Uterine fibroids are the most common benign smooth muscle tumor of the uterus in women of reproductive age, affecting 30–70% of women in this age group.1 The effects of pregnancy on fibroid and fibroids on pregnancy are a clinical concern.
African women are three times more likely to develop fibroids suggesting a genetic predisposition. The incidence of uterine fibroids rises with increasing age. Uterine fibroids have a prevalence of 0.1–10.7% in pregnancy and are associated with a 10–40% obstetric complication rate.1
The growth of fibroids during pregnancy is not linear; most of the growth occurs in the first trimester with little or no increase during the second and third trimesters.2 Large fibroids (> 5 cm in diameter) are more likely to grow during pregnancy and cause adverse obstetric outcomes.3
The size, location, and multiplicity of fibroids appear to be risk factors for pregnancy complications. Larger size, retroplacental location, and distortion of the uterine cavity are characteristics that have been associated with an increased risk of miscarriage, placental abruption, fetal growth restriction, hemorrhage, and preterm labor and birth.4,5 Cesarean section (CS) rates are higher, mainly due to obstructed labor and malpresentation.6,7
As there is limited information available on the prevalence and impact of fibroids on pregnancy outcomes and no specific study to date in Oman addressing this issue, this study is of great relevance to Oman to make specific recommendations regarding follow-up and management of pregnant women with fibroids throughout the antenatal and intrapartum period.
The primary objective of the present study was to assess the overall prevalence of fibroids complicating pregnancy in Omani women followed up and delivered at Sultan Qaboos University Hospital (SQUH). The secondary objective was to correlate the size (> 5 cm) and location of fibroids with maternal complications and neonatal outcomes in these women.
Methods
This was a retrospective cohort study conducted in the Obstetrics and Gynecology Department at SQUH, a tertiary referral and teaching hospital in Oman, from 1 January 2011 to 31 December 2016. Ethical approval was obtained from the hospital ethical committee (MREC Approval #1991).
All women with singleton gestation who had uterine fibroids identified on routine obstetric ultrasonography during the first or second trimester were included. Age-matched women without uterine fibroids following the index cases delivering at SQUH were randomly selected as controls over the same period of study in a 1:2 ratio. Exclusion criteria for women without uterine fibroids were induction of labor, elective cesarean section, and multiple gestation. Data was collected from the obstetric ultrasonography database, maternity register, operating theatre register, and hospital information system. Demographic data and clinical characteristics included maternal age, gravidity, parity, body mass index (BMI), past medical history, and previous preterm delivery. Ultrasonographic data included the total number of fibroids, diameter of the largest fibroids, number of fibroids > 5 cm in diameter, and the location of these fibroids. The main obstetric outcome measures in this study were preterm delivery (< 37 weeks), preterm premature rupture of membranes (PPROM), malpresentation, intrauterine growth restriction (IUGR), mode of delivery, postpartum hemorrhage (PPH) (estimated blood loss of > 500 mL following vaginal delivery and > 1 L following cesarean section), retained placenta, and cesarean myomectomy. Fetal outcomes included were infant birth weight and Apgar score at one and five minutes. Data was analyzed using SPSS Statistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). Chi-square test and independent sample t-test were used to calculate significant outcomes. A p-value of < 0.050 was considered statistically significant.
Results
A total of 62 women with singleton gestation had uterine fibroids documented on routine obstetric ultrasonography during the study period. The total number of deliveries were 24 800, giving a prevalence of 0.3%.
Table 1: Demographic data of women with large fibroids and women with no fibroids.
|
Age, mean ± SD |
32.6 ± 4.2 |
31.0 ± 4.4 |
0.057 |
|
Gravidity, median
(min–max) |
1 (1–8) |
3 (1–9) |
|
|
Parity, median
(min–max) |
0 (0–5) |
2 (0–7) |
|
SD: standard deviation; BMI: body mass index.
