. Data were collected by nurses working in the ED, PDCU, and pediatric inpatient wards over the four-month study period. Approximately 150 nurses were trained in filling out the data collection tool by the principal investigator of the study. All nurses were encouraged to complete the form every time they performed an IV access procedure on a child.
Statistical analysis of the data was conducted using SPSS Statistics version 25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Collected data were examined for outliers using histograms and box plots. A chi-squared test was used to determine associations between categorical sociodemographic variables and DIVA. A p-value of < 0.30 was considered statistically significant. Subsequently, an adjusted logistic regression (multiple logistic regression) analysis was performed for significant outcome variables in the bivariate analysis. A scoring system was developed to predict the likelihood of successful IV cannulation. The odds ratios (ORs) from the multivariable analysis were used to weigh significant variables.29 Although no imputation analysis was performed for missing data, variables with > 30% missing data were not included in the analysis.
Based on their OR values, the variables of venous visibility, venous palpability, and the absence of venous scarring from previous IV access attempts were given weights of 3, 2, and 2, respectively. Child and parent cooperation were given weights of 1 each if the children and parents cooperated. Thus, for example, if the veins were visible, the likelihood of cannulation success was three times higher. Similarly, if the veins were palpable, then the opportunity for success was twice as high. The total score per child ranged from 0 to 9, with scores correlated against cannulation success. A receiver-operating characteristic (ROC) curve was drawn to determine the area under the curve (AUC) for the optimal threshold value for summative scores. According to established model-building strategies, 8–12 variables should be included in the model; however, a trade-off was necessary between the number of variables and p-values for our potential variables to be included in the model.29 Thus, five variables with p-values of < 0.30 were included.
This study was approved by the institutional ethics committee for research involving human participants. Verbal consent for the cannulation procedure based on treatment requirements was obtained by the treating physician from either the child or his/her parent or guardian. In addition, as part of their professional responsibility, the nurse or healthcare provider explained the cannulation procedure to the child and his/her parents/guardians before starting the procedure. Only children who had verbally agreed or those whose parents/guardians had verbally agreed to the cannulation procedure were included in the study. In turn, nurses’ participation in the study as data collectors was voluntary and anonymous. We considered the nurses’ completion of data in the study tool as indicative of their implied consent to participate in the study. All collected data were confidential and anonymous and used only for research purposes.
Results
A total of 511 children who underwent cannulation between September and December 2015 were included in the analysis. The majority of the children were 1–3 years old (59.2%), followed by 3–5 years (19.8%) and 5–12 years (10.9%). Few of the children were < 1 year (7.9%) or 12–18 years old (2.2%). Overall, 119 children (23.3%) underwent two or more cannulation attempts. Based on the nurses’ assessment, 91.0% of children had 0–3 access sites. Furthermore, 12.3%, 75.3%, 73.0%, and 39.9% of children were dehydrated, had visible veins, palpable veins, and vein scarring from previous IV access attempts, respectively [Table 2].
Table 1: Reported risk factors for difficult intravenous (IV) access in children according to the literature.
|
Patient-related factors8–13
|
Age
|
|
Weight
|
|
Prematurity
|
|
Fragility of the veins
|
|
Poor visibility and palpability of the veins
|
|
Location of IV attempt
|
|
Rolling, dark, or scarred veins
|
|
Race/ethnicity
|
|
Peripheral vasoconstriction
|
|
Mental/emotional status
|
|
Needle phobia and pain
|
|
Anxiety and fear
|
|
Disease-related factors8,10
|
Acute conditions
(e.g., dehydration)
|
|
Chronic illnesses (e.g., cancer)
|
|
Long-term treatment
|
Table 2: Univariate analysis of variables predicting intravenous access success among the participants (N = 511).
