Approximately three million people worldwide are affected by multiple sclerosis (MS), with Caucasians having a higher incidence than sub-Saharan Africans.1 The estimated crude prevalence of MS in Oman rose to 15.9/100 000 by 2019, suggesting that Oman should be placed in the medium-risk zone for MS.2 MS is a chronic, inflammatory, and disabling disorder that causes demyelination in the nervous systems of young and middle-aged adults.3 This inflammatory disease is characterized by phases of exacerbation in which the symptoms are heightened and phases of symptom subsidence, where the symptoms are minimal.4 These symptoms may include sensation changes, vision problems, dysarthria, muscle weakness, imbalance, mood changes, depression, pain, fatigue, and heat intolerance.5 In addition to these symptoms, MS can influence many characteristics of a patient’s personal life and has considerable repercussions on their quality of life (QoL).6 Patients with MS need long-term treatment. One of the major goals in treating MS is to decrease the negative effects of this chronic disease on patients’ QoL.7 Health-related QoL (HRQoL) is a complicated concept in which a patient’s health is evaluated through physical, emotional, mental, and social components.8 An assessment of HRQoL is necessary to enable a better and holistic course of treatment to improve the overall QoL of the patient.5
Since objective indicators do not accurately reflect the effect of MS on a patient’s personal life, many instruments to effectively measure QoL from the patient’s perspective have been developed.8 Many HRQoL surveys for MS are available and have been extensively used. However, most of these surveys are generic instruments and not specific to MS.5 In 1992, the MS International QoL (MusiQoL) questionnaire was developed and validated in 15 countries.9 This instrument is short, self-administered, and multidimensional, and it specifically studies patients’ points of view regarding the effect of MS on their QoL.10,11 The MusiQoL has been translated into many languages, including Arabic, and has been psychometrically assessed and validated based on a standardized methodology. Previous studies from around the world have used MusiQoL to evaluate patients’ points of view on the impact of MS on their daily lives.12–15 However, to the best of our knowledge, no studies have focused on the effect of MS on HRQoL in Omani patients. Each country has unique factors, practices, beliefs, traditions, and healthcare systems, which could lead to differences in patients’ QoL.16 Therefore, there is a need for research into the HRQoL of Omani patients with MS because presently, there is no researched information about the subject.
According to the Atlas of MS 2013 map, Oman, which is part of the Arabian Gulf, is a low-risk region for MS.17 The prevalence of MS in this zone started to increase during the first decade of this century, except in Oman, which reported a low prevalence rate of 4/100 000 in 2005.18 One could therefore hypothesize that Omanis may have different genetic factors than their Arab neighbors.19 Thus, this study aims to assess the impact of MS on the HRQoL of Omani patients using the validated disease-specific self-administered MusiQoL instrument.
Methods
This cross-sectional descriptive study was carried out between April and December 2019 on 177 MS patients who attended the neurology outpatient departments of two major hospitals (Sultan Qaboos University Hospital and Khoula Hospital in Muscat, Oman. The study was approved by the Research and Ethics Committees of the College of Nursing, Sultan Qaboos University Hospital, and the Ministry of Health (REC/2017-2018/09). Participants in the study were patients who had been diagnosed with MS by the senior neurologist of these two tertiary care hospitals based on the McDonald criteria. Both male and female MS patients > 18 years who were willing to participate were included in the study. Patients perceived to have physical or mental challenges in answering the questions were excluded from the study. According to a recent hospital-based study, 15.9% is the prevalence rate of MS in Oman, and all patients are treated in tertiary care hospitals in Muscat. The study sample size was calculated using the following formula: N = Z2 P (1-P)/d2 where N is the number of samples, Z is the level of confidence (95% = 1.96), P is the prevalence (15.9%), and d is the effect size (5%).
N = (1.96)2 × 0.159 (1-0.159)/0.052 = 205, was the final sample size. We collected the patient list from the hospital registry, and a consecutive sampling method was used to approach the patients during this data collection period. The response rate was 86%.
