The recent decades have seen dramatic changes in the nutritional and eating patterns worldwide. Combined with increasing sedentary behavior, a worldwide epidemic of ‘diabesity’ has arisen, where obesity and type 2 diabetes mellitus (T2DM) occur in the same individual.1 In Oman, where this paper originates, there are about 98 000 T2DM cases, rising by about 7000 a year.2 Adults with T2DM are required to adhere to a self-care regimen comprising dietary restrictions, physical exercises, medications, and self-monitoring of glucose levels. Patient Adherence to diabetes dietary guidelines is vital for sustained glycemic control and long-term health outcomes.3,4
However, shifting to a healthy diet often means dropping decades of acquired eating habits and the many related small behaviors in the course of each day. By contrast, medication adherence requires very few well-defined and brief actions daily, while the physiological, emotional, and sociological challenges associated with diet adherence may exert their amorphous and complex influences throughout the day.5,6
A T2DM patient’s diet adherence may face three additional challenges. First, the diabetic diet must be custom designed to suit the client’s weight, glucose level, and the type and stage of the disease. Secondly, different medical and dietary authorities offer varying T2DM diet plans. Thirdly, as nutritional sciences evolve, the concept of a diabetic-friendly diet also evolve. This can confuse diabetic patients and shake their resolve to follow their recommended diet. Thus, only about 25% T2DM patients adhere to their healthy diet plans.7,8
Despite the importance of diet adherence, there is a scarcity of literature devoted to it unlike the clinical aspects of diabetes management. This literature review takes a preliminary step to provide an operational definition of adherence for healthcare providers. Defining adherence and understanding its barriers may help evolve more effective strategies and tools that improve diet adherence in adults with T2DM.
In healthcare settings, the terms adherence, compliance, concordance, and sustenance are often used interchangeably.9 In the early 1970s, the scientific study on patient compliance resulted in an influential book by Sackett & Haynes, entitled Compliance with Therapeutic Regimens.10 In 1975, the term patient compliance was added as a new medical subject heading (MeSH) in the US National Library of Medicine.11
Till the mid-1990s, the terms compliance and concordance used to appear in the literature more often than adherence.9 After prolonged debates, the preference shifted to adherence as it was perceived as a nonjudgmental statement of facts rather than of blame of the provider, patient, or the treatment.9,12 Burke and Dunbar-Jacob saw adherence as emphasizing the mutual responsibility between the patient and the healthcare provider to help the patient implement and follow the treatment plan.13 In current medical terminology, adherence is used in combination with other terms like treatment adherence, medication adherence, exercise adherence, and diet adherence.
Diet adherence is the keystone of T2DM management and the first-line therapy. Dietary recommendations are individualized and usually given within the context of medical advice. A healthy daily diet includes at least 400 g (3–5 servings) of fruit and vegetables and significantly less free sugars (< 10% of total energy intake) and fats (< 30% of total energy intake). This is advocated for all adults, not only those with T2DM.14–16 Despite the proven benefits of a healthy diet, adherence in patients with T2DM remains low.17 The US-based National Health and Nutrition Examination Survey [NHANES] reported that 65% Americans with diabetes adhered to protein recommendations, 28% adhered to saturated fat recommendations, and 18% took the recommended fiber intake.18 In New Zealand, only 22% T2DM patients reported complete adherence to dietary recommendations.19 In Jordan, the adherence was even lower, at 18.6%.20
Empirical and clinical results thus indicate the need to have a clear and universal definition of diet adherence, understand its attributes, systematically investigate the barriers that cause low adherence, and develop strategies and interventions to mitigate these. Therefore, the purpose of the current study was to use concept analysis to clarify the meaning of diet adherence, its attributes, antecedents, and consequences among adults with diabetes.
Methods
We adopted the Walker and Avant method of concept analysis. It involved identifying the concept, determining the purposes of the analysis, defining the concept and its uses, determining its critical attributes, constructing the cases, identifying the antecedents and consequences, identifying illustrative cases—model, borderline, related, contrary, invented, and illegitimate—and defining the empirical referents.21
The study began by searching for research publications in English language during 2010–2020, whose abstracts contained the following terms: compliance, adherence, treatment adherence, diet adherence, T2DM, and concept analysis. The scientific databases queried were CINAHL, PubMed, PsycINFO, Health and Psychological Instruments, Psychology and Behavioral Sciences Collection, and SocINDEX. The identified articles were reviewed for inclusion. Their abstracts were evaluated for the following inclusion criteria: definition of diet adherence, defining attributes, antecedents, consequences, and measurement. Articles meeting any of these requirements were included in the study. As searches yielded insufficient numbers of good quality studies, we scoured the reference sections of the best papers, which yielded additional studies. We also referred to standard English language dictionaries for the currently accepted definitions of the key terms.
