Despite the wide spread of statin use in Arabian Gulf countries, patients with very high risk for atherosclerotic cardiovascular diseases (ASCVD), like diabetic patients with multiple risk factors, patients with severe familial hypercholesterolemia, and patients with established ASCVD remain at very high risk of residual cardiovascular and recurrent cardiovascular events.1–5
Several studies have demonstrated a strong association between high triglycerides (TG) and high triglyceride-rich lipoproteins (TRLs) and cardiovascular events.6–8 Non-high-density lipoprotein cholesterol (non-HDL-C) is a good measure of all atherogenic lipoproteins and defined as:
|
non-HDL-C = |
total cholesterol (TC) – HDL-C. |
Hence, regional Middle East consensus papers highly recommend the use of low-density lipoprotein cholesterol (LDL-C) in combination with non-HDL-C as primary therapeutic targets to reduce the risk of future and recurrent cardiovascular events, especially in patients with diabetes mellites (DM) and established ASCVD.9,10
We sought to estimate the achievement of the non-HDL-C target in patients with very high ASCVD risk stratified by TG levels despite statin-controlled LDL-C in the Centralized Pan-Middle East Survey on the Undertreatment of Hypercholesterolemia (CEPHEUS).
Methods
The details of this study have already been described.11 Briefly, the CEPHEUS study was a multi-center non-interventional survey of patients on lipid-lowering drugs (LLDs) in six Arabian Gulf countries (Saudi Arabia, UAE, Oman, Qatar, Bahrain, and Kuwait). A total of 5276 patients were enrolled in this survey from outpatient clinics by 177 specialists and primary care physicians. The study was conducted between 22 November 2009 and 7 July 2010. The inclusion criteria were: patients ≥ 18 years old taking LLDs for ≥ 3 months, with no dose change for a minimum of six weeks.
A fasting blood sample was taken from each subject to measure TC, HDL-C, TG, apolipoprotein A1 (apo A1), apo B, glucose, and glycated hemoglobin. LDL-C was calculated using Friedewald’s formula. Non-HDL-C was calculated using the following formula:
Blood samples were collected in three tubes (5 mL in a gel tube, 2 mL in a fluoride tube, and 2 mL in an EDTA tube). All blood samples were shipped by air courier, and the tests were performed at the King Faisal Specialist Hospital and Research Centre (Riyadh, Saudi Arabia). All the laboratory tests underwent internal and external quality control checks. In this study, we only included patients with very high ASCVD risk status (DM with major risk factors and patients with established ASCVD) defined by the European Society of Cardiology and European Atherosclerosis Society (ESC/EAS) 2019 guidelines for the management of dyslipidemia.12 These patients were further stratified into controlled LDL-C defined as < 70 mg/dL (< 1.8 mmol/L) with normal TG < 150 mg/dL (< 1.7 mmol/L) and high TG between 150–400 mg/dL (1.7–4.5 mmol/L).13 The non-HDL-C target was defined as < 100 mg/dL (< 2.6 mmol/L).13 Low HDL-C was defined < 40 mg/dL (1.0 mmol/L) for men and < 50 mg/dL (1.3 mmol/L) for women.13
Descriptive statistics were used to describe the data. For categorical variables, frequencies and percentages were reported. Differences between groups were analyzed using Pearson’s chi-squared tests (or Fisher’s exact tests for cells < 5). For continuous variables, mean and standard deviation were used to summarize the data. Analyses were performed using Student’s t-test. An a priori two-tailed level of significance was set at 0.05. Statistical analyses were conducted using STATA version 16.1 (STATA Corporation, College
Station, TX, USA).
This study complied with the Declaration of Helsinki. The study had approval from the internal review bodies/ethics committees of each participating institution in the Arabian Gulf countries. Informed written consent was also obtained from all patients enrolled in the study.