The research instrument used was a self-reported questionnaire in Arabic consisting of three sections. Section one includes questions related to sociodemographic variables (age, gender, occupation, place of living, education level, marital status, and occupation). Section two included clinical profile (disease course – relapsing-remitting, primary progressive, or secondary progressive), disease duration, type of MS-specific therapies, visual functions, and sleep patterns. Section three is the MusiQoL part to assess HRQoL. The MusiQoL questionnaire, which comprises 31 items that describe nine dimensions. Each dimension is named according to its constitutive items, as follows: activities of daily living (eight items); psychological wellbeing (four items); symptoms (three items); relationships with friends (four items); relationships with family (three items); relationship with the healthcare system (three items); sentimental and sexual life (two items); coping (two items); and rejection (two items).9
Each item was responded to using a six-point Likert scale, where 1 = never/not at all, 2 = rarely/a little, 3 = sometimes/somewhat, 4 = often/a lot, 5 = always/very much, and 6 = not applicable. The negatively worded item scores were reversed. All dimension scores were linearly converted to a 0–100 scale, and the higher scores indicated poor HRQoL. A score of up to 20 was considered good HRQoL, a score of 20.1–60 was considered moderate HRQoL, and a score > 60 was considered poor HRQoL. Results from the validation of MusiQoL suggest that the instrument is a disease-specific instrument that is sensitive to changes in the clinical status of patients.9,20 The researchers also reported that the instrument demonstrated good internal validity and consistency, external validity, and reproducibility with a Cronbach’s alpha of 0.92.
Data was collected by research assistants who are senior registered neurology nurses and were specifically trained to collect data from MS patients. Information about patients diagnosed with MS was collected from the hospital registry. Three subtypes of MS were identified from the patient file and were defined as: ‘relapsing-remitting’, ‘secondary progressive’, and ‘primary progressive’. The selected participants were then approached in the neurology outpatient departments of the two hospitals when they came for their routine follow-up visits. After a thorough explanation of the study purpose and assurance of anonymity, as well as their confidentiality and right to withdraw at any time from the study, written informed consent was obtained from every subject involved in the study. The subjects were then interviewed in a private room by the research assistant. Participants were given the self-reported questionnaire, and the research assistant helped those who required assistance. All personal identifications of patients remained anonymous to ensure that there was no violation of privacy. Data confidentiality was maintained, and all physical data files were kept in locked cabinets in the researcher’s office. All the signed informed consent forms with the respondent’s details were stored and locked separately from the data. Confidentiality was also maintained by assigning code numbers instead of names to the data files.
SPSS Statistics (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.) was used for data entry, data cleaning, and data analysis. The data was audited for accuracy by two investigators. Normality of data was checked with the Shapiro-Wilk test before proceeding with data analysis. A p-value of < 0.050 was considered statistically significant for all tests. Descriptive summaries of sociodemographic and clinical characteristics (means, standard deviations, frequencies, and percentages) were used to describe the sample. Comparison of HRQoL scores with demographic and clinical variables was done with an independent t-test and analysis of variance (ANOVA).
Results
A total of 177 Omani patients diagnosed with MS, with a mean age of 34.71±8.69 years, participated in the study. Descriptive statistics showed that 73.4% of the patients were female. Almost half (53.7%) of the participants lived in Muscat, the capital city of Oman, and 53.7% had a university education. In addition, 61.6% were married, and 54.8% were employed. The majority (92.1%) of patients were classified as having relapsing-remitting MS, while 2.8% had primary progressive MS and 5.1% secondary progressive MS. Visual impairments were reported by 41.8% of the respondents, while 33.3% experienced sleep disturbances. Table 1 presents the demographic profile of the respondents.
