The first four to six weeks after delivery, known as the postpartum period, is one of the most sensitive stages of life and an important field of study in women’s reproductive health.1 Although pregnancy-induced changes and childbirth return to normal after this period, evidence suggests that many health-related problems persist for months after delivery.2,3 These include breast and nipple problems and stress related to caring for the baby,4 which sometimes have long-term effects on women’s health and quality of life.5
The COVID-19 virus has also become a stressor in the postpartum period. Acute respiratory syndrome, named COVID-19 by the World Health Organization, was initially reported in December 2019 and rapidly became a worldwide epidemic and declared a pandemic in March 2020.6 The virus can be associated with preterm delivery,7 neonatal death, and fetal asphyxia.8 The perinatal period can be associated with high levels of anxiety and depression. Telehealth was recommended to enhance healthcare at this time.9
Postpartum services are crucial for preventing unwanted maternal and neonatal outcomes.10
Caregivers’ performance and the amount of maternal environmental support are key factors for better adaptation during the postpartum period.11 In this regard, Iran’s Ministry of Health has developed a program for the postpartum period, which includes three postpartum care sessions for the mother on days 1–3, 14–15, and 42–45 after delivery. This care includes examinations, observations, questions, and necessary training on personal, mental, sexual, and oral health, warning signs, common complaints, nutrition, medication supplements, breastfeeding, neonatal care, and family planning.11 Nevertheless, postpartum care is often overlooked by health care providers and midwives compared to pregnancy, both quantitatively and qualitatively.2
Besides implementing postpartum care, attention should also be paid to the support given by significant others, such as the spouse, which can affect the mother’s quality of life and performance.11 During the COVID-19 pandemic, all pregnant mothers were advised to avoid unnecessary visits to health centers and to reduce such visits and exposure to environmental contamination, routine care for low-risk pregnant mothers was reduced from eight to four sessions by the Ministry of Health until full control of the infection.
The mother’s condition should be monitored at intervals, the results of tests and ultrasounds should be given by telephone or text message, and if necessary, the mother should be referred to related specialists.12 Despite the logical nature of this protocol for increasing pregnant mothers’ safety and ensuring their health during the postpartum period, it seemed that most of the care needs, especially the educational needs of the target group, were neglected in public health centers. Moreover, counseling and self-care training during pregnancy and the postpartum period, which met the self-care needs of mothers and infants, were overshadowed by the pandemic. On the other hand, to manage the pressures of the postpartum period and the pandemic, more social support was needed to reduce the existing stress, albeit temporarily. A qualitative study in Chile (Learning to Work While Homebound - The Effects of Remote Work) during the pandemic reported improved work performance but decreased motivation, creativity, and performance in the long term.13
Various studies have suggested strategies for optimizing postpartum care, including home visits,11 e-learning,14 feedback training,15 and internet-based training programs.16 One of the strategies to promote postpartum care is to raise awareness and improve health beliefs in the family and significant others through family-centered training,17 grandmother training,18,19 and community-based education,20 which can improve breastfeeding. Providing care for vulnerable populations is an important part of managing infectious diseases. Using simple solutions such as social networks can effectively address the mothers’ concerns.21 One of the most effective models for promoting self-care behaviors is a participatory care model introduced by Mohammadi and colleagues in 2001.22 Such care is effective in increasing men’s participation in prenatal and postpartum care23 and quality of life.24
Participatory care involves the regular and logical process of establishing effective, interactive, and dynamic communication between the mother and health-care providers for better understanding and recognizing the needs. The participation process is one of the key components of individual and family empowerment and improves the quality of life. Participatory care consists of four stages: motivation, preparation, involvement, and evaluation, ranging from self-care to professional care, in which family members, service providers, and health care workers participate, and it ultimately improves health and quality of life.22 In participatory care, contrary to the traditional approach, the focus is not on the service provider as the main factor of care, but on the combined and balanced role of all effective people, including the mother, spouse, and friends.23
Based on the available knowledge, the impact of this model on the quality of life and performance of women in the postpartum period has not been studied. Also, because of the large population covered by government centers in the country, the need for cost-effective and readily available care that is flexible based on the women’s socioeconomic status is felt more than ever. Therefore, considering the need for implementing interventions to promote the health and quality of life of women in the critical postpartum period, especially during the COVID-19 pandemic, we aimed to assess the effect of an approach based on the participatory care model on the quality of life and postpartum performance in Bojnourd, Northeastern Iran during 2020.
Methods
This study was a quasi-experimental study. We randomly selected health centers into intervention and standard care groups. We used non-probability sampling and convenience sampling. For this purpose, all mothers who were eligible for the study entered to reach a sufficient sample size in each center. The study was conducted semi-experimentally on nulliparous pregnant women in the third trimester of pregnancy living in Bojnourd city, North Khorasan Province, Iran. Bojnourd city had a population of 334 000 in 2016 and the total fertility rate in North Khorasan Province was 2.4,25 the second-highest fertility rate in the country.26 Therefore, since we aimed to test the participatory model on quality of life and self-care during the postpartum period, we used the participation of the spouse and key supporter. For this reason, the inclusion criteria were as follows: singleton pregnancy, literacy in Persian, absence of known medical and obstetric disorders in pregnancy, having electronic messengers and internet access, and the presence of the husband and a supporter in the participatory training sessions. The exclusion criteria were: the spouse or the supporter not accompanying the women during the study, infant death, preterm delivery, divorce, and relocation of the city of residence.