Results
Definition
The words ‘diet’ and ‘adherence’ are not found together but listed separately in prominent online dictionaries. The Cambridge English Dictionary defines adherence as “the fact of someone behaving exactly according to rules, beliefs, etc.” To adhere to something means “to continue to obey, believe in, or support something”. An adherent is “a person who strongly supports a particular person, principle, or set of ideas.” In literature, the term adherence is still used interchangeably with terms such as compliance, concordance, and maintenance, while the opposite of adherence is described as noncompliance or nonadherence. In healthcare settings, adherence is seen as one’s ability to maintain the self-care behaviors associated with a plan of care, such as taking medications as prescribed, keeping medical appointments, and following the recommended health behaviors.
For diet, the Cambridge English Dictionary offers multiple meanings. One definition relevant to this study is: “an eating plan in which someone eats less food, or only particular types of food, because they want to become thinner or for medical reasons”.5
The World Health Organization (2003) has defined adherence as the extent to which a person’s behaviour such as taking medication, following a diet, and executing lifestyle changes corresponds with agreed recommendations from a healthcare provider.26 When the term diet is paired with adherence, it presents a picture of faithful commitment to healthy dietary recommendations that are mutually planned by the healthcare provider and the recipient to promote health and prevent disease-related complications.
In adults with T2DM, the dietary plan should be individualized according to the disease stage, biochemical parameters of the recipient, and food availability. According to the American Diabetes Association there is no one-size-fits-all eating pattern for individuals with diabetes.27 Instead, patient and providers mutually discuss and evolve individualized dietary plans that combine patient preferences with healthy dietary recommendations.
Self-efficacy and self-care in patients have been found predictive of successful diet adherence.3 Social influences also play a critical role. Adherence to diet require family support with meal planning, diet recommendations, and sometimes financial support. These depend on the nature of interpersonal relationships and lifestyles within the family, as well as economic, sociocultural, and psychological factors.
Attributes of adherence
Following concept analysis method, the defining attributes of diet adherence were teased out, providing the researchers with broad insight into the concept and help differentiate it from similar and related phenomena.21 A review of numerous research studies revealed several common attributes associated with diet adherence, of which three most important attributes are discussed below.
1. Following the recommendations. This is the first attribute of diet adherence required for behavioral change. This implies that the recommendations have been understood clearly. The cognitive process involves changing the negative thoughts into a positive internal dialogue. The behavior change includes implementing new thoughts and learning new skills that help the client to practice new behavior. Currently, there are no specific dietary recommendations for patients with T2DM. However, decreased calorie intake, increased physical activity to promote weight reduction, and monitoring of carbohydrate intake are all recommended.28
2. Self-monitoring. Wilde and Garvin et al,29 defines it as the “awareness of symptoms or bodily sensations that are enhanced through periodic measurements, recordings and observations to provide information for improved self-management.” Self-monitoring of dietary intake in T2DM is an essential component of programs promoting dietary change by recording either the consumed units (calories, grams etc.) of macronutrients (carbohydrates, fats, proteins), or the consumed number and sizes of servings of various food groups.30 The process of self-monitoring of diet has three components: awareness of the importance of monitoring, interpretation of the current situation, and response to the outcomes.31 These components are closely related, interdependent, and non-hierarchical. A significant association has been found between self-monitoring of diet and weight loss.32
3. Maintenance and relapse prevention. Maintenance is a critical stage in the diet adherence process, but research is not clear about how interventions can be made to sustain diet adherence over time until it becomes an integral part of a lifestyle.33 Successful weight loss maintenance criteria include eating a low-fat, low-calorie diet, frequent monitoring of weight of at least once a week, staying connected to the source of support, and an hour of moderate-intensity physical activity per day.34
After the successful implementation and maintenance of dietary recommendations, it is essential to monitor for relapse prevention. Individuals who have made dietary changes face many high-risk situations that can lead to lapses. Psychosocial events such as stress, divorce, job change, or financial worries may drive people to go back to their old unhealthy diet. Relapse prevention training enables individuals to predict, strategize, and manage high-risk dietary situations.