Table 1: Demographic and clinical profile of participants (N = 177).
|
Age, years |
|
|
< 30 |
57 (32.2) |
|
31–50 |
108 (61.0) |
|
> 50 |
12 (6.8) |
|
Gender |
|
|
Male |
47 (26.6) |
|
Female |
130 (73.4) |
|
Place of living |
|
|
Muscat |
95 (53.7) |
|
Outside Muscat |
82 (46.3) |
|
Educational level |
|
|
Up to elementary school |
17 (9.6) |
|
High school and higher secondary |
65 (36.7) |
|
University education |
95 (53.7) |
|
Marital status |
|
|
Single |
56 (31.6) |
|
Married |
109 (61.6) |
|
Separated/divorced/widowed |
12 (6.8) |
|
Occupation |
|
|
Employed |
97 (54.8) |
|
Unemployed |
80 (45.2) |
|
Disease course |
|
|
Relapsing-remitting |
163 (92.1) |
|
Primary progressive |
5 (2.8) |
|
Secondary progressive |
9 (5.1) |
|
Type of MS-specific therapies |
|
|
Disease-modifying medicines |
150 (84.7) |
|
Disease-modifying medicines and physiotherapy |
27 (15.3) |
|
Visual functions |
|
|
Normal |
103 (58.2) |
|
Visual impairments |
74 (41.8) |
|
Sleep patterns |
|
|
Normal |
118 (66.7) |
MS: multiple sclerosis.
Table 2: Mean and standard deviation (SD) of total and component scores of health-related quality of life (HRQoL) of multiple sclerosis patients.
|
Activities of daily living |
57.4 ± 22.2 |
|
Psychological wellbeing |
60.3 ± 22.8 |
|
Symptoms |
56.6 ± 20.3 |
|
Relationship with friends |
63.1 ± 15.0 |
|
Relationship with family |
75.7 ± 24.2 |
|
Sentimental and sexual life |
52.3 ± 39.6 |
|
Coping |
49.8 ± 25.8 |
|
Rejection |
42.2 ± 25.3 |
|
Relationship with the healthcare system |
81.7 ± 18.9 |
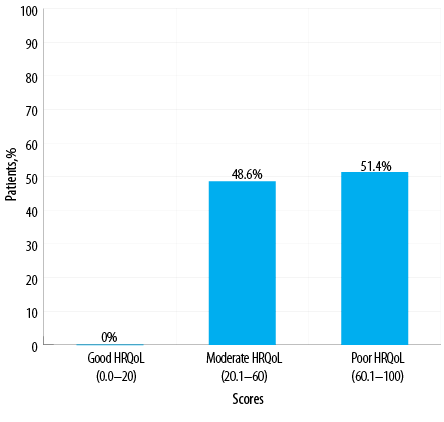
Figure 1: Percentage of patients with multiple sclerosis based on their health-related quality of
life scores (HRQoL).
The mean duration of the disease was 6.6±4.57 years. Over half (51.4%) of the respondents had poor HRQoL (60.1–100 scores), while 48.6% of them had moderate HRQoL (20.1–60 scores). Surprisingly, no patient had a good HRQoL (0–20 scores) (Figure 1).
The total mean score of the HRQoL of the respondents was 60.6±11.4 [Table 2]. The relationship with the healthcare system and relationship with family was the most affected components, with mean scores of 81.7±18.9 and 75.7±24.2, respectively. The least affected subscale was rejection, with a mean score of 42.2±25.3.
Table 3 illustrates the comparison of means of HRQoL and gender. Females reported a poor HRQoL in total and the components of HRQoL. Statistically significant differences were seen with psychological wellbeing (t = -2.353, df = 175,
p = 0.020), coping (t = 2.630, df = 175, p = 0.009), and total HRQoL (t = -2.145, df = 175, p = 0.033), with males having better HRQoL. The relationship between HRQoL components and other demographic variables did not show any statistically significant differences.