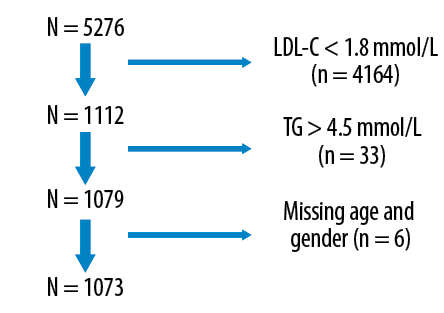
Figure 1: Schematic diagram of the patient flow of theCentralized Pan-Middle East Survey on the Undertreatment of Hypercholesterolemia study.
Results
The full CEPHEUS cohort consisted of 5276 patients. However, this study included only 1112 patients who had controlled LDL-C (< 1.8 mmol/L). Furthermore, we only recruited those with TG levels of ≤ 4.5 mmol/L (n = 1079). Six patients with missing age and gender were excluded from the analysis with the final working sample of 1073 patients [Figure 1]. The overall mean age was 58.0±11.0 years, 66.8% (n = 717) were male, 9.7% (518/1070) were smokers, and 48.4% (n = 518) had BMI ≥ 30 kg/m2. The proportion of patients that had metabolic syndrome (MetS), DM, and CAD were 31.8% (338/1064), 73.0% (n = 780), and 48.7% (n = 523), respectively. The proportion of patients with high TG levels (≥ 1.7–4.5 mmol/L) was 23.8% (n = 255).
Table 1: Demographic and clinical characteristics.
|
Age, years, mean±SD |
58.0 ± 11.0 |
59.0 ± 11.0 |
57.0 ± 10.0 |
0.017 |
|
Gender, male |
717 (66.8) |
522 (63.8) |
195 (76.5) |
< 0.001 |
|
Smoker |
104 (9.7) |
63 (7.7) |
41 (16.1) |
< 0.001 |
|
BMI ≥ 30, kg/m2 (n = 1070) |
518 (48.4) |
387 (47.3) |
131 (51.4) |
0.278 |
|
MetS (n = 1064) |
338 (31.8) |
140 (17.1) |
198 (77.6) |
< 0.001 |
|
Low HDL-C |
606 (65.5) |
404 (49.4) |
202 (79.2) |
< 0.001 |
|
Family history of CVD |
228 (21.2) |
164 (20.0) |
64 (25.1) |
0.085 |
|
Diabetes mellitus |
780 (73.0) |
585 (72.7) |
195 (76.5) |
0.121 |
|
Hypertension |
789 (73.5) |
595 (72.7) |
194 (76.1) |
0.291 |
|
Coronary artery disease |
523 (48.7) |
398 (48.7) |
125 (49.0) |
0.919 |
|
Peripheral artery disease |
31 (2.9) |
23 (2.8) |
8 (3.1) |
0.786 |
BMI: body mass index; MetS: metabolic syndrome; CVD: cerebrovascular disease; HDL-C: high-density lipoprotein cholesterol.
Low HDL-C < 1.0 mmol/L in males and < 1.3 mmol/L in females.
Table 2: Medication history.
|
Statin therapy only |
1008 (93.9) |
774 (94.6) |
234 (91.8) |
0.095 |
|
Ezetimibe-Simvastatin |
3 (0.3) |
1 (0.1) |
2 (0.8) |
0.116 |
As shown in Table 1, those with high TG levels were male (76.5% vs. 63.8%; p < 0.001), smokers (16.1% vs. 7.7%; p < 0.001), have MetS (77.6% vs. 17.1%; p < 0.001), and low HDL-C levels (79.2% vs. 49.4%; p < 0.001). As outlined in Table 2, 93.9% (n = 1008) were on statins (atorvastatin and rosuvastatin) with only 2.2% (n = 24) on the combined statins plus fenofibrate/gemfibrozil.
Only 27.4% (n = 294) of patients had non-HDL-C goal attainment. Goal attainment rates in DM (3.1% vs. 34.4%; p < 0.001), CAD (2.4% vs.37.9%; p < 0.001), DM plus CAD (0% vs. 40.0%; p < 0.001), and CVD (0% vs. 30.0%; p = 0.048) patients were significantly lower in those with higher TG compared to those with lower TG levels [Table 3].