Antecedents
Antecedents are described as factors that must precede the occurrence of interest towards a health plan.21 The most important antecedents are motivation, understanding the dietary recommendations, self-efficacy, goal setting, and social support. These play a significant role in determining the extent of dietary adherence and predicting the success of the behavior change. Lack of motivation and lack of understanding have been identified as the main obstacles to diet adherence.35
The first antecedent identified in this concept analysis is motivation, which plays a crucial role in adherence.35 Motivation mobilizes personal abilities and improves commitment to the recommended diet. Motivation is vital during the initial phase of behavior change and essential throughout the treatment period. Numerous studies have found that motivational enhancement is significantly associated with reduction in glycated hemoglobin (HbA1c) in adults with T2DM.36,37
The second antecedent is understanding the dietary recommendations. Understanding implies the mental grasping and the capacity to apprehend general relations of the received information. In a study among 98 adults that investigated their understanding of the Dietary Guidelines for Americans, a minority of the participants misinterpreted the guidelines, suggesting a lack of understanding.38 In a randomized control trial conducted among 90 patients with T2D, those who had received group discussion-based education where information and understanding were emphasized showed better adherence to diet (t = 5.22, p < 0.001).39
Health beliefs and self-efficacy are other important antecedents of dietary adherence. Self-efficacy is individuals’ belief in their capacity to execute a specific behavior required to produce a particular outcome.40 Individuals who demonstrated high self-efficacy for long-term maintenance were better in relapse prevention and problem-solving.41 A study conducted by Yun and Choi,42 (2016) found that a dietary program based on self-efficacy helped improve adherence to the diet. Another similar study found that improvement in self-efficacy over time was associated with better dietary adherence and significant weight loss.43 Similarly, health beliefs were found to improve adherence to dietary recommendations.44
Goal setting is the fifth identified factor that influences dietary adherence positively. Once the person gets motivated to start a dietary program, reasonable goals must be established. Setting SMART goals (Specific, Measurable, Attainable, Rewarding, and Timely) may help to achieve dietary changes that will improve long-term outcomes. Goals may be benchmarked on an established set of recommendations, such as the American Diabetes Association’s dietary guidelines, and then tweaked to suit individual circumstances.
Social support is crucial for successful dietary adherence. It involves active inclusion of the individual’s spouse or others in the household who are most responsible for cooking, shopping, and meal planning. Social support benefits patient health by moderating stress, changing affective states, increasing self-efficacy, and facilitating the extinction of negative health habits.45 Empirical studies have shown that social support significantly improves diet adherence of chronic patients.46
Consequences
Adherence to healthy dietary recommendations has shown to cure diseases, slow disease progression, and markedly reduce the risk of chronic diseases to a similar extent as pharmacologic therapy.47 In adults with T2DM, it improves disease-specific parameters such as lower body mass index (BMI) and HbA1c, better levels of triglycerides and cholesterols, and lower diastolic blood pressure.48 Psychological benefits include improved self-esteem, self-confidence, and overall health-related quality of life (HRQoL).49 A summary of the antecedents, defining attributes, and consequences of diet adherence are presented in Figure 1.
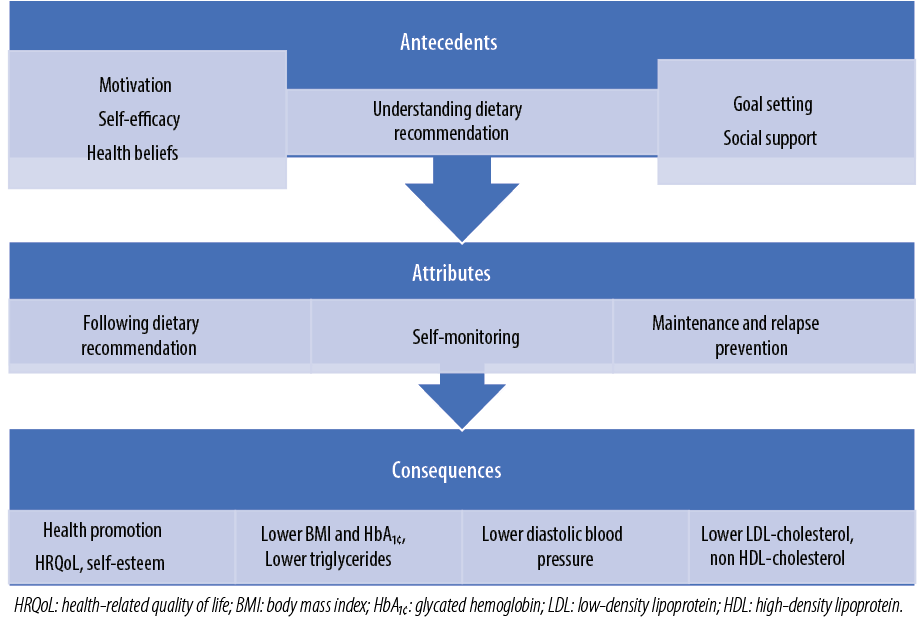
Figure 1: Attributes, antecedents, and consequences of diet adherence in adults with type 2 diabetes mellitus.
