A 45-year-old woman presented with bilateral, painless slowly-progressing cervical lumps for the past eight years. She never had a chronic cough, weight loss, or trauma. Her appetite and bowel habits were satisfactory throughout this period. Her pitch and caliber of voice were normal, without any dysphagia, loss of taste, or earache. Her family history was insignificant. General physical and systemic examinations were normal. Local examination revealed 3 × 2 cm and 3.5 × 3 cm globular firm rubbery non-tender cervical masses located anterior to the sternocleidomastoid muscles just below the angles of mandibles on the right and left sides, respectively [Figure 1]. They were well-mobile horizontally, but had restricted mobility in the vertical direction, non-compressible, pulsatile on deep palpation, and did not move with deglutition. No other lumps were felt in any triangles of the neck. Her ear, nose, throat, and indirect laryngoscopic examinations did not reveal any abnormality. Her bimanual oral examination was normal.
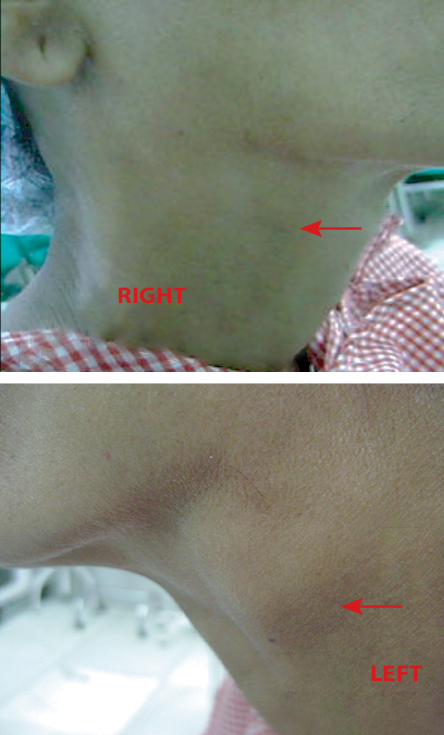
Figure 1: Bilateral, painless cervical lumps on a 45-year-old patient, which had been slowly-progressing over eight years.
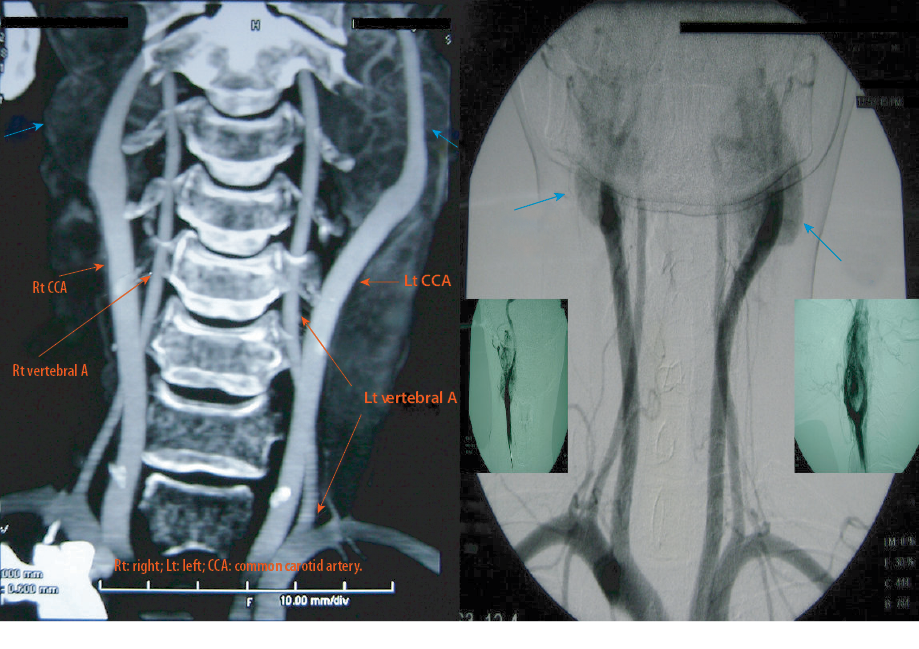
Figure 2: Contrast-enhanced computed tomography (CECT) (3D reconstruction) with digital subtraction angiogram of carotid body tumor. Note, bilateral intensely hypervascular masses (blue arrows) at but not encircling the carotid bifurcation (red arrows), splaying external and internal carotid arteries—the pathognomonic lyre sign. Also, note the absence of tumor thrombus or vascular dilation.