Table 3: Non-high-density lipoprotein cholesterol goal achievements (< 2.6 mmol/L) stratified by diabetes mellitus (DM), coronary artery disease (CAD), and cerebrovascular disease (CVD).
|
All |
294 (27.4) |
284 (34.7) |
10 (3.9) |
< 0.001 |
|
DM (n = 780) |
207 (26.5) |
201 (34.4) |
6 (3.1) |
< 0.001 |
|
CAD (n = 523) |
154 (29.4) |
151 (37.9) |
3 (2.4) |
< 0.001 |
|
DM+CAD (n = 359) |
104 (29.0) |
104 (40.0) |
0 |
< 0.001 |
Discussion
This study evaluated the achievement of the non-HDL-C target < 100 mg/dL (< 2.6 mmol/L) in patients with very high ASCVD risk (DM with major risk factors and patients with established ASCVD) and high TG 150–400 mg/dL (1.7–4.5 mmol/L) versus normal TG < 150 mg/dL (< 1.7 mmol/L) despite statin-controlled LDL-C < 70 mg/dL (< 1.8 mmol/L). Non-HDL-C was achieved in 3.9% in patients with very high TG compared to 34.7% in patients with normal TG levels (p < 0.001).
Patients with high TG levels were younger and had a higher rate of smoking, MetS, and low HDL-C than patients with low TG levels. Even though most patients were on statins, only a small percentage were on combination therapies (2.2%) that specifically target the lowering of TG in both groups. Hence, this could explain the small percentage of patients achieving the non-HDL-C in both groups. Patients with high TG, low HDL-C, and high risk for ASCVD can benefit from the combination therapies of fibrate and omega 3, as shown by many studies.14–16
We found no association between ASCVD and high TG levels. This contrasts with the study by Nicholos et al,17 which demonstrated greater CV events in patients with DM with high TG levels and controlled LDL-C. The small sample size could explain our findings. Our study was not intended to look at the CV events. Several epidemiological, genetic studies, and post-hoc analyses of clinical trials demonstrated strong associations between high TG, TRLs, and ASCVD.4–6 Moreover, lower on-treatment TG level was associated with lower CV risk.18,19
Patients with DM and established ASCVD should be recommended to adhere to lifestyle intervention and evidence-based CV therapies.20 Statins are still considered the first-line therapeutic option to reduce LDL-C levels to the recommended therapeutic targets in these very high risk patients. Statins can be used as monotherapy or in combination with other treatments like ezetimibe and monoclonal PCSK9 inhibitors.12 Despite the current best treatments, patients continue to experience residual CV risk, especially in patients with high TG and low HDL-C.12 In the Fenofibrate Intervention and Event Lowering in Diabetes12 and The Action to Control Cardiovascular Risk in Diabetes15 clinical trials in diabetic patients with the subpopulation with atherogenic dyslipidemia (high TG and low HDL-C), the use of fibrate therapies alone or in combination with a statin, resulted in a significant 27% and 31% risk reduction of CV events, respectively. Moreover, the use of 4 g/d of the highly purified omega-3 fatty acid icosapent ethyl in combination with a statin in the Reduction of Cardiovascular Events With Icosapent Ethyl–Intervention Trial, in patients with elevated TG and DM or established ASCVD, resulted in a significant 25% and 20% risk reduction in CV events and CV mortality, respectively.16
Non-HDL-C is a good measure of all atherogenic lipoproteins, including LDL, very LDL, intermediate-density lipoprotein, and lipoprotein a. Several studies have shown non-HDL-C to have a better predication of ASCVD risk than LDL-C.21–23 Moreover, many international lipid guidelines consider non-HDL-C as a primary or secondary therapeutic target, especially in patients with high TG and TRLs found in high prevalence in patients with DM.12,20,24,25 Both the Middle East lipid consensus papers (2016 and the updated 2021)9,10 recommend a 50% reduction and < 70 mg/dL (< 1.8 mmol/L) for LDL-C in addition < 100 mg/dL (< 2.6 mmol/L) for non-HDL-C as primary targets in patients with very high risk including DM and established ASCVD.