Examples of various levels of adherence
Model Case
Sam, aged 42 years, 280 lb, BMI 32, reports a sedentary lifestyle, and consumes over 5000 calories daily. A banker, he lives with his wife and three children. Four months ago, he started feeling tired and thirsty and developed polyuria. Sam’s family physician diagnoses him with T2DM and hyperlipidemia. The physician explains the prognosis of these conditions and encourages Sam to modify his diet and exercise and starts him on the first line pharmacotherapy. Sam understands the necessity of a healthy diet and believes he is capable of adhering to it. He and the doctor together set a goal of weight reduction by three pounds a month through diet and exercise. Sam is motivated to start his new diet plan. At home his wife encourages him and starts making food as per his diet plan. Sam consistently adheres to his new diet, exercises and weighs himself daily, and regularly records the nutritional values and calories of his food intake. Three months later, Sam’s physician is gratified to see him to have achieved the agreed nine pounds reduction. His BMI has dropped to 27. The other clinical parameters like HbA1c, low-density lipoprotein (LDL)-cholesterol, and triglycerides have also improved significantly. Encouraged by his physician, Sam plans to continue with his new lifestyle and avoid relapse.
Borderline Case
Sara is a 55-year-old woman who presents with polyuria, polydipsia, and ‘feeling dry’ during the past two months. She has a three-year history of poorly controlled T2DM. Her fasting blood glucose is 350 mg/dL, initial serum cholesterol is 300 mg/dL, triglycerides at 940 mg/dL, and high-density lipoprotein (HDL) cholesterol at 32 mg/dL. Her endocrinologist explains the risks of uncontrolled hyperglycemia and hyperlipidemia and encourages her for a lifestyle change. The physician and Sara draw a plan for three months and set achievable goals. Sara feels motivated and starts a program of healthy diet and daily physical exercises. Sara initially adheres to diet and exercise plan despite barriers such economic difficulties, lack of family support, and stress, but finds her diet plan increasingly intolerable. After one month, she stops adhering to much of her diet plan. However, she does continue with daily physical exercises. Even though she has not followed through with tracking calories and modifying her nutrient intake, she has tried to reduce portion size and the frequency of meals. She hopes that exercise alone will help and is open to medication to improve her glycemic control.
Contrary Case
Jacob is a 52-year-old man with obesity and a seven-year history of T2DM. He presents with fatigue, difficulty losing weight, and lack of motivation. He is living alone, and most of his meals are from fast-food restaurants. His health care practitioners have repeatedly advised weight loss and exercise. He tries to follow dietary recommendations but fails and resumes to his former lifestyle. He reveals that the pain in his knees and ankles makes it difficult to exercise. His laboratory parameters are worsening with each visit to the obesity clinic. He believes that the disease is from God whose wisdom should not be questioned.
Empirical Referents
Walker and Avant (2011) viewed empirical referents as the means by which an individual can recognize or measure the defining characteristics or attributes.21 The literature provides various self-report tools to measure the attributes of diet adherence. Perceived dietary adherence questionnaire (PDAQ) is a self-report screening tool used to monitor dietary adherence in patients with T2DM.50 The questionnaire consists of nine questions rated on a seven-point Likert scale structured to cover recent diabetes nutrition therapy guidelines. The correlation coefficients for PDAQ items range from 0.46 to 0.11. The intra-class correlation is 0.78, indicating high reliability.50 When compared with the 24 hours recall method, PDAQ showed excellent convergent validity in terms of dietary recommendations specific to people with T2DM, and includes vegetables and fruits, foods with low glycemic index, sugars, and fats. These results suggested PDAQ to be a valid and reliable measure of diabetes dietary recommendations.