|
Gender
|
|
|
|
0.924
|
|
Male
|
300 (58.7)
|
230 (76.7)
|
70 (23.3)
|
|
|
Female
|
211 (41.3)
|
161 (76.3)
|
50 (23.7)
|
|
|
Age, years*
|
|
|
|
0.866
|
|
Infant (< 1)
|
40 (7.9)
|
30 (75.0)
|
10 (25.0)
|
|
|
Toddler (1–3)
|
299 (59.2)
|
232 (77.6)
|
67 (22.4)
|
|
|
Preschool (3–5)
|
100 (19.8)
|
76 (76.0)
|
24 (24.0)
|
|
|
School (5–12)
|
55 (10.9)
|
42 (76.4)
|
13 (23.6)
|
|
|
Adolescent (12–18)
|
11 (2.2)
|
7 (63.6)
|
4 (36.4)
|
|
|
Available IV access sites
|
|
|
|
|
|
0–1
|
370 (72.4)
|
280 (75.7)
|
90 (24.3)
|
-
|
|
2–3
|
95 (18.6)
|
71 (74.7)
|
24 (25.3)
|
0.212
|
|
> 3
|
46 (9.0)
|
40 (87.0)
|
6 (13.0)
|
-
|
|
History of prematurity
|
|
|
|
|
|
Yes
|
38 (7.4)
|
23 (60.5)
|
15 (39.5)
|
0.052
|
|
No
|
215 (42.1)
|
166 (77.2)
|
49 (22.8)
|
|
|
Unknown
|
258 (50.5)
|
202 (78.3)
|
56 (21.7)
|
|
|
History of neonatal stay
|
|
|
|
|
|
Yes
|
53 (10.4)
|
36 (67.9)
|
17 (32.1)
|
0.119
|
|
No
|
458 (89.6)
|
355 (77.5)
|
103 (22.5)
|
-
|
|
Underweight or overweight
|
|
|
|
|
|
Yes
|
58 (11.4)
|
37 (63.8)
|
21 (36.2)
|
0.015
|
|
No
|
453 (88.6)
|
354 (78.1)
|
99 (21.9)
|
-
|
|
Dehydration
|
|
|
|
|
|
Yes
|
63 (12.3)
|
45 (71.4)
|
18 (28.6)
|
0.309
|
|
No
|
448 (87.7)
|
346 (77.2)
|
102 (22.8)
|
-
|
|
Visibility of veins
|
|
|
|
|
|
Yes
|
385 (75.3)
|
321 (83.4)
|
64 (16.6)
|
< 0.001
|
|
No
|
126 (24.7)
|
70 (55.6)
|
56 (44.4)
|
-
|
|
Palpability of veins
|
|
|
|
|
|
Yes
|
373 (73.0)
|
312 (83.6)
|
61 (16.4)
|
< 0.001
|
|
No
|
138 (27.0)
|
79 (57.2)
|
59 (42.8)
|
-
|
|
Scars from previous IV access attempts
|
|
|
|
|
|
Yes
|
204 (39.9)
|
135 (66.2)
|
69 (33.8)
|
< 0.001
|
|
No
|
307 (60.1)
|
256 (83.4)
|
51 (16.6)
|
-
|
|
Child cooperation
|
|
|
|
|
|
Yes
|
243 (47.6)
|
199 (81.9)
|
44 (18.1)
|
0.006
|
|
No
|
268 (52.4)
|
192 (71.6)
|
76 (28.4)
|
-
|
|
Parent cooperation†
|
|
|
|
|
|
Yes
|
250 (50.2)
|
201 (80.4)
|
49 (19.6)
|
0.024
|
|
No
|
248 (49.8)
|
178 (71.8)
|
70 (28.2)
|
-
|
|
IV access experience, years‡
|
|
|
|
|
|
≤ 5
|
86 (17.0)
|
69 (80.2)
|
17 (19.8)
|
-
|
|
5.1–10
|
171 (33.8)
|
126 (73.7)
|
45 (26.3)
|
0.668
|
|
10.1–15
|
129 (25.5)
|
100 (77.5)
|
29 (22.5)
|
-
|
|
≥ 15.1
|
120 (23.7)
|
93 (77.5)
|
27 (22.5)
|
-
|
|
Overall nursing experience, years‡
|
|
|
|
|
|
≤ 5
|
88 (17.4)
|
69 (78.4)
|
19 (21.6)
|
-
|
|
5.1–10
|
173 (34.2)
|
129 (74.6)
|
44 (25.4)
|
0.857
|
|
10.1–15
|
129 (25.5)
|
101 (78.3)
|
28 (21.7)
|
-
|
IV: intravenous.
*Percentages for this variable are calculated out of 505 due to missing data. †Percentages for this variable are calculated out of 498 due to missing data. ‡Percentages for these variables are calculated out of 506 due to missing data.