Table 3: Comparison of HRQoL scores of MS patients based on gender.
|
Activities of daily living |
|
Male |
47 |
55.6 ± 23.2 |
-0.660 |
0.510 |
|
Female |
130 |
58.1 ± 21.8 |
|
|
|
Psychological wellbeing |
|
Male |
47 |
53.7 ± 22.2 |
-2.353 |
0.020 |
|
Female |
130 |
62.7 ± 22.6 |
|
|
|
Symptoms |
|
Male |
47 |
53.4 ± 17.9 |
-1.266 |
0.207 |
|
Female |
130 |
57.8 ± 21.0 |
|
|
|
Relationship with friends |
|
Male |
47 |
61.1 ± 14.3 |
-1.040 |
0.300 |
|
Female |
130 |
63.8 ± 15.3 |
|
|
|
Relationship with family |
|
Male |
47 |
73.2 ± 25.7 |
-0.844 |
0.400 |
|
Female |
130 |
76.7 ± 23.6 |
|
|
|
Sentimental and sexual life |
|
Male |
47 |
53.2 ± 40.8 |
0.188 |
0.851 |
|
Female |
130 |
51.9 ± 39.3 |
|
|
|
Coping |
|
Male |
47 |
41.5 ± 22.5 |
-2.630 |
0.009 |
|
Female |
130 |
52.9 ± 26.3 |
|
|
|
Rejection |
|
Male |
47 |
42.6 ± 26.2 |
0.128 |
0.898 |
|
Female |
130 |
42.0 ± 25.0 |
|
|
|
Relationship with the healthcare system |
|
Male |
47 |
77.6 ± 22.6 |
-1.731 |
0.085 |
|
Female |
130 |
83.1 ± 17.2 |
|
|
|
Total HRQoL |
|
Male |
47 |
57.5 ± 11.8 |
-2.145 |
0.033 |
HRQoL: health-related quality of life; MS: multiple sclerosis; SD: standard deviation.
Table 4: Association of total HRQoL of MS patients with their demographic and clinical characteristics.
|
Age, years |
| |
|
|
|
|
|
|
< 30 |
57 |
56.7 ± 11.1 |
2,174 |
5.107 |
0.007 |
|
31–50 |
108 |
62.5 ± 10.8 |
|
|
|
|
> 50 |
12 |
61.7 ± 14.4 |
|
|
|
|
Marital status |
| |
|
|
|
|
|
|
Single |
56 |
56.7 ± 10.7 |
3,173 |
4.155 |
0.007 |
|
Married |
109 |
61.8 ± 11.0 |
|
|
|
|
Separated/divorced/widowed |
12 |
66.9 ± 12.0 |
|
|
|
|
Visual functions |
|
|
|
|
|
|
Normal |
103 |
58.8 ± 11.5 |
1,175 |
6.236 |
0.013 |
|
Impairments |
74 |
63.0 ± 10.9 |
|
|
|
|
Sleep patterns |
| |
|
|
|
|
|
|
Normal |
118 |
58.5 ± 11.3 |
1,175 |
12.620 |
<0.001 |
HRQoL: health-related quality of life; MS: multiple sclerosis; SD: standard deviation; df: degree of freedom.
The results of the ANOVA of the demographic and clinical variables with the total mean scores of HRQoL of MS patients are presented in Table 4. Only significant results are presented in the table. The results suggest a significant difference between total HRQoL scores and age groups (F (2,174) = 5.107, p = 0.007), marital status (F(3,173) = 4.155, p = 0.007), sleep pattern (F(1,175) = 12.620, p < 0.001), and visual functions (F(1,175) = 6.236, p = 0.013). Post-hoc analysis revealed age group > 31 years old, being separated, divorced, or widowed, group perceived poor HRQoL than others. Being female, and having sleep and visual disturbances are associated with poor HRQoL scores.