The sample size was estimated at 200 pregnant women with a husband and a key supporter using the formula for comparing the means in each group
α = 0.05, Zβ = 0.84, effect size = 0.3. The minimum sample required 89 mothers. The sample size in each group was estimated to be 100 people taking into account 10% sample loss.
Sampling was done in several stages so that at first health centers in Bojnourd city were divided into high and low socioeconomic classes. Two centers were randomly selected from the low socioeconomic class as intervention clusters and two centers as clusters with standard care. The same procedure was performed for privileged areas. Then from within each cluster, using a quota method based on the population covered by each center, 100 people in intervention clusters and 100 people in standard care clusters were included to reach the determined sample size. The sampling period started in July 2020. Participants were followed-up until delivery and for eight weeks after by four visits until February 2021.
The researcher-made demographic and obstetrics questionnaire had 21 items on the most important information needed about the couples and key supporters. It was validated using face and content validity and by receiving the opinions of 10 experts.
The questionnaire on quality of life after childbirth is a validated questionnaire that has been used in various studies14,27,28 with 30 items in eight domains: mother’s feelings toward herself, mother’s feelings toward her child, mother’s feelings toward her husband and others, mother’s feelings about sex, physical health status, the relationship between childbirth and economic status, maternal satisfaction with the mode of delivery, and her choice about future deliveries. The items were scored on a five-point Likert scale ranging from 30 to 150. A higher score indicates a better quality of life. The validity of this questionnaire has been previously determined and confirmed in several studies using content validity.27,28 In the present study, the reliability of the questionnaire was assessed by internal consistency (Cronbach’s alpha: 0.84) and test-retest method, and calculating the correlation coefficient and intra-cluster correlation index (ICC) between two test times, which was 0.93.
The researcher-made questionnaire on mothers’ performance in the field of self-care and infant care was compiled with the help of the postpartum lifestyle awareness and belief questionnaire and postpartum care knowledge and practice questionnaire, and the latest national instructions of “Integrated Maternal Health Care Protocol”10,11,29 including 24 items scored on a four-point Likert scale ranging from 24 to 96.
To check the qualitative face validity, the primary questionnaire was given to 10 specialists (reproductive health specialists, gynecologists specialists, and midwives) and three eligible mothers to participate in the research, and after making the necessary corrections, it was approved. The coefficient of each item was calculated quantitatively, and finally, because all questions scored > 1.5, none of the questions were omitted. Evaluators checked the validity of the qualitative part of the tool. In the quantitative part (considering that there were 10 people in the panel), the minimum acceptable coefficient of variation ratio was determined to be 0.62 based on the Lawshe table, and all items received the minimum score. According to the content validity index, all questions had a score of above 0.79.30,31 Also, Cronbach’s alpha coefficient for reliability was 0.91, and the ICC of this instrument, which was completed by 20 eligible women, with a one-week interval, was 0.89.
The action plan was developed based on the results of the preliminary needs assessment study of the target group based on the participatory care model.32 Initially, meetings were held with the officials and staff of Bint Al-Huda health centers and maternity hospitals, and a full explanation of the study was provided. In the next stage, the training classes were advertised by the researcher and the health centers staff in person and by phone. In addition to informing in person, the researcher contacted all eligible pregnant women who were in the third-trimester of pregnancy and asked them to talk to their spouse and a key supporter to see whether they wished to participate in the study, and included all three in the study upon their approval and informed consent.
Then, the pregnant woman, her husband, and a key supporter were asked to visit the health center together during one of the third-trimester visits to collect data. Because of the COVID-19 pandemic, in which women and their families could not hold classes in person, the first session was held online and offline after coordination with the participants. Online meetings were held by two members of the research team based in Bojnourd using the “Maternal and Neonatal Care” online system (https://homevirtualvisit.ir), which is a telemedicine system in the field of obstetrics and midwifery designed by North Khorasan University of Medical Sciences. The demographic information questionnaire and midwifery records (https://homevirtualvisit.ir), maternal performance questionnaire (self-care and infant care) (https://panel.porsall.com/Poll/Show/93574d2de1ac4b4), quality of life questionnaire in the postpartum period (https://panel.porsall.com/Poll/Show/1ba6fb3bcd53451) were designed for simultaneous use in the same system. The training session began after completing the demographic and midwifery records questionnaire using the link provided. Then, meetings were held simultaneously using the help system, in which the system link (https://www.intelligenttechnology.ir/ch/komak-nazari) was sent to pregnant women, their spouses, and key supporters, and after logging in, the content was presented to all three.