Table 3: Multivariable analysis of variables predicting intravenous access success among the participants (N = 511).
|
Available IV access sites
|
|
|
|
|
0–2
|
1.09
|
0.42–2.83
|
0.861
|
|
2–3
|
0.49
|
0.18–1.33
|
0.160
|
|
> 3
|
1.00
|
-
|
-
|
|
History of neonatal stay
|
|
|
|
|
Yes
|
0.95
|
0.47–1.92
|
0.886
|
|
No
|
1.00
|
-
|
-
|
|
Underweight or overweight
|
|
|
|
|
Yes
|
0.88
|
0.46–1.70
|
0.705
|
|
No
|
1.00
|
-
|
-
|
|
Dehydration
|
|
|
|
|
Yes
|
0.74
|
0.39–1.40
|
0.35
|
|
No
|
1.00
|
-
|
-
|
|
Visibility of veins
|
|
|
|
|
Yes
|
2.72
|
1.58–4.68
|
< 0.001
|
|
No
|
1.00
|
-
|
-
|
|
Palpability of veins
|
|
|
|
|
Yes
|
2.22
|
1.29–3.83
|
0.004
|
|
No
|
1.00
|
-
|
-
|
|
Scars from previous IV access attempts
|
|
|
|
|
Yes
|
0.49
|
0.31–0.77
|
0.002
|
|
No
|
1.00
|
|
|
|
Child cooperation
|
|
|
|
|
Yes
|
1.02
|
0.62–1.69
|
0.925
|
|
No
|
1.00
|
|
|
|
Parent cooperation
|
|
|
|
|
Yes
|
1.20
|
0.75–1.93
|
0.445
|
OR: odds ratio; IV: intravenous.
Table 2 shows the univariate analyses of variables associated with successful IV cannulation. Being underweight or overweight was significantly associated with unsuccessful IV access in the univariate analysis (63.8% versus 36.2%; p = 0.015). However, this was not a statistically significant risk factor in the multivariable analysis (OR = 0.88, 95% CI: 0.46–1.70; p = 0.705). In contrast, several other risk factors remained significant in the multivariable analysis [Table 3]. Children with visible veins had a 2.7-times greater chance of successful IV access than those whose veins were not visible (OR = 2.72, 95% CI: 1.58–4.68; p < 0.001). Similarly, children whose veins were palpable had a 2.2-times greater chance of successful IV access compared to those without palpable veins (OR = 2.22, 95% CI: 1.29–3.83; p = 0.004). Finally, children with venous scarring from previous IV access attempts were half as likely to have successful IV cannulation compared to their counterparts (OR = 0.49, 95% CI: 0.31–0.77; p = 0.002).
Based on the ROC curve, the best threshold score was ≥ 7 [Figure 1]. A score of > 6 resulted in a sensitivity rate of 62.1% (95% CI: 57.1–61.0) and specificity rate of 74.2% (95% CI: 72.6–80.1) for IV cannulation success. The likelihood ratio was 2.4 (95% CI: 1.8–3.3), indicating that children who underwent successful IV cannulation were about 2.5-times more likely to score > 6. The AUC was 0.72 (p < 0.001). Positive and negative predictive values were 88.7% (95% CI: 84.3–92.4) and 37.6% (95% CI: 31.4–44.0), respectively. These findings indicated that, at this threshold, the scoring system would help identify children for whom IV cannulation success was more likely.

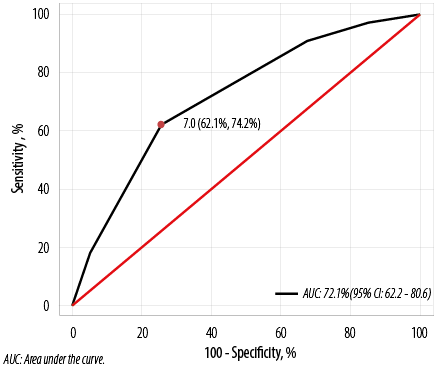 Figure 1: Receiver-operating characteristic curve for a five-variable scoring system to predict the success of intravenous access in children.
Figure 1: Receiver-operating characteristic curve for a five-variable scoring system to predict the success of intravenous access in children.
Discussion
Our study identified five factors significantly associated with DIVA in children admitted to a tertiary hospital in Oman: venous visibility, venous palpability, venous scarring from previous IV access attempts, being underweight or overweight, and child and parent cooperation status. However, only venous visibility, palpability, and the presence of venous scarring from previous IV access attempts remained statistically significant in the adjusted multivariable analysis. These findings are consistent with those reported in previous research.9,12
When conducting this study, no previous studies were found in the literature addressing venous scarring from previous IV access attempts as a factor contributing to DIVA in children. This variable was included in the present study due to its inclusion in a list of factors by an expert panel as “scarred or damaged veins”.8,10 The terminology of this variable was modified in the data collection tool utilized in the present study based on experienced nurses’ feedback to make it more understandable for nurses. Recently, the presence of “vein[s] with scars from previous IV access” has been significantly associated with failed IV access in adults, mainly patients with a history of IV drug abuse or those with chronic diseases undergoing long-term treatments such as chemotherapy.30 Therefore, the presence of this variable in children might indicate concurrent chronic illnesses requiring frequent IV treatments such as cancer or long-term treatments such as chemotherapy.