Patient diet adherence in diabetes (PDAD) scale is another standardized tool developed based on Polish Diabetes Association guidelines and consists of 20 behaviors demonstrating dietary options for adults with T2DM.51 Each behavior scores one point with a maximum possible score of 20. However, psychometric analysis of the instrument’s internal consistency yielded only 0.642, and the factorial analysis of the instrument suggested a significant degree of variation in the evaluated behaviors (from physical exercise through to alcohol drinking and eating behaviors).51 The main disadvantage of PDAD is that it does not focus on one construct, but on various unhealthy behaviors.
The compliance praxis survey-diet (COMPASS-Diet) is another instrument used to measure adherence to dietary recommendations. The COMPASS-Diet survey measures four components of adherence: normative behavior, effective structural circumstances, social support, and wisdom/knowledge.52 Each of these components contains three items answered on a 9-point Likert-type scale (from completely disagree to completely agree) with a score range of 12–108 points. COMPASS-Diet has been shown to have internal consistency and excellent internal reliability (Cronbach alpha at 0.82).52 The instrument gives special importance to knowledge and social support.
Other commonly used tools are food frequency questionnaires (FFQ), 24-hour recalls, and multi-day food diaries.53 The FFQ is used to measure long-term dietary habits. It presents a list of foods, accompanied by a close-ended question that asks about frequency of consumption for each item, usually over the preceding year. FFQ is inexpensive and relatively easy for participants to complete. On the downside, it offers a fixed food list, which must be tailored to the targeted population and market availability.54 The 24-hour dietary recall is a structured interview aimed to gather detailed information about all foods, drinks, and dietary supplements consumed in the preceding 24 hours. The tool can either be administered by a trained interviewer or through automated self-administered tools. The 24-hour recall is very helpful in measuring actual dietary behaviors, examining relationships between diet and other factors, and evaluating the effectiveness of diet interventional studies.55 Multi-day food diaries is similar to 24-hour recalls, repeated over multiple days of food diary entries. Both these tools are easy to administer and inexpensive, but time-consuming to complete and analyze.
Discussion
The results of this concept analysis indicate that diet adherence is integral to T2DM management. It has also teased out the individual attributes of diet adherence: following diet recommendations, self-monitoring, maintenance, and relapse prevention. Also identified are the antecedents for diet adherence: motivation, understanding of diet recommendations, health beliefs, self-efficacy, goal setting, and social support. The consequences of successful diet adherence were identified to include: overall health gain, enhanced HRQoL, and improved disease-specific clinical parameters such as lower BMI and HbA1c, a better level of triglycerides, LDL-cholesterol, non-HDL-cholesterol, and lower diastolic blood pressure.
The results of this concept analysis also suggest that diet adherence in T2DM may be understood through the lenses of the Information–Motivation–Behavioral (IMB) skills model, some constructs of the Health Belief Model, and the Transtheoretical Model. The IMB model constructs have been applied to many promotive behaviors that include adherence to medications, diet, and exercise.56 The constructs of the model, including information, motivation, and behavioral skills, are congruent with the antecedents and attributes of diet adherence concept analysis. While understanding dietary information and motivation represents the first and second constructs of IMB, following diet recommendations, self-monitoring, maintenance, and relapse prevention fit well with the third construct of IMB. The Health Belief Model is another model that can be used to explain diet adherence. The model theorizes that people’s beliefs about whether or not they are at risk for a disease or health problem, and their perceptions of the benefits of taking action to avoid it, influence their readiness to act.57 In the case of T2DM, persons’ beliefs about the benefits of diet adherence in preventing disease complications will influence their decision and action. The Transtheoretical Model and stages of change offers yet another explanation of the diet adherence concept. It proposes that long-term changes in health behavior involve multiple actions and adaptations over time.58 The theory states five stages of change: pre-contemplation, contemplation, preparation, action, and maintenance. These stages of change are consistent with the antecedents and attributes identified for the concept of diet adherence, the need to initiate and then maintain diet changes over time, and to prevent relapse.
