A 40-year-old man with multiple comorbidities presented to the emergency department with noisy breathing. The patient had prior history of a week-long intubation for respiratory distress. According to the patient, noisy breathing was present since discharge. Upon examination, biphasic stridor was audible. He was not tachypneic or tachycardic. Flexible nasopharyngolaryngoscopy revealed normal supraglottic structures with mobile vocal cords with stenosis noted beyond subglottic region. Tracheostomy for laryngotracheal stenosis was performed under local anesthesia. Flexible bronchoscopy (FB) via tracheostomy tube revealed blind-end opening over the right side of trachea above carina [Figure 1].
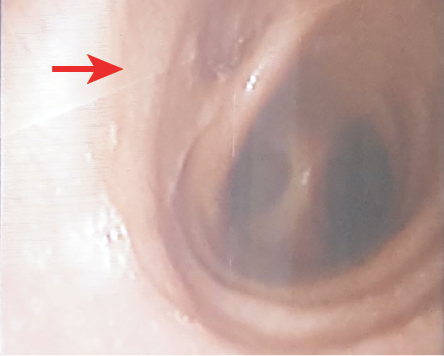
Figure 1: Flexible bronchoscopy via tracheostomy tube revealed blind-end opening over right side of trachea above the carina.
Question
1. What is your diagnosis?
a) Tracheal bronchus.
b) Tracheomalacia.
c) Tracheal stenosis.
d) Granulation tissue.
Answer
a) Tracheal bronchus.
Discussion
Tracheal bronchus or bronchus suis is a congenital aberrant bronchus commonly emerging from the right tracheal wall above carina. In general population, 0.1–2% have been reported to have this condition.1 Tracheal bronchus occurs as a result of additional tracheal outpouching which occurs in early embryonic life. This rare condition is often discovered incidentally during bronchoscopy (either rigid or flexible) and imaging.2 Tracheal stenosis is also associated with Down’s syndrome.1 Right-sided predilection has also been reported.3
Most patients remain asymptomatic, as in the present case. Some patients may present with recurrent chest infections following retained secretion and even respiratory distress. In such cases, routine intubation of tracheal bronchus may inadvertently lead to atelectasis, postoperative pneumonia, respiratory failure, or pneumothorax.3 Patients with no clinical symptoms can be managed conservatively.
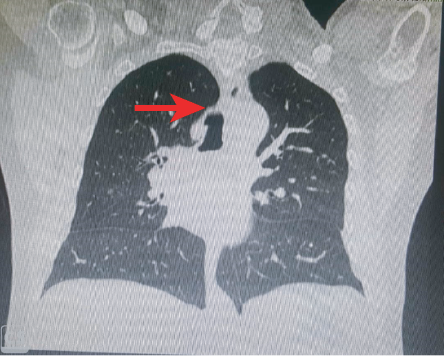
Figure 2: High resolution computed tomography of the larynx shows an outpouching lesion arising at the right lateral wall of the trachea at level T4.
FB is a powerful diagnostic tool. FB can detect tracheomalacia by the weakening or collapse or malacic nature of the tracheal wall. Tracheal stenosis may appear under FB as narrowed laryngotracheal lumen and the granulated appearance of the tissue along the laryngotracheal wall. In this case, no narrowing, weakening, or granulation of the tracheal wall tissue was noted.
Routine intubation of patients with this anomaly (as had been done previously in this patient) carries the risk of occlusion, leading to collapse of lobe, pneumothorax, and inadequate ventilation. Therefore, tracheal bronchus ought to be considered as a possible differential diagnosis in all patients, especially children, with recurrent upper lobe collapse.
The standard diagnostic procedures mentioned in this case are sufficient to diagnose tracheal bronchus. However, we also employed high-resolution computed tomography of the larynx, which gave a much clearer picture, and showed an outpouching lesion arising at the right lateral wall of the trachea at level T4 [Figure 2].
Conclusion
The tracheal bronchus is a rare but potentially dangerous congenital aberration in the bronchus. Otorhinolaryngologists need to maintain a high-index of suspicion for tracheal bronchus while intubating patients with repeated chest infections (especially children) to avoid serious complications.
Disclosure
The authors declared no conflicts of interest. Informed consent was obtained from the patient to include the diagnostic photograph for clinical training and scientific publishing.
references
- 1. Ruchonnet-Metrailler I, Abou Taam R, de Blic J. Presence of tracheal bronchus in children undergoing flexible bronchoscopy. Respir Med 2015 Jul;109(7):846-850.
- 2. Doolittle AM, Mair EA. Tracheal bronchus: classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg 2002 Mar;126(3):240-243.
- 3. Lai KM, Hsieh MH, Lam F, Chen CY, Chen TL, Chang CC. Anesthesia for patients with tracheal bronchus. Asian J Anesthesiol 2017 Dec;55(4):87-88.