Discussion
The MusiQoL questionnaire was used to assess the respondents’ MS-specific HRQoL. To our best knowledge, this study is the first to investigate the HRQoL of Omani patients with MS using this valid and reliable questionnaire. We found that being > 30 years, female, married, separated, widowed, or divorced, and having visual and sleep problems were significantly associated with poorer HRQoL. Among the different HRQoL components, relationship with the healthcare system and relationship with family and friends were the most negatively affected as a result of the disease process. Our results also showed that psychological wellbeing and coping domains of MusiQoL questionnaires are significantly reduced in females compared to males.
The MusiQoL instrument is the best to use in our setting because it has been validated in 14 languages, including Arabic, and the differential item functioning was found to be satisfactory in more than 15 countries around the world.9 The use of this questionnaire is suitable for international settings, and such use can be beneficial for comparing different populations. The MusiQoL instrument has the advantage of being shorter than other instruments and more suitable for clinical practice.13 It is well known that HRQoL is affected by the population’s different cultural backgrounds and healthcare systems.
All patients had a high MusiQoL score that fell in the moderate to low HRQoL category. This result can be explained by the fact that over 90% of the studied population suffers from the relapse-remitting MS subtype. Studies have shown that the worst level of HRQoL is observed in patients with relapse-remitting MS.12 Similarly, other studies have revealed that the more progressive the disease course, the poorer the HRQoL for the MS patient.21 However, in our study, the low percentage (> 8%) of patients with progressive disease did not allow us to compare the HRQoL between the three different disease courses.
The study found that patients with MS showed a low level of HRQoL in the components of the relationship with the healthcare system, family, and friends. This, therefore, implies that having MS affects interpersonal relationships with family and friends. In addition, studies have shown that social support is an important component that can help improve HRQoL in MS patients. Interestingly, while all support is important, psychological support to the MS patient appears to be more required than material support in all dimensions of HRQoL.22 Hence, understanding which components greatly affect patients with MS will allow us to develop strategies to mitigate their effect and positively affect HRQoL.
Comparison of means among the categories of sociodemographic characteristics showed that older adults, females, those who are separated, divorced, or widowed, and patients with visual and sleep problems have poorer HRQoL. This result supports the findings of many other studies that also showed that younger age (< 30 years) and being a male were significantly linked to a better HRQoL in similar studies conducted using MusiQoL instrument.13,23,24
We also found that the patient’s marital status played a significant role in affecting their total HRQoL. Being single was associated with higher HRQoL levels. Being married was associated with a lower HRQoL while being divorced, separated, or widowed had the lowest scores. This result appears to contradict the findings of previous studies, which showed that being married was associated with higher HRQoL levels.10,25 For instance, a study of 1992 patients from 15 countries reported that patients with MS who have partners had significantly higher HRQoL than single patients.13 In trying to better understand the possible explanation for this difference, we noted that all these previous studies asked respondents whether they were ‘single’ or ‘not single’. It is possible that a separated, divorced, or widowed person would answer as single; therefore, the differentiation between single and separated, widowed, or divorced may not have been as clear to their respondents. This could have influenced the results and increased the score for the ‘single’ component. In our study, we can argue that a single patient who has never been married has the highest HRQoL. A married patient probably has more responsibilities and, therefore, has a lower HRQoL, while a separated, divorced, or widowed patient lacks the family support they once had, and this easily shows as having the lowest HRQoL. Omani patients with MS showed a low HRQoL dimension of relationship with family, which could also explain the aforementioned association.
The present study showed poor HRQoL perception among MS patients with sleep and vision disturbances. Other researchers support this finding.26,27 Increased levels of inflammatory cytokines or lesions in the brain may disrupt pathways involved with sleep which may contribute to sleep disruption in MS patients.28 Visual disturbances in MS patients need to be considered in the light of falls, which are commonly reported among them.29 These findings highlight the importance of carefully screening all patients with MS for the presence of sleep and visual problems so that a variety of strategies to reduce the effects of these problems on the HRQoL are implemented promptly. Future research on sleep quality in MS should consider exploring sleep disturbance, particularly its relationship with disease activity. Vision rehabilitation may be required for patients experiencing visual difficulties in the course of the disease progression. Therefore, it is important to use a holistic interdisciplinary approach to address the person’s needs with MS.