In some sessions, all three people logged in from the same system and were trained together. If one of the participants was not able to participate in a class simultaneously, the class file was uploaded at another time as a multimedia file in one of the virtual messaging applications and followed by a phone call. Pregnant women, their spouses, and key supporters were told to watch the educational video, and their questions were answered. Moreover, to gain further trust and higher cooperation rates, the researcher’s phone number was given to the participants to call at any time if they had any problems. All people became members of the virtual question and answer group. The meetings were held as follows:
The first session (motivational stage of participatory care model): a friendly relationship was established to establish trust. Then, postpartum problems were discussed in general, and the importance of the role of the spouse and key supporter in the postpartum period. Since these courses were helpful during the COVID-19 pandemic, the last 10 minutes of the session were spent on hygiene and breastfeeding in case pregnant women were infected with the virus. Discussion on these issues increased the participants’ awareness, sensitization, and motivation, which was needed to follow and continue subsequent care programs. The next steps (preparation and involvement) were designed and performed based on training and follow-up participatory visits.
The second and third sessions (participatory educational visits, preparation, and involvement stage) included two visits in the first 24 hours after delivery and the second week after delivery. All women in the study were asked to notify the researcher whenever they were admitted to the hospital for delivery. The hospital visit was coordinated when the spouse and a key supporter were present at the hospital, and they were trained at the hospital. The meeting was held online and offline during the second week after delivery. These two visits were attended by all three people (pregnant woman, spouse, and key supporter), and the duration of each session varied from 30 minutes to 100 minutes, depending on the needs of the participants.
The fourth session (follow-up participatory visit: preparation and involvement stage) was held three to four weeks after delivery and in line with previous participatory educational visits, with the presence of a pregnant woman, husband, and a key supporter. Positive and negative results were reviewed, and feedback was received from the participants.
During the intervention period, the standard care group received routine care from health centers. Women’s performance in self-care and infant care and quality of life after delivery were measured and compared in two stages (second and eighth weeks after delivery) by online questionnaires and telephone. A summary of the above intervention method is shown in Table 1.
Table 1: Summary of the data collection method.
|
Session 1 |
Online or offline training |
Motivation |
Third trimester of pregnancy |
Changes and physical, mental, and emotional needs of the mother in the postpartum period
maternal and neonatal risk factors after delivery.
Benefits of breastfeeding.
The role of the father and supporter in supporting the mother in the continuation of exclusive breastfeeding.
Adhering to health tips and breastfeeding if the mother is infected with COVID-19. |
|
Session 2 |
Bint Al-Huda Hospital in Bojnourd |
Preparation and involvement |
First day after delivery |
Time to visit the health center.
Time to screen the baby.
Mother and baby care.
Breastfeeding.
Maternal and infant danger signs.
Attention to maternal mood disorders. |
|
Session 3 |
Online or offline training |
Preparation and involvement |
7–14 days after delivery |
Mental health.
Caring for the mother and child at home. |
Data were analyzed using IBM SPSS Statistics for Windows, version 23 (IBM Corp., Armonk, N.Y., USA). According to the study’s objectives, descriptive statistics and inferential statistics (independent t-test and analysis of variance with repeated measures) were used.
The study did not have any costs for the participants. They were reassured that their information would remain confidential. This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences with the code IR. SBMU.PHNM.1398.089. Written consent was obtained from all participants, and the title of the research proposal was registered in the Iranian Clinical Trial Registration Center (IRCT20180715040477N1).
Results
The participatory care program was performed for 200 people in the intervention and standard care groups, but 12 people were excluded from the program for various reasons [Figure 1].

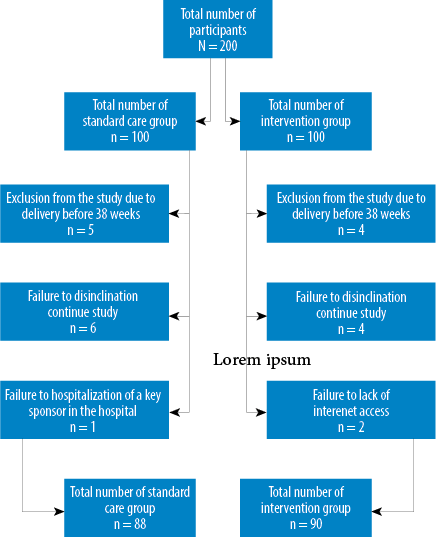 Figure 1: Flow chart for this study.
Figure 1: Flow chart for this study.
The mean ages of research participants in the intervention and standard care groups were 26.4±4.0 and 25.4±4.7 years, respectively. The two groups were homogeneous in terms of demographic and midwifery variables [Tables 2 and 3].