Our study has important limitations. This study was an observational cross-sectional trial that did not assess long-term outcomes. We assessed TG levels, other cardiometabolic risk factors, and ASCVD at entry level and did not evaluate the impact of changes during follow-up. Observational real word data does not establish causality but provides important data concerning risk and associations as seen in clinical practice. The population studied is relatively small, and considerable variability in practice patterns across the countries exists, and probably even among study site; therefore, caution should be exercised when extrapolating the results to the general population.
Conclusion
A large proportion of statin-controlled LDL-C diabetic patients and patients with established ASCVD with high triglycerides did not achieve the non-HDL-C target. The current study did not demonstrate an association between ASCVD and high TG levels, and a follow-up study is required to assess long-term ASCVD outcomes in
this cohort.
Disclosure
The authors declared no conflicts of interest. The CEPHEUS project was sponsored by AstraZeneca. The sponsor had no involvement in the study conception, design, analysis, interpretation of data, writing, review, approval of the manuscript, or the decision to submit the manuscript
for publication.
Acknowledgements
We thank the patients, physicians, nurses, and support staff who participated in the CEPHEUS project for their invaluable cooperation. Thanks also go to ClinArt MENA for organizing the survey.
references
- 1. Al Saleh AS, Alhabib KF, Alsheik-Ali AA, Sulaiman K, Alfaleh H, Alsaif S, et al. Predictors and Impact of In-Hospital Recurrent Myocardial Infarction in Patients With Acute Coronary Syndrome: Findings From Gulf RACE-2. Angiology 2017 Jul;68(6):508-512.
- 2. Zubaid M, Rashed W, Alsheikh-Ali AA, Garadah T, Alrawahi N, Ridha M, et al. Disparity in ST-segment Elevation Myocardial Infarction Practices and Outcomes in Arabian Gulf Countries (Gulf COAST Registry). Heart Views 2017 Apr-Jun;18(2):41-46.
- 3. Al-Rasadi K, Al-Zakwani I, Alsheikh-Ali AA, Almahmeed W, Rashed W, Ridha M, et al. Prevalence, management, and outcomes of familial hypercholesterolemia in patients with acute coronary syndromes in the Arabian Gulf. J Clin Lipidol 2018 May - Jun;12(3):685-692.e2.
- 4. Al-Hashmi K, Al-Zakwani I, Al Mahmeed W, Arafah M, Al-Hinai AT, Shehab A, et al. Non-high-density lipoprotein cholesterol target achievement in patients on lipid-lowering drugs and stratified by triglyceride levels in the Arabian Gulf. J Clin Lipidol 2016 Mar-Apr;10(2):368-377.
- 5. Al-Zakwani I, Al-Mahmeed W, Arafah M, Al-Hinai AT, Shehab A, Al-Tamimi O, et al. Control of Risk Factors for Cardiovascular Disease among Multinational Patient Population in the Arabian Gulf. Curr Vasc Pharmacol 2016;14(4):374-381.
- 6. Sarwar N, Danesh J, Eiriksdottir G, Sigurdsson G, Wareham N, Bingham S, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation 2007 Jan;115(4):450-458.
- 7. Jørgensen AB, Frikke-Schmidt R, West AS, Grande P, Nordestgaard BG, Tybjærg-Hansen A. Genetically elevated non-fasting triglycerides and calculated remnant cholesterol as causal risk factors for myocardial infarction. Eur Heart J 2013 Jun;34(24):1826-1833.
- 8. Miller M, Cannon CP, Murphy SA, Qin J, Ray KK, Braunwald E; PROVE IT-TIMI 22 Investigators. Impact of triglyceride levels beyond low-density lipoprotein cholesterol after acute coronary syndrome in the PROVE IT-TIMI 22 trial. J Am Coll Cardiol 2008 Feb;51(7):724-730.
- 9. Al Sayed N, Al Waili K, Alawadi F, Al-Ghamdi S, Al Mahmeed W, Al-Nouri F, et al. Consensus clinical recommendations for the management of plasma lipid disorders in the Middle East. Int J Cardiol 2016 Dec;225:268-283.