Diet adherence is affected by social pressure, cultural, psychological factors, and self-efficacy specific to diet. Antecedents can be distinguished in terms of social factors (e.g., watching others consume forbidden foods) and individual factors (e.g., adhering to diet recommendations, resisting the offer to eat unhealthy foods at social events). Fatalism or beliefs about the causes of diabetes outside the self are associated with low socioeconomic status and negatively associated with adherence.59 Diet adherence is a mediating factor for the effects of individual beliefs, attitudes, and self-efficacy on health outcomes among adults with T2DM.
Diet adherence has numerous implications for health research and clinical practice. In research, operationalizing the definition of diet adherence will help develop valid and reliable tools, effective interventions, and long-term strategies to improve diet adherence in adults with T2DM. In clinical practice, understanding the term ‘diet adherence’ can help nurses encourage patients to adhere to lifestyle modifications. It also may help healthcare providers and nurses to advocate for their patients to receive a comprehensive discharge plan that focuses on the importance of medications, diet, and exercise.
Our adoption of the Walker and Avant (2011) strategy for concept analysis caused the literature search to be restricted to the papers that met Walker and Avant’s (2011) guidelines. This can be seen as a limitation of this study, as the identification of the concept antecedents, attributes, and consequences are dependent on the literature reviewed and the researcher’s understanding of the literature.
Conclusion
The results of this concept analysis suggest that diet adherence in T2DM may be understood through the IMB skills model, some constructs of the Health Belief Model, and the Transtheoretical Model. The Walker and Avant’s concept analysis method provided a step-by-step guide to concept analysis. The current findings contribute to the body of knowledge that help educating nurses and adults with T2DM with the full spectrum of the meaning of diet adherence and its attributes so that both the nurse and the patient understand each other clearly. With improved understanding, they can together arrive on personalized nutritional choices for better outcome. Further research should aim to develop practical interventions that strengthen and sustain diet adherence in adults with T2DM.
references
- 1. Pappachan JM, Viswanath AK. Medical Management of Diabesity: Do We Have Realistic Targets? Curr Diab Rep. 2017 Jan;17(1):4.
- 2. Ministry of Health Oman. Annual health report 2018, Statistical reports; 2018.
- 3. D’Souza MS, Karkada SN, Parahoo K, Venkatesaperumal R, Achora S, Cayaban AR. Self-efficacy and self-care behaviours among adults with type 2 diabetes. Appl Nurs Res 2017 Aug;36:25-32.
- 4. Raj GD, Hashemi Z, Soria Contreras DC, Babwik S, Maxwell D, Bell RC, et al. Adherence to diabetes dietary guidelines assessed using a validated questionnaire predicts glucose control in adults with type 2 diabetes. Can J Diabetes 2018 Feb;42(1):78-87.
- 5. Kelly MP, Barker M. Why is changing health-related behaviour so difficult? Public Health 2016 Jul;136:109-116.
- 6. Cook PF, Schmiege SJ, Reeder B, Horton-Deutsch S, Lowe NK, Meek P. Temporal immediacy: a two-system theory of mind for understanding and changing health behaviors. Nurs Res 2018 Mar/Apr;67(2):108-121.
- 7. Al-Sinani M, Min Y, Ghebremeskel K, Qazaq HS. Effectiveness of and adherence to dietary and lifestyle counselling: effect on metabolic control in type 2 diabetic Omani patients. Sultan Qaboos Univ Med J 2010 Dec;10(3):341-349.
- 8. Ayele AA, Emiru YK, Tiruneh SA, Ayele BA, Gebremariam AD, Tegegn HG. Level of adherence to dietary recommendations and barriers among type 2 diabetic patients: a cross-sectional study in an Ethiopian hospital. Clin Diabetes Endocrinol 2018 Nov;4(1):21.
- 9. Chakrabarti S. What’s in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World J Psychiatry 2014 Jun;4(2):30-36.
- 10. Compliance with therapeutic regimens. In: David L, Sackett R, Brian H, editors. Johns Hopkins University Press, Baltimore, Md; 1976. p.293.
- 11. Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al; ABC Project Team. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 2012 May;73(5):691-705.
- 12. McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA 2002 Dec;288(22):2868-2879.
- 13. Burke LE, Dunbar-Jacob J. Adherence to medication, diet, and activity recommendations: from assessment to maintenance. J Cardiovasc Nurs 1995 Jan;9(2):62-79.