Table 2: Demographic characteristics of the intervention and standard care groups.
|
Mother’s age, years (mean ± SD) |
26.4 ± 4.0 |
25.4 ± 4.7 |
0.103$ |
|
key supporter’s age, years (mean ± SD) |
49.0 ± 9.4 |
51.0 ± 9.9 |
0.171$ |
|
Woman’s education, years |
|
|
0.302* |
|
0–6 |
4 (4.4) |
6 (6.8) |
|
|
7–12 |
19 (21.1) |
23 (26.2) |
|
|
>12 |
67 (74.4) |
59 (67.0) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Type of mother education |
|
|
0.564** |
|
Medical sciences |
5 (5.6) |
7 (8.0) |
|
|
Non-medical sciences |
85 (94.4) |
81 (92.0) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Woman’s occupation |
|
|
0.567** |
|
Housewife |
67 (74.4) |
69 (78.4) |
|
|
Employed |
23 (25.6) |
19 (21.6) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Spouse’s education, years |
|
|
0.124* |
|
0–6 |
1 (1.1) |
3 (3.4) |
|
|
7–12 |
31 (34.4) |
39 (44.3) |
|
|
>12 |
58 (64.4) |
46 (52.3) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Spouse’s occupation |
|
|
0.388*** |
|
Employed |
33 (36.7) |
28 (31.8) |
|
|
Manual laborer |
6 (6.7) |
11 (12.5) |
|
|
Self-employed |
51 (56.7) |
49 (55.7) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Monthly income |
|
|
0.147** |
|
Sufficient |
80 (88.9) |
71 (80.7) |
|
|
Insufficient |
10 (11.1) |
17 (19.3) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Key supporters |
|
|
0.454** |
|
Mother |
74 (82.2) |
67 (76.1) |
|
|
Other people (sister-in-law, mother-in-law, sister) |
16 (17.8) |
21 (23.9) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Key supporters’ education, years |
|
|
0.486* |
|
0–6 |
47 (52.2) |
55 (62.5) |
|
|
7–12 |
19 (21.1) |
17 (19.3) |
|
|
>12 |
24 (26.7) |
16 (18.2) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Key supporters’ occupation |
|
|
0.094** |
|
Housewife |
72 (80.0) |
79 (89.8) |
|
|
Employed |
18 (20.0) |
9 (10.2) |
|
$Independent t-test; *Mann-Whitney U test; **Fishers exact test; ***Chi-square test.
Table 3: Midwifery characteristics of the intervention and standard care groups.
|
Weeks of gestation at delivery (mean ± SD) |
39.2 ± 0.9 |
39.1 ± 1.0 |
0.889$ |
|
Neonate weight, grams (mean ± SD) |
3209.6 ± 365.3 |
3295.8 ± 365.8 |
0.113$ |
|
Neonate’s sex |
|
|
0.103* |
|
Female |
50 (55.6) |
38 (43.2) |
|
|
Male |
40 (44.4) |
50 (56.8) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Planned pregnancy |
|
|
0.079** |
|
Yes |
87 (96.7) |
79 (89.8) |
|
|
No |
3 (3.3) |
9 (10.2) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Mode of delivery |
|
|
0.325* |
|
Normal viganal delivery |
56 (62.2) |
60 (68.2) |
|
|
Cesarean section |
34 (37.8) |
28 (31.8) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Episiotomy |
|
|
0.136** |
|
Yes |
51 (91.1) |
52 (86.7) |
|
|
No |
5 (8.9) |
8 (13.3) |
|
|
Total |
56 (100) |
60 (100) |
|
|
Causes of hospitalization |
|
|
0.415* |
|
Labor pain |
34 (37.8) |
40 (45.5) |
|
|
Rupture of membranes |
13 (14.4) |
15 (17) |
|
|
Postdate (Gestational age = 40 week) |
24 (26.7) |
15 (17) |
|
|
Other cases (Decreased fetal movement, vaginal bleeding, decreased amniotic fluid index, elective cesarean section due to genital herpes, cervical myoma) |
19 (21.2) |
18 (20.5) |
|
|
Total |
90 (100) |
88 (100) |
|
|
Place of pregnancy care |
|
|
0.255* |
|
Health center |
30 (33.3) |
18 (20.5) |
|
|
Gynecologist’s office |
47 (52.2) |
52 (59.1) |
|
|
Health center and gynecologist’s office |
9 (10.0) |
12 (13.6) |
|
|
Health center, midwifery office, and gynecologist’s office |
4 (4.4) |
6 (6.8) |
|
$Independent t-test; *Chi-square test; **Fishers exact test.
The mean scores of women’s quality of life in the intervention and standard care groups were 115.5±10.9 and 114.7±11.0 two weeks after delivery and 121.0±10.6 and 116.8±12.0 eight weeks after delivery, respectively. The results of repeated-measure analysis of variance showed that there was a significant difference between the two groups (p < 0.001, Table 4, Figure 2).