Our study noted no association between age and IV access success. This indicates that all age groups carried the same risk of DIVA. However, most children in the current study were toddlers; as such, it was difficult to analyze findings from the other age groups due to their low numbers. In contrast, age has been reported in other research to be significantly associated with DIVA, particularly for children less than one year old.9,12 Furthermore, a positive association has also been reported between older age and successful IV cannulation on the first attempt.11
The number of available IV access sites was not found to significantly affect IV success. This could be because fewer available IV access sites may have prompted nurses/healthcare providers to remain more vigilant when attempting cannulation. Similarly, no significant associations were observed between DIVA and either history of prematurity or neonatal admission; this is in contrast to other findings reported in the literature.9 However, results regarding the history of prematurity and neonatal admission might not be reliable in this study for several reasons. One reason is such data were not always available in the children’s hospital records and thus not recorded by the nurses or were based on information provided by the parents, which may have been affected by recall bias, particularly for older children.
Despite being significantly associated with unsuccessful IV cannulation in the univariate analysis, being underweight or overweight was not a statistically significant risk factor in the adjusted multivariable analysis. Being underweight or overweight has been found to significantly increase DIVA risk in previous published studies.6,8,10 This difference in findings may be because the height, weight, and body mass index of the children were not measured and recorded in this study; instead, nurses were requested to indicate if the child was underweight or overweight based on their physical assessment and the information already present in the child’s medical records. Therefore, the nurses might not have indicated if the child was underweight or overweight if this was not mentioned in the child’s hospital records or if they had not assessed the child’s weight.
Cooperation on the part of the child being cannulated is an important predictor of success in securing IV access.7 Furthermore, it has been reported that parents often show symptoms of stress and anxiety while watching their children undergo potentially distressing or painful medical procedures.31 In turn, the presence of highly anxious parents can increase the children’s anxiety and serve as a source of additional stress and distraction for inexperienced healthcare providers, thereby making the IV access process more difficult.1,31 In our study, cooperation of both the children and parents was significantly associated with successful IV access in the univariate analysis. However, these risk factors were not statistically significant in the adjusted multivariable analysis.
On the other hand, lower levels of expertise and competency of the healthcare provider inserting the cannula have been reported to significantly affect DIVA risk and contribute to the worsening of the experience for children.1,7,32 One study showed that 98% of phlebotomists, 44% of nurses, and only 23% of physicians were able to successfully secure IV access on the first attempt; the researcher concluded that phlebotomists had additional skills and experience with IV access that affected their success rates compared to nurses and physicians.33 Another study found that IV access success rates were significantly higher when the procedure was performed by nurses who rated their IV insertion skills to be high, had more experience with IV cannulation, and had more years of nursing experience.1 However, despite these correlations, other factors were reported to better predict IV access success compared to nurse experience and self-rated competency.7
The findings of our study did not support a correlation between IV access success and either overall nursing experience or specific experience with IV access. In general, almost all of the IV access attempts in the current study were performed by nurses. Therefore, no data were available to determine success rates based on profession. Furthermore, IV cannulation is considered a routine nursing procedure at the studied hospital, with all nurses certified to conduct this procedure within their first few months of employment. On the other hand, asking nurses to state their approximate years of experience with IV access procedures might not reflect their true level of expertise. Indeed, Riker et al,12 reported that they had to omit staff-related variables from their analysis due to the subjectivity of such variables.