In the present study, educational level, employment status, disease course, and MS-specific therapy did not show any difference in perception of HRQoL. Unlike other study populations,10 Omani MS patients who have a higher level of education do not have a better HRQoL. This could be because only slightly < 10% of the studied sample did not have a high school or university education. In addition, our results do not show a higher HRQoL among employed MS patients when compared to the unemployed patients, contrary to other studies.30 This observation could be unique to the Omani population and may be associated with the society and particular characteristics of Omani MS patients.
When examining demographic variables, we found that only gender exhibits differences in some MusiQoL dimensions. Other sociodemographic variables did not affect the different component scales of the MusiQoL questionnaire. We found that the HRQoL of males is somewhat higher than that of females but only for two MusiQoL domains. Both psychological wellbeing and coping scores were higher for women than men, which means better functions for the latter. As a mediator between MS and psychological wellbeing, coping is an important domain to be assessed. As MS advances, coping becomes of paramount importance to the patient’s psychological wellbeing.24 Studies have shown that emotional and psychological functions are lower in women with MS than in men.13,30 The finding that coping and psychological wellbeing appear to negatively impact females more than males must be further explored to understand the reasons for these differences among the genders. One possible reason in our setting is that Oman is a patriarchal society whose culture places high expectations on men, who should show physical and mental ability, power, efficiency, and productivity. These findings are very important in developing coping strategies targeting Omani men and women with MS who could benefit from a psychological rehabilitation program. Studies suggest that patients should change their lifestyles, ambitions, and expectations from their physical performances and adapt themselves to live with the disability to better cope with MS.31
Eye examinations in the early stages to prevent diminishing visual acuity, sleep clinics to empower them with strategies to overcome their sleep disturbances, and psychological counseling with family support can play an important role in improving the HRQoL of these patients living with MS.
Several limitations of our study should be examined. First, the size of the studied population is relatively small, and additional research with a larger sample of Omani patients is necessary to confirm our results. Second, our study did not assess fatigue, depression, anxiety, and other major symptoms like pain, bladder/bowel symptoms, and disability, which have been shown to affect HRQoL.6,32 It is recommended that future research on the observation of all the major symptoms experienced by these patients could be assessed. Another limitation is the cross-sectional study design, which does not allow us to interpret the associations as causal relationships. Only a longitudinal study can better understand the course of MS and the coping mechanisms in Omani patients.
Understanding the HRQoL of MS patients will help healthcare providers to assess their patients and treat them better. This research will help patients with MS who have not been coping well with their disease be better identified, treated, and referred to counselors when deemed necessary. The results of this study will contribute to the limited body of literature on Omani patients with MS and allow us to develop strategies for improving their HRQoL. Such information will aid stakeholders, including the Ministry of Health of Oman, to plan strategies to improve their HRQoL to ease the burgeoning load of this disease to the Omani society.
Conclusion
Poor HRQoL has been reported by Omani patients with MS in our study. We found that being > 30 years, female, married, separated, widowed, or divorced, and having visual and sleep problems resulted in poorer HRQoL scores. Moreover, relationships with the health care system and family and friends most negatively affect patients’ HRQoL. Understanding these results is of paramount importance to the Omani health care system to design a more comprehensive approach to more effectively care for Omani patients with MS. Understanding factors influencing HRQoL among people with MS is helpful for the health care workers to design early intervention programs.
Disclosure
The authors declared no conflicts of interest. The study was funded by the internal grants of Sultan Qaboos University with ethical approval #REC/2017-2018/09.