Table 4: Comparison of the mean overall score and scores of the different dimensions of the postpartum quality of life in the intervention and standard care groups.
|
Overall score of postpartum quality of life |
2 weeks after delivery |
115.5 ± 10.9 |
114.7 ± 11.0 |
0.645 |
< 0.001 |
|
8 weeks after delivery |
121.0 ± 10.6 |
116.8 ± 12.0 |
0.015 |
|
|
Mother’s feelings toward herself |
2 weeks after delivery |
22.3 ± 3.1 |
22.6 ± 3.1 |
0.586 |
< 0.001 |
|
8 weeks after delivery |
23.8 ± 3.2 |
22.5 ± 3.3 |
0.009 |
|
|
Mother’s feelings toward her child |
2 weeks after delivery |
13.9 ± 1.7 |
14.2 ± 1.3 |
0.303 |
0.103 |
|
8 weeks after delivery |
14.2 ± 1.4 |
14.2 ± 1.1 |
0.883 |
|
|
Mother’s feelings toward her spouse and others |
2 weeks after delivery |
31.8 ± 4.3 |
32.2 ± 5.3 |
0.635 |
0.144 |
|
8 weeks after delivery |
32.5 ± 4.3 |
32.3 ± 5.5 |
0.797 |
|
|
Mother’s feelings toward sexual relations |
2 weeks after delivery |
9.3 ± 3.0 |
7.8 ± 2.2 |
0.001 |
0.001 |
|
8 weeks after delivery |
10.2 ± 2.8 |
7.9 ± 2.2 |
< 0.001 |
|
|
Physical health |
2 weeks after delivery |
26.2 ± 4.2 |
28.2 ± 4.4 |
0.208 |
0.982 |
|
8 weeks after delivery |
25.4 ± 4.4 |
27.4 ± 4.7 |
0.242 |
|
|
Financial status |
2 weeks after delivery |
4.6 ± 0.5 |
4.5 ± 0.8 |
0.430 |
0.221 |
|
8 weeks after delivery |
4.6 ± 0.5 |
4.5 ± 0.8 |
0.766 |
|
|
Satisfaction with delivery |
2 weeks after delivery |
3.5 ± 1.2 |
3.8 ± 1.0 |
0.081 |
0.117 |
|
8 weeks after delivery |
3.6 ± 1.2 |
3.8 ± 1.1 |
0.272 |
|
|
2 weeks after delivery |
3.5 ± 1.3 |
3.9 ± 1.1 |
0.033 |
0.179 |
*Independent t-test; **Repeated measures analysis of variance.

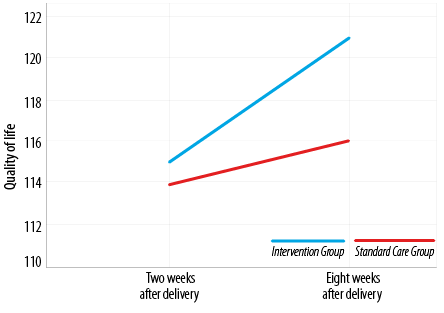 Figure 2: Changes in quality of life scores of the intervention and standard care groups in the two and eight weeks after delivery.
Figure 2: Changes in quality of life scores of the intervention and standard care groups in the two and eight weeks after delivery.
The mean general performance scores of women in the intervention and standard care groups two weeks after delivery (after presenting two training sessions in the intervention group) were 74.7±8.5 and 73.6±9.3, respectively. The corresponding scores eight weeks after delivery (after four training sessions) were 81.7±9.3 and 75.8±9.2 in the intervention and standard care groups, respectively (p = 0.428,
p < 0.001). However, the increase in the mean scores of woman’s performances in the intervention group eight weeks after delivery was more than the standard care group (p < 0.001). The results of the analysis of variance with repeated measures showed that there was a significant difference between the two groups (p <0.001, Table 5, Figure 3).

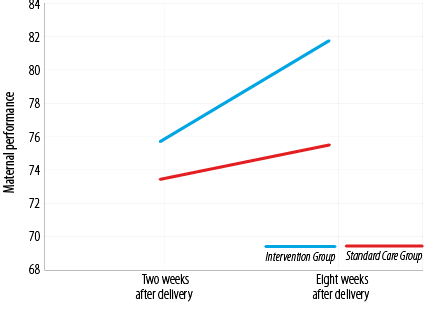 Figure 3: Changes in mothers’ performance scores in the intervention and standard care groups two and eight weeks after delivery.
Figure 3: Changes in mothers’ performance scores in the intervention and standard care groups two and eight weeks after delivery.
Table 5: Comparison of the mean overall score and scores of the different dimensions of the maternal performance in the intervention and standard care groups.
|
Overall score of maternal performance |
2 weeks after delivery |
74.7 ± 8.5 |
73.6 ± 9.3 |
0.428 |
< 0.001 |
|
8 weeks after delivery |
81.7 ± 9.3 |
75.8 ± 9.2 |
< 0.001 |
|
Maternal performance in self-care |
2 weeks after delivery |
32.5 ± 6.29 |
32.4 ± 5.2 |
0.856 |
< 0.001 |
|
8 weeks after delivery |
35.8 ± 6.92 |
33.3 ± 5.1 |
0.007 |
|
2 weeks after delivery |
42.1 ± 4.6 |
41.2 ± 5.7 |
0.253 |
*Independent t-test; **Repeated measures analysis of variance.