- 14. World Health Organization. Guideline: sugars intake for adults and children. 2015 [cited 2019 June 6] Available from: https://www.who.int/publications/i/item/9789241549028.
- 15. Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell CD, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev 2015 Aug;(8):CD011834.
- 16. Fats and fatty acids in human nutrition. Report of an expert consultation. FAO Food Nutr Pap 2010;91:1-166.
- 17. García-Pérez L-E, Alvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther 2013 Dec;4(2):175-194.
- 18. Halali F, Mahdavi R, Mobasseri M, Asghari Jafarabadi M, Karimi Avval S. Perceived barriers to recommended dietary adherence in patients with type 2 diabetes in Iran. Eat Behav 2016 Apr;21:205-210.
- 19. Broadbent E, Donkin L, Stroh JC. Illness and treatment perceptions are associated with adherence to medications, diet, and exercise in diabetic patients. Diabetes Care 2011 Feb;34(2):338-340.
- 20. Khattab M, Khader YS, Al-Khawaldeh A, Ajlouni K. Factors associated with poor glycemic control among patients with type 2 diabetes. J Diabetes Complications 2010 Mar-Apr;24(2):84-89.
- 21. Walker LO, Avant KC. Strategies for theory construction in nursing. Boston: Prentice Hall; 2011.
- 22. “Adherence.” Cambridge Dictionary (Online). [cited 2022 February 21]. Available from: https://dictionary.cambridge.org/dictionary/english/adherence?q=Adherence+.
- 23. “Adhere-to-something.” Cambridge Dictionary (Online). [cited 2022 February 21]. Available from: https://dictionary.cambridge.org/dictionary/english/adhere-to-something.
- 24. “Adherent.” Cambridge Dictionary (Online). [cited 2022 February 21]. Available from: https://dictionary.cambridge.org/dictionary/english/adherent.
- 25. “Diet.” Cambridge Dictionary (Online). [cited 2022 February 21]. Available from: https://dictionary.cambridge.org/dictionary/english/diet.
- 26. World Health Organization. Adherence to long-term therapies: evidence for action / [edited by Eduardo Sabaté]. Geneva: World Health Organization; 2003.
- 27. American Diabetes Association. Lifestyle management; standards of medical care in diabetes—2018. Diabetes Care 2018 Jan;41(Suppl 1):S38-S50.
- 28. Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity/exercise and diabetes: a position statement of the American diabetes association. Diabetes Care 2016 Nov;39(11):2065-2079.
- 29. Wilde MH, Garvin S. A concept analysis of self-monitoring. J Adv Nurs 2007 Feb;57(3):339-350.
- 30. Treatment adherence: a practical handbook for health care providers. Thousand Oaks, California: SAGE Publications, Inc; 2006.
- 31. Song M, Lipman TH. Concept analysis: self-monitoring in type 2 diabetes mellitus. Int J Nurs Stud 2008 Nov;45(11):1700-1710.
- 32. Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011 Jan;111(1):92-102.
- 33. Pullen C, Noble Walker S. Midlife and older rural women’s adherence to U.S. dietary guidelines across stages of change in healthy eating. Public Health Nurs 2002 May-Jun;19(3):170-178.
- 34. Shay LE. A concept analysis: adherence and weight loss. Nurs Forum 2008 Jan-Mar;43(1):42-52.
- 35. Cook PF, Schmiege SJ, Bradley-Springer L, Starr W, Carrington JM. Motivation as a mechanism for daily experiences’ effects on HIV medication adherence. J Assoc Nurses AIDS Care 2018 May - Jun;29(3):383-393.
- 36. Li M, Li T, Shi BY, Gao CX. Impact of motivational interviewing on the quality of life and its related factors in type 2 diabetes mellitus patients with poor long-term glycemic control. Int J Nurs Sci 2014;1(3):250-254.
- 37. Pourisharif H, Babapour J, Zamani R, Besharat MA, Mehryar AH, Rajab A. The effectiveness of motivational interviewing in improving health outcomes in adults with type 2 diabetes. Procedia Soc Behav Sci 2010;5:1580-1584.
- 38. Chea M, Mobley AR. Interpretation and understanding of the dietary guidelines for Americans consumer messages among low-income adults. J Am Coll Nutr 2020 Jan;39(1):63-71.
