Neurofibromatosis (NF), also known as von Recklinghausen’s disease, usually involves organs of ectodermal origin—the nervous system, eyes, and skin.1 There are three known variants: neurofibromatosis type 1 (NF1), neurofibromatosis type 2 (NF2), and schwannomatosis.2 Bleeding into a NF1 lesion can occur either spontaneously or secondary to trivial trauma, and can be fatal if not diagnosed and managed expeditiously.
Case Report
A 14-year-old girl presented to our emergency department with a rapidly expanding swelling in the previously diagnosed NF1 in her left hemi-scalp/face [Figure 1]. There was no definitive history of trauma. She was alert and oriented in time, place, and person. A spontaneous bleed into the NF1 was suspected and an emergency computed tomography angiography (CTA) was performed [Figure 2]. About two hours after the presentation, the swelling suddenly increased in size, the patient became hypotensive, and the hemoglobin dropped from 11.7 g/dL to 6.6 g/dL. She was transferred to the hybrid operating room where an urgent digital subtraction angiography (DSA) was performed via a right trans-femoral artery access; meanwhile, resuscitation measures were ongoing by the anesthesia team. Following coiling of the left maxillary artery and branches [Figure 3], there was no further increase in the size of the swelling. She was discharged three days later with an appointment to see the plastic surgery team to assess the possibility of excision of the NF1.

Figure 1: Neurofibromatosis left hemi-scalp and face.

Figure 2: 3D volume-rendered CTA image reveals active arterial contrast extravasation seen as a jet of contrast (blue arrows) from left maxillary artery branch (yellow arrows). Note the significant displacement of left superficial temporal artery
(red arrow) along with galeal tissue.
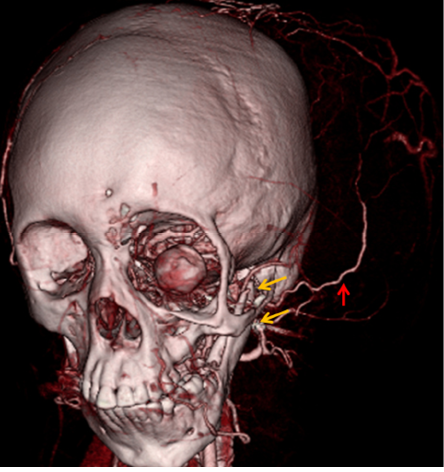
Figure 3: 3D-volume rendered CTA image acquired after angioembolization reveals the absence of active arterial contrast extravasation with metallic coils (yellow arrows) along the course of maxillary artery branch. Note the persistent displacement of left sided superficial temporal artery (red arrow) and galeal soft tissue.
Discussion
NF1 is a rare autosomal dominant neurogenic disease characterized by café-au-lait spots, pigmented hamartomas of the iris, skeletal deformities, and multiple neurofibromas. The incidence ranges from 1 in 2500–3500 individuals with about 50% having a family history of the disease. A mutation of the NF1 tumor suppressor gene located on chromosome 17q11.2 may make an individual vulnerable to development of NF1. Pathogenesis is uncertain with no sex or racial predilection. Learning disability and malignant transformation are also known to be associated with this condition.2–5 A friable vascular tree is thought to be secondary to invasion of the vessel wall by the neurofibroma or arterial dysplasia. The NF tissue itself has thin walled ectatic blood vessels which lie within the loose neural stroma that has replaced the normal adipose tissue.5 Bleeding is seen usually in the intrathoracic, gut (gastrointestinal stromal tumors), subcutaneous tissues, or less commonly in the brain or retroperitoneal tissue. Vascular lesions are usually diagnosed when patients have pain or hemorrhage which at times can be fatal.6,7
Multidimensional imagings using 3/2D ultrasound, CTA, and DSA plays a crucial role in assessing the source of bleed and planning intervention.8 Neuroimaging findings in patients with NF1 include focal areas of increased signal intensity on T-2 weighted imaging, called ‘unidentified bright objects’ and may disappear in adulthood. In 2–6% of patients with NF1, increased brain volume and abnormal cerebral vessels are also detected.9
Spontaneous hemorrhage into the NF1 lesions in the scalp, face, and skull base (as in our case) is rare. There is a need to expedite diagnosis and intervention to avoid airway compromise and prevent compression of vascular and orbital structures.10 Open surgical repair is likely to be catastrophic due to accompanying skeletal deformities.3
In our patient, the sphenoid bone was absent on the affected side. The maxillary artery was bleeding through this bony defect, compounded with the fragility of the vasculature. Hence, achieving proximal control would have been challenging with open surgery. She was shifted to the hybrid operating room and via a right transfemoral access, the left maxillary artery and its branches were successfully embolized with coils.
