Coronavirus disease 2019 (COVID-19), which is declared a global pandemic by the World Health Organization, usually presents with fever, cough, shortness of breath, and myalgia. Headache, diarrhea, and sore throat have also been reported, although less frequently. One of the major complications other than acute respiratory distress syndrome is the hypercoagulable state leading to vascular thrombotic complications. We report a case of a patient with COVID-19 who presented with an acute abdomen. Further investigation with computed tomography (CT) revealed superior mesenteric artery thrombosis leading to bowel ischemia.

Figure 1: Selected sagittal reformat of the abdominal CT scan showing thrombus in the main super mesenteric artery and one of its major branches (red arrows). Some of the small bowel loops are not enhancing, indicating established bowel ischemia (red asterisks).
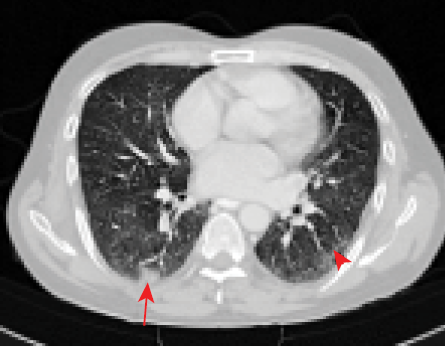
Figure 2: Mild focal consolidation in the superior segment of the right lower lobe (red arrow). Focal scar with surrounding ground-glass density at the superior segment of the left lower lobe (arrowhead). Both findings are described lung changes of COVID-19 infection.
Case report
A 51-year-old male patient presented to the emergency department with acute abdominal pain and nausea. He was diagnosed with COVID-19 one week before and was kept in home isolation. On examination, he was afebrile and clinically stable without any signs of respiratory distress with 100% saturation in room air. He was a non-smoker and without any previous history of peripheral arterial disease. Further work-up with CT angiogram showed superior mesenteric artery thrombosis with resultant bowel ischemic signs [Figure 1] with typical covid lung changes [Figure 2]. D-dimer was 2.5 mcg/mL and ferritin level was 687ng/mL. He was operated on for urgent laparotomy and thrombectomy. Intraoperatively, we found that around 45 cm of his jejunum was gangrenous, which was subsequently resected. At the end of the surgery, the abdomen was not closed, and he was moved to the intensive care unit (ICU) for elective mechanical ventilation. He was started on heparin infusion, which was titrated according to institution protocol. Good hydration was maintained, and his vitals were normal throughout his stay in ICU. He underwent two re-look laparotomies where another 10 cm of the gangrenous segment of his jejunum was again resected, and jejunocolic anastomosis was done. His superior mesenteric artery flow was found to be good. After a third laparotomy and abdominal closure, he was extubated and taken to the high dependency unit after six days in the ICU. He was later moved to the ward, where he had a long hospital stay of almost forty days before getting discharged. At the time of discharge, he had recovered completely and was advised follow-up on an outpatient basis.
Discussion
The most common presentation of COVID-19 is respiratory. But with new emerging data, it seems it can present various other complications like hypercoagulable state with venous and arterial thrombosis, which is prognostic of poorer outcomes.1,2 Venous thrombosis occurs more frequently than arterial. Among arterial thrombotic presentations, coronary and lower limb complications are well reported.3
The mechanism of thrombosis in COVID-19 cases can be attributed to various theories, which include a severely heightened inflammatory response that leads to thromboinflammation through mechanisms such as cytokine storm, complement activation, and endotheliitis.4 Excessive cytokine release contributes to thrombosis through multiple mechanisms, including activation of monocytes, neutrophils, and the endothelium, all of which generate a prothrombotic state.
In a series of 150 ICU patients, four arterial occlusions were observed, of which one caused mesenteric ischemia, one limb ischemia, and two cases of cerebral ischemia.5 In a retrospective review of case series involving the presentation of acute abdomen and worsening of COVID-19 symptoms, early abdominal CT was advocated.6
Laboratory findings usually include elevated D-dimer with normal prothrombin time and activated partial thromboplastin time.6 The recommended treatment modality is intravenous or subcutaneous use of low molecular heparin or unfractionated heparin and dosing based on coagulation parameters or clinical scenarios.
In our case, the patient had no other comorbidities or known hematological disorders. All other baseline investigations were normal, including echocardiography. CT angiogram as a part of investigation protocol helped arrive at a diagnosis, which helped in early intervention.
Conclusion
A hypercoagulable state in COVID-19 is emerging as a major pathological occurrence with serious consequences in mortality and morbidity. Therefore, the complication arising out of the hypercoagulable state must be kept in mind while treating COVID-19 cases, even in patients with mild symptoms or in the post-COVID recovery phase.
Disclosure
All authors declared no conflicts of interest. The authors certify that they have obtained all appropriate patient consent form. In the form, the patient has given his consent for his images and clinical information to be reported in the journal. The patient understands that his name and initial will not be published, and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
references
- 1. ZhouF, YuT, DuR, FanG, LiuY, LiuZ, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study.Lancet2020 Mar;395(10229):1054-1062.
- 2. TangN, LiD, WangX, SunZ. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia.J ThrombHaemost2020 Apr;18(4):844-847.
- 3. GargK, BarfieldME, PezoldML, SadekM, CayneNS, LugoJ, et al. Arterial thromboembolism associated with COVID-19 and elevated D-dimer levels.J VascSurg Cases Innov Tech2020 Jun;6(3):348-351.
- 4. HuangC, WangY, LiX, RenL, ZhaoJ, HuY, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China.Lancet2020 Feb;395(10223):497-506.
- 5. HelmsJ, TacquardC, SeveracF, Leonard-LorantI, OhanaM, DelabrancheX, et al; CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis). High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study.Intensive Care Med2020 Jun;46(6):1089-1098.
- 6. IgnatM, PhilouzeG, Aussenac-BelleL, FaucherV, CollangeO, MutterD, et al. Small bowel ischemia and SARS-CoV-2 infection: an underdiagnosed distinct clinical entity.Surgery2020 Jul;168(1):14-16.