Discussion
The effect of the participatory model in improving women’s quality of life and performance in the field of self-care and infant care was significant compared to current methods of care. This effect showed itself more as the postpartum weeks increased. Various studies on different strategies for improving the quality of life after childbirth have shown encouraging results. One study on the use of short-term postpartum counseling sessions such as breastfeeding, immunization, child and mother care, family planning, sexual health, mental health, and lifestyle, based on the results of a women’s needs assessment, showed better quality of life after childbirth in the intervention group.33
Also, the impact of the home care program in Hainan Province in China on depressed women showed an improvement in quality of life.34 Providing self-care training based on the pattern of feedback training significantly increased women’s quality of life.14 Also, the findings of some studies showed that support programs improve the quality of life of women in the postpartum period35 and e-learning, including telephone counseling,36,37 affects the quality of postpartum life, which is consistent with our study. Although it may seem that educational interventions or home visits will always be associated with positive results, the method of instruction, its content, and compatibility of the type of care with the needs of the target group and their involvement in care programs, are critical in designing such programs for pregnant women from different social groups and are often neglected. For example, in a clinical trial in Tehran, the effect of home care on quality of life, although the quality of life scores after the intervention were higher in the intervention group; the difference between the groups was
not significant.38
Although women are expected to experience a better quality of life in the postpartum weeks with an improvement in their physical condition and regain their ability to take care of themselves, significant differences between this variable in the intervention group indicate the importance of counseling. Moreover, training key supporters are also important since they have a key role in women’s understanding of social support. However, in one study, home care did not improve the quality of life eight weeks after delivery,38 which could be attributed to the fact that the care location was moved to their house. Still, in our study, besides the care provided by the health center, caregiving training was also given in the form of a participatory care model.
In this study, training based on the participatory care model increased women’s performance in the intervention group. A study in South Korea, reviewing educational and psychological interventions during the pregnancy and postpartum period in immigrant women in 2017, showed improved self-care, infant management, and self-efficacy. Moreover, interventions involving spousal participation reported greater effectiveness.39 Two other studies in Iran on lifestyle and home care training showed improved lifestyle awareness and women’s performance in infant care.11,40
We found that the mean scores of performance and quality of life of women in the intervention group two weeks after delivery, despite a higher score, were not significantly different from the standard care group, but after eight weeks (after four sessions and counseling in the virtual group) higher and significant scores than the standard care group were seen. Such differences (improving quality of life and performance) can characterize this type of intervention in the target group. In classical studies, although the effects of educational interventions can be seen for weeks after the intervention, in the present study, the participatory nature (not only training mothers but also the husband and a key supporter) was the most important reason for the sustainability of significant effects on the desired outcomes, the effects of which were visible on quality of life structures, which makes this study unique compared with other similar studies.
One of the most important components in managing any threat of contagious diseases is caring for vulnerable populations, and pregnancy has been reported as very dangerous for many women.41 The use of simple strategies such as social media can effectively reduce the mother’s anxiety.21 Social support can reduce the anxiety induced by the COVID-19 pandemic in pregnant women.42,43 The results of a study in China showed that by reducing the perception of social support from others, the rate of postpartum depression increased,44 while the perception of support, especially spouse support,45 increased self-care behaviors. In our study, the participatory care model was associated with improved support by the spouse and key supporter in the postpartum period, increased self-care behaviors, and better women’s performance in the postpartum period.
Although the participatory care model was used for the first time to improve women’s quality of life and performance in postpartum self-care and was effective, our study had some limitations. For example, the quasi-experimental design of the study and the impossibility of randomization of participants into study groups and blinding.
Conclusion
The findings of this study showed that the use of the participatory care model was effective during the postpartum period and improved the mothers’ quality of life and performance in self-care and caring for the baby during the COVID-19 pandemic. Therefore, the design and implementation of family-centered intervention programs focusing on the health needs of individuals can be effective in increasing the understanding of women’s satisfaction and social support and promoting their health during the postpartum period.
Disclosure
The authors declared no conflicts of interest. This study was supported financially by Shahid Beheshti University of Medical Sciences. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and its later amendments.
Acknowledgements
We hereby express our gratitude and appreciation for the guidance of respected professors of the university, officials, and colleagues of health centers and Bint Al-Huda Hospital in Bojnourd and all mothers who had cooperated with the researcher to conduct this research. We also appreciate the financial support of Shahid Beheshti University of Medical Sciences.
references
- 1. Cunningham FL, Bloom S, Hauth J, Rouse D, Spong C. Williams obstetrics. 23rd ed. New York: McGraw Hill Medical Publishing; 2018.
- 2. Rouhi M, Stirling C, Ayton J, Crisp EP. Women’s help-seeking behaviours within the first twelve months after childbirth: A systematic qualitative meta-aggregation review. Midwifery 2019 May;72:39-49.