The hardware used for the endovascular procedure were the following: 5F arterial sheath (Radifocus, Terumo Corporation, Japan); 0.035" Hydrophilic guidewire (Radifocus, Terumo Corporation, Japan); 5F, 100 cm shaft H1 guiding catheter (Cook Medical, USA); 2.8 F, 130 cm shaft, Progreat® Microcatheter (Terumo Corporation, Japan); with 3x30 mm, 0.018’ Hilal embolization microcoils (Cook medical, Denmark).
The patient required blood transfusions during and after the procedure. At discharge, on the third post-procedure day, she was seen by the plastic surgery team for suitability of excision of the lesion, supported by the neurosurgical and vascular surgical teams.
Conclusion
NF1 is a rare disorder that can present with catastrophic bleeds due to the fragile nature of the vasculature. Urgent imaging in the form of a CTA or DSA followed by embolization procedure can
be lifesaving.
Disclosure
The authors declare no conflicts of interest. Consent was obtained from the patient’s parents.
Acknowledgements
The authors thank the patient’s parents for permitting use of the clinical picture for purposes of teaching and publication.
references
- 1. Jouhilahti EM, Peltonen S, Heape AM, Peltonen J. The pathoetiology of neurofibromatosis 1. Am J Pathol 2011 May;178(5):1932-1939.
- 2. Korf BR. Neurofibromatosis. Handb Clin Neurol 2013;111:333-340.
- 3. Qin H, Chen W, Kong J, Chen F, Wen X, Li Z, et al. Tratamiento quirúrgico de un neurofibroma masivo de cabeza y cuello en un paciente con neurofibromatosis tipo 1: reporte de un Caso. Int J Morphol 2018;36(1):194-200.
- 4. Zhu L, Shi L, Wang B, Bi M, Pu J, Zhang L, et al. Novel mutations in one allele in a Chinese family with neurofibromatosis type 1: including a complex insertion-deletion mutation. J Dermatol 2016 Nov;43(11):1332-1335.
- 5. Baek SH, Kim JH, Kim JS, Han SB, Cho JS, Yoon YH, et al. Recurrent massive subcutaneous hemorrhage in neurofibromatosis type 1: a case report. J Korean Med Sci 2007 Aug;22(4):728-730.
- 6. Moerbeek PR, van Buijtenen JM, van den Heuvel B, Hoksbergen AW. Fatal retroperitoneal bleeding caused by neurofibromatosis: a case report and review of the literature. Case Rep Med 2015;2015:965704.
- 7. Oderich GS, Sullivan TM, Bower TC, Gloviczki P, Miller DV, Babovic-Vuksanovic D, et al. Vascular abnormalities in patients with neurofibromatosis syndrome type I: clinical spectrum, management, and results. J Vasc Surg 2007 Sep;46(3):475-484.
- 8. Wortsman X, Lobos N, De la Parra R, Carreno L. Multidimensional ultrasound and computed tomography imaging support in bleeding plexiform neurofibromatosis of the scalp: A case report and literature review. Indian J Dermatol 2015 Jul-Aug;60(4):421-424.
- 9. Korf BR, Lobbous M, Metrock LK. Neurofibromatosis type1 (NF1): Pathogenesis, Clinical features, and diagnosis. June 03,2020. [Cited 2020 October 5]. Available from: https://www.uptodate.com/contents/2939#!.
- 10. Svider PF, Patel CR, Lamba S, Gandhi C, Baredes S, Jyung RW. Massive, spontaneous facial hematoma in a neurofibromatosis type 1 patient. International Journal of Otolaryngology and Head & Neck Surgery 2013;2:17-20.