- 10. Alsayed N, Almahmeed W, Alnouri F, Al-Waili K, Sabbour H, Sulaiman K, et al. Consensus clinical recommendations for the management of plasma lipid disorders in the Middle East: 2021 update. Atherosclerosis 2022 Feb;343:28-50.
- 11. Arafah M, Al-Hinai AT, Al Mahmeed W, Al-Rasadi K, Al Tamimi O, Al Herz S, et al. Centralized pan-Middle East Survey on the undertreatment of hypercholesterolemia: results from the CEPHEUS study in Arabian Gulf countries. Angiology 2014 Nov;65(10):919-926.
- 12. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al; ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020 Jan;41(1):111-188.
- 13. Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1 - executive summary. J Clin Lipidol 2014 Sep-Oct;8(5):473-488.
- 14. Scott R, O’Brien R, Fulcher G, Pardy C, D’Emden M, Tse D, et al; Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) Study Investigators. Effects of fenofibrate treatment on cardiovascular disease risk in 9,795 individuals with type 2 diabetes and various components of the metabolic syndrome: the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study. Diabetes Care 2009 Mar;32(3):493-498.
- 15. Ginsberg HN, Elam MB, Lovato LC, Crouse JR III, Leiter LA, Linz P, et al; ACCORD Study Group. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med 2010 Apr;362(17):1563-1574.
- 16. Peterson BE, Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, et al; REDUCE-IT Investigators. Reduction in Revascularization With Icosapent Ethyl: Insights From REDUCE-IT Revascularization Analyses. Circulation 2021 Jan;143(1):33-44.
- 17. Nichols GA, Philip S, Reynolds K, Granowitz CB, Fazio S. Increased residual cardiovascular risk in patients with diabetes and high versus normal triglycerides despite statin-controlled LDL cholesterol. Diabetes Obes Metab 2019 Feb;21(2):366-371.
- 18. Miller M, Cannon CP, Murphy SA, Qin J, Ray KK, Braunwald E; PROVE IT-TIMI 22 Investigators. Impact of triglyceride levels beyond low-density lipoprotein cholesterol after acute coronary syndrome in the PROVE IT-TIMI 22 trial. J Am Coll Cardiol 2008 Feb;51(7):724-730.
- 19. Schwartz GG, Abt M, Bao W, DeMicco D, Kallend D, Miller M, et al. Fasting triglycerides predict recurrent ischemic events in patients with acute coronary syndrome treated with statins. J Am Coll Cardiol 2015 Jun;65(21):2267-2275.
- 20. Chapman MJ, Ginsberg HN, Amarenco P, Andreotti F, Borén J, Catapano AL, et al; European Atherosclerosis Society Consensus Panel. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J 2011 Jun;32(11):1345-1361.
- 21. Sniderman AD, Williams K, Contois JH, Monroe HM, McQueen MJ, de Graaf J, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes 2011 May;4(3):337-345.
- 22. Zhang Y, Wu NQ, Li S, Zhu CG, Guo YL, Qing P, et al. Non-HDL-C is a Better Predictor for the Severity of Coronary Atherosclerosis Compared with LDL-C. Heart Lung Circ 2016 Oct;25(10):975-981.
- 23. Johannesen CD, Mortensen MB, Langsted A, Nordestgaard BG. Apolipoprotein B and Non-HDL Cholesterol Better Reflect Residual Risk Than LDL Cholesterol in Statin-Treated Patients. J Am Coll Cardiol 2021 Mar;77(11):1439-1450.
- 24. Grundy SM. Low-density lipoprotein, non-high-density lipoprotein, and apolipoprotein B as targets of lipid-lowering therapy. Circulation 2002 Nov;106(20):2526-2529.
- 25. Expert Dyslipidemia Panel of the International Atherosclerosis Society Panel members. An International Atherosclerosis Society Position Paper: global recommendations for the management of dyslipidemia–full report. J Clin Lipidol 2014 Jan-Feb;8(1):29-60.