Local ultrasonography revealed solitary well-defined hypoechoic lesions on either side of the neck located at the carotid bifurcations. On addition of color Doppler, they exhibited intense tumor blush. A contrast-enhanced computed tomography (CECT) scan with digital subtraction angiography demonstrated two distinct well-demarcated masses—3.2 × 2.3 × 1.5 cm and 3.7 × 3.2 × 2 cm— at the carotid bifurcations on the right and left sides, respectively. They were homogeneously enhancing, loosely abutting against the external carotid artery (ECA) for about 80o on either side without infiltration. Maintaining the calibers, tumors splayed respective ECAs and internal carotid artery (ICA) distinctly [Figure 2].
Question
1. What is the probable diagnosis?
a) Tuberculous lymphadenitis.
b) Carotid body tumors (CBTs).
c) Thyroid nodules.
d) Enlarged submandibular glands.
Answer
b) Carotid body tumors.
The clinical presentation and the radiological findings are typical of CBT. However, the patient refused staged excision and opted for surveillance. Over one year follow-up, she is doing well, and the lumps have remained unchanged in size and character.
Discussion
Carotid body, a relatively small but extremely vital organelle situated at the carotid artery bifurcation, was first described by von Haller in 1743.1,2
A part of the paraganglion system, it contains a conglomeration of highly vascular and innervated chemoreceptor tissue specialized in ameliorating hypoxia, hypercapnia, and acidosis by modulating the autonomic nervous pathway.2–4 These carotid bodies produce catecholamines and are said to be essential during fetal development.2
CBT, better nominated as carotid body paraganglioma, was first reported by von Luschka in 1862.2 It could be sporadic (commonest), familial (due to mutations in succinate dehydrogenase gene), or hyperplastic (secondary to chronic hypoxia, like at high altitudes).2–4 As such, bilateral disease is less common—seen more frequently in the familial (30%) than in the sporadic (5%) variety.2–4 Only 5%–10% eventually undergoes malignant transformation.3
The most important ‘rate limiting’ step in its management is keeping a high index of suspicion generated after a sound physical examination and rational judgment or else the clinician could easily fall to its deceptive clinical appearance and offer commoner differentials like lymphadenopathy or thyromegaly (others being salivary gland tumors or carotid aneurysms) leading to disastrous consequences like advising needle aspiration or even a biopsy.1,2,4 Here, though its typical clinical presentation (painless cervical lump) could be inherently confusing, the Fontaine sign (free mobility in horizontal rather than craniocaudal plane) could clinch the clinical diagnosis in favor of CBT.1,2
Duplex ultrasound, a handy initial investigation, reveals a hypervascular tumor at the carotid bifurcation.2,4 However, CT and magnetic resonance angiography are modern non-invasive vascular mapping tools that produce reliable, high-quality images depicting homogenously-enhancing lesion splaying ICA and ECA (the classic lyre sign), the extent of infiltration and degree of encircling carotid artery along with its precise size and craniocaudal extent.1,2,4,5 Based on these criteria, Shamblin et al grouped CBTs into type I (small size, < 180o carotid encircling), type II (medium size, 180o–270o carotid encircling), and type III (large size, > 270o carotid encircling).1,2 While early lesions (type I and II) merit immediate curative surgical excision by sequential craniocaudal or retrocarotid dissection techniques, it is considered prudent to administer preoperative chemoembolization and radiation to advance tumors (type III) before subjecting them to extirpative surgery involving complicated vascular reconstruction.1,2 This reduces perioperative bleeding and major cranial nerve (X-XII) deficits as high as 40%.3 However, for bilateral disease, a staged approach is recommended in which a larger tumor is excised before smaller ones at two separate sittings to avoid labile hypertension.3
Thus, CBTs demand a high degree of suspicion and optimum imaging for pinpointing the diagnosis. This ultimately incurs multidisciplinary involvement critical to achieving better results.1
Disclosure
Written consent was obtained from the patient.
references
- 1. Fan D, Luster S, Eid IG, Saied Calvino A. A multidisciplinary approach to carotid body tumors surgical management. J Surg Case Rep 2020 Mar 2;2020(3):rjaa030.
- 2. Butt N, Baek WK, Lachkar S, Iwanaga J, Mian A, Blaak C, et al. The carotid body and associated tumors: updated review with clinical/surgical significance. Br J Neurosurg 2019 Oct;33(5):500-503.
- 3. Bobadilla-Rosado LO, Garcia-Alva R, Anaya-Ayala JE, Peralta-Vazquez C, Hernandez-Sotelo K, Luna L, et al. Surgical management of bilateral carotid body tumors. Ann Vasc Surg 2019 May;57:187-193.
- 4. Anand J, Singh JP. Bilateral sporadic carotid body tumors-a rare case report. Radiol Case Rep 2018 Aug;13(5):988-992.
- 5. Razek AA, Gaballa G, Megahed AS, Elmogy E. Time resolved imaging of contrast kinetics (TRICKS) MR angiography of arteriovenous malformations of head and neck. Eur J Radiol 2013 Nov;82(11):1885-1891.