The intrathoracic lesions constitute a common clinical problem in which multiple diagnostic dilemmas arise. The use of imaging methods such as computed tomography, magnetic resonance imaging of mediastinum, positron emission tomography, and chest ultrasound have helped clinicians to reach a diagnosis.1–3 Invasive methods such as bronchoscopy, thoracoscopy, mediastinoscopy, and exploratory thoracotomy are sometimes essential for the proper diagnosis.4–6
Another option for diagnosing intrathoracic lesions can be the biopsy of extrathoracic tissues such as scalene lymph node biopsy. This biopsy can be conducted through Daniel’s technique [Figure 1].7,8 This technique is simple and can be conducted using local anesthesia, thus preventing the patient from complications of general anesthesia. An incision is made over the clavicle and laterally to the sternocleidomastoid muscle. The clavicular part of this muscle can be divided, and the whole muscle is retracted more centrally. Through this movement, the area under the anterior scalenus muscle is exposed. This area contains fat and multiple lymph nodes, which can be easily and safely removed. Additionally, with the use of this technique, the subclavian and jugular vessels can be followed in the mediastinum to extract more lymph nodes and increase the possibility for diagnosis.7
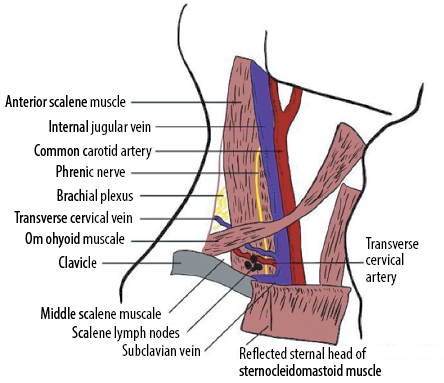
Figure 1: Daniel’s lymph node biopsy.
This technique has been used in various cases. These include rare microorganisms, malignancies, and autoimmune disorders, such as sarcoidosis.9–12 This method can be very helpful for the differential diagnosis of various diseases when other laboratory and imaging methods cannot help. The tissue from the lymph node can be thoroughly examined histopathologically and cultured to reveal diseases such as lymphomas, tuberculosis, and sarcoidosis.12 In addition, the histopathological confirmation of the malignancy can help the physician locate the exact position of the lesion.12 The main complication of Daniel’s technique is the injury of the thoracic duct, mainly in the left,7 however, its use has significant advantages. First of all, it constitutes a simple surgical technique, less invasive than others such as exploratory thoracotomy. More invasive surgeries for the patient can be avoided by using Daniel’s technique for the diagnosis.7 Furthermore, local anesthesia is more attractive than general anesthesia and safer in patients unable to undergo surgery.13 Finally, it might also be more cost-effective for the diagnosis, compared to the use of various imaging methods such as PET.14
In conclusion, Daniel’s technique constitutes a surgical method, which is temporarily out of use and forgotten. This might have happened because new methods replace old ones and science progresses. Sometimes, however, past and more advanced methods can offer better clinical outcomes. Therefore, new surgeons should learn and consider this method since it contains numerous advantages and few disadvantages.
references
- Goo HW, Goo JM, Dual-Energy CT. Dual-Energy CT: new horizon in medical imaging. Korean J Radiol 2017 Jul-Aug;18(4):555-569.
- Pessôa FM, de Melo AS, Souza AS Jr, de Souza LS, Hochhegger B, Zanetti G, et al. Applications of magnetic resonance imaging of the thorax in pleural diseases: a state-of-the-art review. Lung 2016 Aug;194(4):501-509.
- Yildirim H, Metintas M, Entok E, Ak G, Ak I, Dundar E, et al. Clinical value of fluorodeoxyglucose-positron emission tomography/computed tomography in differentiation of malignant mesothelioma from asbestos-related benign pleural disease: an observational pilot study. J Thorac Oncol 2009 Dec;4(12):1480-1484.
- 4. Batra H, Yarmus L. Indications and complications of rigid bronchoscopy. Expert Rev Respir Med 2018 Jun;12(6):509-520.
- 5. Anevlavis S, Varga C, Nam TH, Man RW, Demetriou A, Jain N, et al. Is there any role for thoracoscopy in the diagnosis of benign pleural effusions. Clin Respir J 2019 Feb;13(2):73-81.
- 6. Sarrazin R, Dyon JF. [Mediastinoscopy]. Rev Mal Respir 1992;9(1):99-110.
- 7. Daniels AC. A method of biopsy useful in diagnosing certain intrathoracic diseases. Dis Chest 1949 Sep;16(3):360-367.
- 8. Freise G, Rensch H. [Results of Daniel’s scalenus lymph nodesbopsy and biopsy of the upper frontal mediastinum according to Carlens]. Thoraxchir Vask Chir 1967 Apr;15(2):133-141.
- 9. Johnson JE Jr, MacCurdy JM. Pulmonary histoplasmosis diagnosed by scalene node biopsy. Am Rev Tuberc 1952 Oct;66(4):497-500.
- 10. Weiss HA, Campbell RM, Budenz GC, McCANDLESS CM Jr. Sarcoidosis diagnosed by means of subclavian lymph node biopsy; report of a case. J Am Med Assoc 1951 Jul;146(13):1221-1222.
- 11. Storey CF, Reynolds BM. Biopsy techniques in the diagnosis of intrathoracic lesions, including lung biopsy, mediastinal biopsy and resection of the deep cervical fat pad and its contained nodes; report of 12 illustrative cases. Dis Chest 1953 Apr;23(4):257-282.
- 12. Shefts LM, Terrill AA, Swindell H. Scalene node biopsy. Am Rev Tuberc 1953 Oct;68(4):505-522.
- 13. Patelis N, Diakomi M, Maskanakis A, Maltezos K, Schizas D, Papaioannou M. General versus local anesthesia for carotid endarterectomy: Special considerations. Saudi J Anaesth 2018 Oct-Dec;12(4):612-617.
- 14. Gerke O, Hermansson R, Hess S, Schifter S, Vach W, Høilund-Carlsen PF. Cost-effectiveness of PET and PET/computed tomography: a systematic review. PET Clin 2015 Jan;10(1):105-124.