Acknowledgements
The authors would like to acknowledge the research assistants Ms. Reem Rashid Al Habsi and Ms. Ms. Suhair Hamood
Al Alawi who helped in data collection in both hospitals and the patients who volunteered to participate in the study.
references
- 1. Thompson AJ, Baranzini SE, Geurts J, Hemmer B, Ciccarelli O. Multiple sclerosis. Lancet 2018 Apr;391(10130):1622-1636.
- 2. Al Senani M, Al Salti A, Al Khabouri J, Elyas ME, Gujjar AR, Ramachandiran N, et al. Incidence and prevalence of multiple sclerosis in the Sultanate of Oman: a hospital based study. Mult Scler Relat Disord 2020;37.
- 3. Salhofer-Polanyi S, Friedrich F, Löffler S, Rommer PS, Gleiss A, Engelmaier R, et al. Health-related quality of life in multiple sclerosis: temperament outweighs EDSS. BMC Psychiatry 2018 May;18(1):143.
- 4. Compston A, Coles A. Multiple sclerosis. Lancet 2008 Oct;372(9648):1502-1517.
- 5. Opara JA, Jaracz K, Brola W. Quality of life in multiple sclerosis. J Med Life 2010 Oct-Dec;3(4):352-358.
- 6. Mitchell AJ, Benito-León J, González JM, Rivera-Navarro J. Quality of life and its assessment in multiple sclerosis: integrating physical and psychological components of wellbeing. Lancet Neurol 2005 Sep;4(9):556-566.
- 7. Kargiotis O, Paschali A, Messinis L, Papathanasopoulos P. Quality of life in multiple sclerosis: effects of current treatment options. Int Rev Psychiatry 2010;22(1):67-82.
- 8. Olascoaga J. [Quality of life and multiple sclerosis]. Rev Neurol 2010 Sep;51(5):279-288.
- 9. Simeoni M, Auquier P, Fernandez O, Flachenecker P, Stecchi S, Constantinescu C, et al; MusiQol study group. Validation of the multiple sclerosis international quality of life questionnaire. Mult Scler 2008 Mar;14(2):219-230.
- 10. Michel P, Baumstarck K, Ghattas B, Pelletier J, Loundou A, Boucekine M, et al. A multidimensional computerized adaptive short-form quality of life questionnaire developed and validated for multiple sclerosis: the MusiQoL-MCAT. Medicine (Baltimore) 2016 Apr;95(14):e3068.
- 11. Moore F, Vickrey B, Fortin K, Lee L. Two multiple sclerosis quality-of-life measures: comparison in a national sample. Can J Neurol Sci 2015 Jan;42(1):55-63.
- 12. Beiske AG, Baumstarck K, Nilsen RM, Simeoni MC. Validation of the multiple sclerosis international quality of life (MusiQoL) questionnaire in Norwegian patients. Acta Neurol Scand 2012 Mar;125(3):171-179.
- 13. Fernández O, Fernández V, Baumstarck-Barrau K, Muñoz L, Gonzalez Alvarez MdelM, Arrabal JC, et al; MusiQoL study group of Spain. Validation of the spanish version of the multiple sclerosis international quality of life (Musiqol) questionnaire. BMC Neurol 2011 Oct;11 (1):127.
- 14. Jamroz-Wiśniewska A, Stelmasiak Z, Bartosik-Psujek H. Validation analysis of the polish version of the multiple sclerosis international quality of life questionnaire (MusiQoL). Neurol Neurochir Pol 2011 May-Jun;45(3):235-244.
- 15. Thumboo J, Seah A, Tan CT, Singhal BS, Ong B. Asian adaptation and validation of an English version of the multiple sclerosis international quality of life questionnaire (MusiQoL). Ann Acad Med Singap 2011 Feb;40(2):67-73.
- 16. Pluta-Fuerst A, Petrovic K, Berger T, Fryze W, Fuchs S, Gold R, et al. Patient-reported quality of life in multiple sclerosis differs between cultures and countries: a cross-sectional Austrian-German-Polish study. Mult Scler 2011 Apr;17(4):478-486.