- 39. Habibzadeh H, Sofiani A, Alilu L, Gillespie M. The effect of group discussion-based education on self-management of adults with type 2 diabetes mellitus compared with usual care: a randomized control trial. Oman Med J 2017 Nov;32(6):499-506.
- 40. Bandura A. Self-efficacy: the exercise of control. New York: W H. Freeman and Company; 1997.
- 41. Nikmanesh Z, Baluchi MH, Pirasteh Motlagh AA. The role of self-efficacy beliefs and social support on prediction of addiction relapse. Int J High Risk Behav Addict 2017;6(1):e21209.
- 42. Yun KS, Choi JY. Effects of dietary program based on self-efficacy theory on dietary adherence, physical indices and quality of life for hemodialysis patients. J Korean Acad Nurs 2016 Aug;46(4):598-609.
- 43. Warziski MT, Sereika SM, Styn MA, Music E, Burke LE. Changes in self-efficacy and dietary adherence: the impact on weight loss in the PREFER study. J Behav Med 2008 Feb;31(1):81-92.
- 44. Clark-Cutaia MN, Ren D, Hoffman LA, Burke LE, Sevick MA. Adherence to hemodialysis dietary sodium recommendations: influence of patient characteristics, self-efficacy, and perceived barriers. J Ren Nutr 2014 Mar;24(2):92-99.
- 45. Miller TA, Dimatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes 2013 Nov;6:421-426.
- 46. Ahrari S, Moshki M, Bahrami M. The relationship between social support and adherence of dietary and fluids restrictions among hemodialysis patients in Iran. J Caring Sci 2014 Feb;3(1):11-19.
- 47. Hill AM, Fleming JA, Kris-Etherton PM. The role of diet and nutritional supplements in preventing and treating cardiovascular disease. Curr Opin Cardiol 2009 Sep;24(5):433-441.
- 48. Davison KA, Negrato CA, Cobas R, Matheus A, Tannus L, Palma CS, et al; Brazilian Type 1 Diabetes Study Group (BrazDiab1SG). Relationship between adherence to diet, glycemic control and cardiovascular risk factors in patients with type 1 diabetes: a nationwide survey in Brazil. Nutr J 2014 Mar;13(1):19.
- 49. Knox E, Muros JJ. Association of lifestyle behaviours with self-esteem through health-related quality of life in Spanish adolescents. Eur J Pediatr 2017 May;176(5):621-628.
- 50. Asaad G, Sadegian M, Lau R, Xu Y, Soria-Contreras DC, Bell RC, et al. The reliability and validity of the perceived dietary adherence questionnaire for people with type 2 diabetes. Nutrients 2015 Jul;7(7):5484-5496.
- 51. Jaworski M, Panczyk M, Cedro M, Kucharska A. Adherence to dietary recommendations in diabetes mellitus: disease acceptance as a potential mediator. Patient Prefer Adherence 2018 Jan;12:163-174.
- 52. Janda M, Zeidler D, Böhm G, Schoberberger R. An instrument to measure adherence to weight loss programs: the compliance praxis survey-diet (COMPASS-Diet). Nutrients 2013 Sep;5(10):3828-3838.
- 53. Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health 2014;36.
- 54. Thornton K, Villamor E. Nutritional epidemiology. In: Caballero B, Finglas PM, Toldrá F, editors. Encyclopedia of Food and Health. Oxford: Academic Press; 2016. p. 104-107.
- 55. National Institutes of Health, National Cancer Institute. Dietary assessment primer. [cited 2019 September 24]. Available from: https://dietassessmentprimer.cancer.gov/.
- 56. Jeon E, Park H-A. Development of the IMB model and an evidence-based diabetes self-management mobile application. Healthc Inform Res 2018 Apr;24(2):125-138.
- 57. Jones CL, Jensen JD, Scherr CL, Brown NR, Christy K, Weaver J. The health belief model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation. Health Commun 2015;30(6):566-576.
- 58. Huang CL, Tang SM. An experience using the transtheoretical model of health behavior change to promote exercise in a type 2 diabetes patient. The Journal of Nursing 2007;54(5):99-103.
- 59. Gutierrez AP, McCurley JL, Roesch SC, Gonzalez P, Castañeda SF, Penedo FJ, et al. Fatalism and hypertension prevalence, awareness, treatment and control in US Hispanics/Latinos: results from HCHS/SOL Sociocultural Ancillary Study. J Behav Med 2017 Apr;40(2):271-280.