We attempted to utilize the findings of this study to develop a successful IV cannulation prediction tool. Five variables were weighted based on their significant correlations with successful IV cannulation [Table 2]. Although some of these variables have been previously tested and weighted in other research, such risk factors might differ between populations.8,11 Based on the results of the analyses, children who had undergone successful IV access procedures were more likely to score > 6 out of a total score of 9. However, this tool still requires further testing and research to establish its validity and reliability. It has been claimed that designing an algorithm that predicts DIVA risk in children and accommodates for other variables such as the comfort of the child and the expertise of the healthcare provider accessing the vein can help reduce the number of IV attempts and more effectively meet the IV access needs of some children.34
Several limitations to this study should be acknowledged. The data were collected in a single hospital in a very populated area. Moreover, as a tertiary institution, the hospital mainly receives high-acuity patients; thus, other pediatric populations might not match the hospital’s patient population, decreasing the findings’ generalizability. Furthermore, the study tool included many variables; however, not all variables were analyzed due to missing or ambiguous data. Therefore, as previously mentioned, variables with > 30% missing data were not included in the analysis. Moreover, several nurses who participated in the study reported that completing the data collection tool was time-consuming; this may have affected compliance. Although one of the researchers periodically conducted follow-up visits to clinical areas to encourage nurses to use the tool, it is likely that some pediatric cannulation cases were not recorded. Furthermore, the researchers cannot exclude the possibility of selection bias in recording cases by nurses that might have affected findings related to the prevalence of DIVA
in this population.
Conclusion
DIVA is a fairly common occurrence and can result in negative consequences in pediatric patients. Therefore, studying the prevalence of and associated risk factors linked to DIVA among children in Oman is important to understand the extent of the problem and its contributing factors. Such findings can optimize pediatric IV access management by developing DIVA clinical care pathways and evidence-based intervention algorithms that can reduce complications and improve the quality of care provided. This study indicates that DIVA is fairly common in Omani children and is affected by certain risk factors. As such, additional strategies are needed to assess such risks to inform clinical decision-making, particularly when considering the value of attempting IV placement versus employing an alternative route of drug administration or fluid replacement. The findings of this study have been utilized to develop a DIVA prediction tool incorporating variables weighted according to their correlation with successful IV cannulation. Further research is recommended to confirm the validity of this tool.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Jacobson AF, Winslow EH. Variables influencing intravenous catheter insertion difficulty and failure: an analysis of 339 intravenous catheter insertions. Heart Lung 2005 Sep-Oct;34(5):345-359.
- 2. Davis EM, Feinsmith S, Amick AE, Sell J, McDonald V, Trinquero P, et al. Difficult intravenous access in the emergency department: performance and impact of ultrasound-guided IV insertion performed by nurses. Am J Emerg Med 2021 Aug;46:539-544.
- 3. Indarwati F, Mathew S, Munday J, Keogh S. Incidence of peripheral intravenous catheter failure and complications in paediatric patients: systematic review and meta analysis. Int J Nurs Stud 2020 Feb;102:103488.
- 4. Sabri A, Szalas J, Holmes KS, Labib L, Mussivand T. Failed attempts and improvement strategies in peripheral intravenous catheterization. Biomed Mater Eng 2013;23(1-2):93-108.
- 5. Goff DA, Larsen P, Brinkley J, Eldridge D, Newton D, Hartzog T, et al. Resource utilization and cost of inserting peripheral intravenous catheters in hospitalized children. Hosp Pediatr 2013 Jul;3(3):185-191.
- 6. de Negri DC, Avelar AF, Andreoni S, Pedreira MdaL. Predisposing factors for peripheral intravenous puncture failure in children. Rev Lat Am Enfermagem 2012 Nov-Dec;20(6):1072-1080.
- 7. Larsen P, Eldridge D, Brinkley J, Newton D, Goff D, Hartzog T, et al. Pediatric peripheral intravenous access: does nursing experience and competence really make a difference? J Infus Nurs 2010 Jul-Aug;33(4):226-235.
- 8. Kuensting LL, DeBoer S, Holleran R, Shultz BL, Steinmann RA, Venella J. Difficult venous access in children: taking control. J Emerg Nurs 2009 Sep;35(5):419-424.
- 9. Yen K, Riegert A, Gorelick MH. Derivation of the DIVA score: a clinical prediction rule for the identification of children with difficult intravenous access. Pediatr Emerg Care 2008 Mar;24(3):143-147.
- 10. Rauch D, Dowd D, Eldridge D, Mace S, Schears G, Yen K. Peripheral difficult venous access in children. Clin Pediatr (Phila) 2009 Nov;48(9):895-901.
- 11. Petroski A, Frisch A, Joseph N, Carlson JN. Predictors of difficult pediatric intravenous access in a community emergency department. J Vasc Access 2015 Nov-Dec;16(6):521-526.
- 12. Riker MW, Kennedy C, Winfrey BS, Yen K, Dowd MD. Validation and refinement of the difficult intravenous access score: a clinical prediction rule for identifying children with difficult intravenous access. Acad Emerg Med 2011 Nov;18(11):1129-1134.