- 17. Browne P, Chandraratna D, Angood C, Tremlett H, Baker C, Taylor BV, et al. Atlas of multiple sclerosis 2013: a growing global problem with widespread inequity. Neurology 2014 Sep;83(11):1022-1024.
- 18. Tharakan JJ, Chand RP, Jacob PC. Multiple sclerosis in Oman. Neurosciences (Riyadh) 2005 Jul;10(3):223-225.
- 19. Yamout BI, Assaad W, Tamim H, Mrabet S, Goueider R. Epidemiology and phenotypes of multiple sclerosis in the Middle East North Africa (MENA) region. Mult Scler J Exp Transl Clin 2020 Jan;6(1):2055217319841881.
- 20. Triantafyllou N, Triantafillou A, Tsivgoulis G. Validity and reliability of the Greek version of the multiple sclerosis international quality-of-life questionnaire. J Clin Neurol 2009 Dec;5(4):173-177.
- 21. Rezapour A, Almasian Kia A, Goodarzi S, Hasoumi M, Nouraei Motlagh S, Vahedi S. The impact of disease characteristics on multiple sclerosis patients’ quality of life. Epidemiol Health 2017 Feb;39:e2017008.
- 22. Costa DC, Sá MJ, Calheiros JM. The effect of social support on the quality of life of patients with multiple sclerosis. Arq Neuropsiquiatr 2012 Feb;70(2):108-113.
- 23. Turpin KV, Carroll LJ, Cassidy JD, Hader WJ. Deterioration in the health-related quality of life of persons with multiple sclerosis: the possible warning signs. Mult Scler 2007 Sep;13(8):1038-1045.
- 24. Pfaffenberger N, Pfeiffer KP, Deibl M, Höfer S, Günther V, Ulmer H. Association of factors influencing health-related quality of life in MS. Acta Neurol Scand 2006 Aug;114(2):102-108.
- 25. Baumstarck K, Pelletier J, Butzkueven H, Fernandez O, Flachenecker P, Idiman E, et al. Health-related quality of life as an independent predictor of long-term disability for patients with relapsing-remitting multiple sclerosis. European Journal of Neurology 2013;20(6):907-914.
- 26. Merlino G, Fratticci L, Lenchig C, Valente M, Cargnelutti D, Picello M, et al. Prevalence of ‘poor sleep’ among patients with multiple sclerosis: an independent predictor of mental and physical status. Sleep Med 2009 Jan;10(1):26-34.
- 27. Tabrizi FM, Radfar M. Fatigue, sleep quality, and disability in relation to quality of life in multiple sclerosis. Int J MS Care 2015 Nov-Dec;17(6):268-274.
- 28. Kaminska M, Kimoff RJ, Benedetti A, Robinson A, Bar-Or A, Lapierre Y, et al. Obstructive sleep apnea is associated with fatigue in multiple sclerosis. Mult Scler 2012 Aug;18(8):1159-1169.
- 29. Nilsagård Y, Denison E, Gunnarsson LG, Boström K. Factors perceived as being related to accidental falls by persons with multiple sclerosis. Disabil Rehabil 2009;31(16):1301-1310.
- 30. Miller A, Dishon S. Health-related quality of life in multiple sclerosis: the impact of disability, gender and employment status. Qual Life Res 2006 Mar;15(2):259-271.
- 31. Casetta I, Riise T, Wamme Nortvedt M, Economou NT, De Gennaro R, Fazio P, et al. Gender differences in health-related quality of life in multiple sclerosis. Mult Scler 2009 Nov;15(11):1339-1346.
- 32. Amato MP, Ponziani G, Rossi F, Liedl CL, Stefanile C, Rossi L. Quality of life in multiple sclerosis: the impact of depression, fatigue and disability. Mult Scler 2001 Oct;7(5):340-344.