- 3. Al Subhi SK, Al Kindi RM, Al Rawahi A, Al Seyabi IS, Al Mukhaini A. Prevalence of gestational diabetes mellitus using the latest world health organization diagnostic criteria among Omani women in Muscat, Oman. Oman Med J 2021 10;36(1):e215.
- 4. Nazari S, Salari P, Mazloom S. Comparison of first and second month postpartum stress and stressors in primiparous and multiparous women. Nurs Midwifery J 2016;14(4):213-223.
- 5. Mahmoodi Z, Karimlou M, Sajjadi H, Dejman M, Vameghi M, Dolatian M. A Communicative Model of Mothers’ Lifestyles During Pregnancy with Low Birth Weight Based on Social Determinants of Health: A Path Analysis. Oman Med J 2017 Jul;32(4):306-314.
- 6. Mimouni F, Lakshminrusimha S, Pearlman SA, Raju T, Gallagher PG, Mendlovic J. Perinatal aspects on the covid-19 pandemic: a practical resource for perinatal-neonatal specialists. J Perinatol 2020 May;40(5):820-826.
- 7. Rahimi F, Goli S. Coronavirus (19) in pregnancy and childbirth: a review study. Journal of Sabzevar University of Medical Sciences 2020;27(4):522-531.
- 8. Rasmussen SA, Kelley CF, Horton JP, Jamieson DJ. Coronavirus disease 2019 (COVID-19) vaccines and pregnancy: what obstetricians need to know. Obstet Gynecol 2021 Mar;137(3):408-414.
- 9. Chen H, Selix N, Nosek M. Perinatal anxiety and depression during COVID-19. J Nurse Pract 2021 Jan;17(1):26-31.
- 10. Kamali fard M, Mirghafourvand M, Mohammad alizade charandabi S, Khodabandeh F, Asghari JafarAbadi M, Mansoori A. Effect of Lifestyle Educational Package on Prevention of Postpartum Health Problems in Nulliparous Mothers: A Randomized Clinical Trial. J Mazandaran Univ Med Sci 2016;25(132):33-48.
- 11. Mokhtari F, Bahadoran P, Baghersad Z. Effectiveness of postpartum homecare program as a new method on mothers’ knowledge about the health of the mother and the infant. Iran J Nurs Midwifery Res 2018 Jul-Aug;23(4):316-321.
- 12. Mirshekari F. The Importance of Pregnancy Care in the Covid Disease Pandemic 19. Behvarz Quarterly. 2021;32(111): 24-27,(persian).
- 13. Rebolledo OA, Vega DC, Belmar RS. Learning to work while homebound-the effects of remote work on job performance during the covid-19 pandemic. JEFMS 2021;4(6):772-793.
- 14. Duffecy J, Grekin R, Hinkel H, Gallivan N, Nelson G, O’Hara MW. A group-based online intervention to prevent postpartum depression (Sunnyside): feasibility randomized controlled trial. JMIR Ment Health 2019 May;6(5):e10778.
- 15. Ghiasvand F, Riazi H, Hajian S, Kazemi E, Firoozi A. The effect of a self-care program based on the teach back method on the postpartum quality of life. Electron Physician 2017 Apr;9(4):4180-4189.
- 16. Phelan S, Hagobian T, Brannen A, Hatley KE, Schaffner A, Muñoz-Christian K, et al. Effect of an internet-based program on weight loss for low-income postpartum women: a randomized clinical trial. JAMA 2017 Jun;317(23):2381-2391.
- 17. Heidari Z, Keshvari M, Kohan S. Clinical trial to comparison the effect of family- centered educational-supportive program on mothers’ empowerment in breast-feeding. Int J Pediatr 2016;4(3):1445-1451.
- 18. Gharaei T, Amiri Farahani L, Haghani SH, Hasanpoor-Azghady SB. The effect of the education of grandmothers on their attitude toward breastfeeding. Iran J Nurs 2019;32(119):59-69.
- 19. Bootsri W, Taneepanichskul S. Effectiveness of experiential learning with empowerment strategies and social support from grandmothers on breastfeeding among Thai adolescent mothers. Int Breastfeed J 2017 Aug;12(1):37.
- 20. Derakhshanpour F, Kashani L, Taghavi S, Salimi Z, Shahini N. Effect of a psychoeducation intervention on postpartum health. Journal of Clinical and Basic Research 2020;4(4):8-16.
- 21. Corbett GA, Milne SJ, Hehir MP, Lindow SW, O’connell MP. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol 2020 Jun;249:96-97.
- 22. Mohammadi E. Design and evaluation of collaborative care model to control high blood pressure. Thesis. Tehran, Iran: Tarbiat Modarres University; 2001.
- 23. Hajian S, Mehran N, Simbar M, Alavi Majd H. The barriers and facilitators of Iranian men’s involvement in perinatal care: a qualitative study. Reprod Health 2022 Feb;19(1):48.