- 13. Zempsky WT. Optimizing the management of peripheral venous access pain in children: evidence, impact, and implementation. Pediatrics 2008 Nov;122(Suppl 3):S121-S124.
- 14. Larsen EN, Marsh N, O’Brien C, Monteagle E, Friese C, Rickard CM. Inherent and modifiable risk factors for peripheral venous catheter failure during cancer treatment: a prospective cohort study. Support Care Cancer 2021 Mar;29(3):1487-1496.
- 15. de Freitas Floriano CM, Machado Avelar AF, Sorgini Peterlini MA. Difficulties related to peripheral intravenous access in children in an emergency room. J Infus Nurs 2018 Jan/Feb;41(1):66-72.
- 16. Fields JM, Piela NE, Ku BS. Association between multiple IV attempts and perceived pain levels in the emergency department. J Vasc Access Nov-Dec 2014;15(6):514-518.
- 17. Schott C, Brown V, Vittone S. Comfort measures for peripheral I.V. catheter placement in children. Nursing 2021 Nov;51(11):60-63.
- 18. Duff AJ. Incorporating psychological approaches into routine paediatric venepuncture. Arch Dis Child 2003 Oct;88(10):931-937.
- 19. Kennedy RM, Luhmann J, Zempsky WT. Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics 2008 Nov;122(Suppl 3):S130-S133.
- 20. Parker SI, Benzies KM, Hayden KA. A systematic review: effectiveness of pediatric peripheral intravenous catheterization strategies. J Adv Nurs 2017 Jul;73(7):1570-1582.
- 21. Cohen LL. Behavioral approaches to anxiety and pain management for pediatric venous access. Pediatrics 2008 Nov;122(Suppl 3):S134-S139.
- 22. Holder MR, Stutzman SE, Olson DM. Impact of ultrasound on short peripheral intravenous catheter placement on vein thrombosis risk. J Infus Nurs 2017 May/Jun;40(3):176-182.
- 23. Kule A, Hang B, Bahl A. Preventing the collapse of a peripheral vein during cannulation: an evaluation of various tourniquet techniques on vein compressibility. J Emerg Med 2014 May;46(5):659-666.
- 24. Liu YT, Alsaawi A, Bjornsson HM. Ultrasound-guided peripheral venous access: a systematic review of randomized-controlled trials. Eur J Emerg Med 2014 Feb;21(1):18-23.
- 25. Witting MD. IV access difficulty: incidence and delays in an urban emergency department. J Emerg Med 2012 Apr;42(4):483-487.
- 26. Katsogridakis YL, Seshadri R, Sullivan C, Waltzman ML. Veinlite transillumination in the pediatric emergency department: a therapeutic interventional trial. Pediatr Emerg Care 2008 Feb;24(2):83-88.
- 27. Angles E, Robin F, Moal B, Roy M, Sesay M, Ouattara A, et al. Pre-operative peripheral intravenous cannula insertion failure at the first attempt in adults: development of the VENSCORE predictive scale and identification of risk factors. J Clin Anesth 2021 Dec;75:110435.
- 28. Kirwan L, Coyne I. Use of restraint with hospitalized children: a survey of nurses’ perceptions of practices. J Child Health Care 2017 Mar;21(1):46-54.
- 29. Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. Hoboken: Wiley; 2013.
- 30. van Loon FH, van Hooff LW, de Boer HD, Koopman SS, Buise MP, Korsten HH, et al. The modified A-DIVA scale as a predictive tool for prospective identification of adult patients at risk of a difficult intravenous access: a multicenter validation study. J Clin Med 2019 Jan;8(2):144.
- 31. Constantin K, Moline RL, McMurtry CM, Bailey HN. Parent cardiac response in the context of their child’s completion of the cold pressor task: a pilot study. Children (Basel) 2017 Nov;4(11):100.
- 32. Parker SI, Simmons SM, Rutherford A, Caird JK, Benzies KM. Novice and expert nurses’ eye movements and success with simulated peripheral intravenous catheterization. Clin Simul Nurs 2021 Apr;53:42-48.
- 33. Frey AM. Success rates for peripheral i.v. insertion in a children’s hospital. Financial implications. J Intraven Nurs 1998 May-Jun;21(3):160-165.
- 34. Hartman JH, Baker J, Bena JF, Morrison SL, Albert NM. Pediatric vascular access peripheral IV algorithm success rate. J Pediatr Nurs 2018 Mar-Apr;39:1-6.