- 24. Zinati F, Khashaninia Z, Rahgoi A, Rezasoltani P, Babamahmodi F. The effect of partnership caring model on quality of life of adolescents with major thalassemia. IJRN 2016;2(2):57-67.
- 25. Abbasi Z. keshavarz Z, Abbasi- Shavazi M J, Ebadi A. Factors affecting on fertility behavior from the perspective of professionals: A qualitative study. Koomesh 2019;21(1):155-163.
- 26. Mohaddes Hakkak H, Hosseini SH, Farahmand D, Rajabzadeh R, Saradj Akbari N, Sadeghi A. Investigation of the trend of vital horoscope indicator in the year following the implementation of rural family physician plan in North Khorasan Province. J North Khorasan Univ Med Sci 2018;10(1):15-20.
- 27. Bahrami N, Karimian Z, Bahrami S, Bolbolhaghighi N. Comparing the postpartum quality of life between six to eight weeks and twelve to fourteen weeks after delivery in iran. Iran Red Crescent Med J 2014 Jul;16(7):e16985.
- 28. Gharacheh M, Ranjbar F, Azadi S. Women’s quality of life and postpartum depression. IJN 2018;30(110):68-77.
- 29. Tehrani SG, Samani LN, Foroushani AR, Ebrahimi M, Karimi N. Evaluation of effect of postpartum care education based on maternal educational needs on knowledge of postpartum care. Nurs Midwifery J 2017;15(2):76-85.
- 30. Waltz C, Strickland O, Lenz E. Measurement in nursing and health research. New York: Springer Publishing; 2017.
- 31. Burns N, Susan K. Burns and Grove’s the practice of nursing research. 9th ed. Elsevier; 2021.
- 32. Nazari S, Hajian S, Abbasi Z, Majd HA. Postpartum care promotion based on maternal education needs: A mixed study. J Educ Health Promot 2021 Jul;10:261.
- 33. Esmkhani M, Ahmadi L, Maleki A. The effect of client needs counseling on the postpartum quality of life of women. J Perinat Educ 2020 Apr;29(2):95-102.
- 34. Zhuang CY, Lin SY, Cheng CJ, Chen XJ, Shi HL, Sun H, et al. Home-based nursing for improvement of quality of life and depression in patients with postpartum depression. World J Clin Cases 2020 Oct;8(20):4785-4792.
- 35. Ghodsbin F, Yazdani K, Jahanbin I, Keshavarzi S. The effect of education on health-promoting behaviors at the first six weeks post-delivery on the quality of life of primiparous women. Armaghane Danesh 2012;17(4):279-288.
- 36. Ngai FW, Wong PW, Chung KF, Leung KY. The effect of a telephone-based cognitive behavioral therapy on quality of life: a randomized controlled trial. Arch Womens Ment Health 2017 Jun;20(3):421-426.
- 37. Salehi S, Mahmoodi Z, Jashni Motlagh A, Rahimzadeh M, Ataee M. Esmaelzadeh –Saeieh S. Effect of midwife-led counseling on the quality of life of women with body image concerns during postpartum. J Holist Nurs Midwifery 2021;31(3):165-174.
- 38. Mirmolaei S, Amelvalizadeh M, Mahmoudi M, Tavakol Z. Effect of home postpartum care on quality of life of low risk mothers. Hayat (Tihran) 2011;17(2):42-51.
- 39. Kyung Kim S, Park S, Ahn S. Effectiveness of psychosocial and educational prenatal and postnatal care interventions for married immigrant women in Korea: systematic review and meta-analysis. Asia Pac J Public Health 2017 Jul;29(5):351-366.
- 40. Mirghaforvand M, Kamalifard M, Alizadeh Cherandabi S, Asghari Jafarabadi M, Khodabandeh F, Mansouri A. Effect of educational package on nulliparous mother’s knowledge and belief about postpartum lifestyle. Journal of Sabzevar University of Medical Sciences 2015;22(1):169-179.
- 41. Gausman J, Langer A. Sex and gender disparities in the COVID-19 pandemic. J Womens Health (Larchmt) 2020 Apr;29(4):465-466.
- 42. Karimi L, Makvandi S, Mahdavian M, Khalili R. Relationship between social support and anxiety caused by COVID-19 in pregnant women. Majallah-i Zanan, Mamai va Nazai-i Iran 2020;23(10):9-17.
- 43. Molgora S, Accordini M. Motherhood in the time of coronavirus: the impact of the pandemic emergency on expectant and postpartum women’s psychological well-being. Front Psychol 2020 Oct;11:567155.
- 44. Liang P, Wang Y, Shi S, Liu Y, Xiong R. Prevalence and factors associated with postpartum depression during the COVID-19 pandemic among women in Guangzhou, China: a cross-sectional study. BMC Psychiatry 2020 Nov;20(1):557.
- 45. Effati-Daryani F, Zarei S, Mohammadi A, Hemmati E, Ghasemi Yngyknd S, Mirghafourvand M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol 2020 Sep;8(1):99.