Of the 62 women with sonographically identified uterine fibroids, 41 had large uterine fibroids (size > 5 cm). These women had a mean age of 32.6 years with median gravidity of 1 and parity 0. Compared to women with no uterine fibroids (n = 88), women with large uterine fibroids were not statistically different with respect to age, BMI, and history of preterm labor [Table 1]. No statistically significant difference was seen among women with large uterine fibroids compared to those with no fibroids with respect to preterm labor, PPROM, malpresentation, retained placenta, and IUGR (p > 0.050). Women with large uterine fibroids had a significantly higher rate of PPH (n = 8; 19.5%) compared to those with no fibroid (n = 4, 4.5%), p = 0.018. The commonest cause of PPH was uterine atony (p = 0.007). Sixteen (41.0%) women with large uterine fibroids underwent CS compared to 13 (14.8%) women with no fibroids (p = 0.002). Normal vaginal delivery occurred in 75 (85.2%) women with no fibroids compared to 21 (52.5%) women with large fibroids (p < 0. 001). Five (12.8%) women with large uterine fibroids underwent cesarean myomectomy (p = 0.002) [Table 2 and Figure 1] The main indication for CS was obstructed labor (n = 10, 62.5%) followed by fetal distress (n = 3 , 18.8%). The rate of malpresentation was 2 (12.5%). Three (18.8%) women had CS due to previous myomectomy and CS.
Table 2: Maternal outcomes in women with large fibroids (> 5 cm) and those with no uterine fibroids.
|
Preterm labor |
|
Yes |
3 (7.3) |
3 (3.4) |
0.381 |
|
No |
38 (92.7) |
85 (96.6) |
|
PPROM |
|
Yes |
1 (2.4) |
1 (1.1) |
0.536 |
|
No |
40 (97.6) |
87 (98.9) |
|
Malpresentation |
|
Yes |
2 (4.9) |
1 (1.1) |
0.237 |
|
No |
39 (95.1) |
87 (98.9) |
|
IUGR |
|
Yes |
10 (24.4) |
9 (10.2) |
0.059 |
|
No |
31 (75.6) |
79 (89.8) |
|
PPH |
|
Yes |
8 (19.5) |
4 (4.5) |
0.018* |
|
No |
33 (80.5) |
84 (95.5) |
|
NVD |
|
Yes |
21 (52.5) |
75 (85.2) |
< 0.001* |
|
No |
19 (47.5) |
13 (14.8) |
|
CS |
|
Yes |
16 (41.0) |
13 (14.8) |
0.002* |
|
No |
23 (59.0) |
75 (85.2) |
|
CS + myomectomy |
|
Yes |
5 (12.8) |
0 (0.0) |
0.002* |
|
No |
34 (87.2) |
88 (100) |
|
Atony uterus |
|
Yes |
7 (18.9) |
3 (3.4) |
0.007* |
|
No |
30 (81.1) |
85 (96.6) |
|
Retained placenta |
|
Yes |
1 (2.7) |
0 (0.0) |
PPROM: preterm premature rupture of membranes; IGUR: intrauterine growth restriction; PPH: postpartum hemorrhage; NVD: normal vaginal delivery; CS: cesarean section.
*Statistically significant.
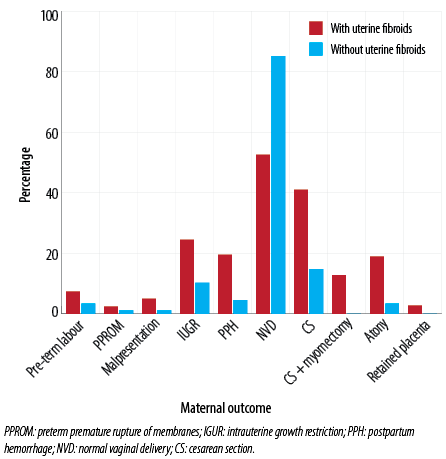
Figure 1: Maternal outcomes in women with large fibroids (> 5 cm) and those with no uterine fibroids.
Regarding neonatal outcome, the mean neonatal weight in women with large uterine fibroids and no fibroids were comparable at 2.9 and 3.0 kg, respectively (p = 0.147). The mean Apgar score at 1 and 5 minutes in women with large fibroids was 8.0 and 9.6, respectively, compared to those with no fibroids, 8.9 and 9.9, respectively. Both were statistically significant (p = 0.010 and 0.015). neonatal intensive care unit admission rates were not significantly different [Table 3].
Table 3: Neonatal outcomes in women with large uterine fibroids and those with no uterine fibroids.
|
Weight,
mean ± SD, kg |
2.9 ± 0.5 |
3.0 ± 0.4 |
0.147 |
|
1 min Apgar score, mean ± SD |
8.0 ± 1.9 |
8.9 ± 0.5 |
0.010* |
|
5 min Apgar score, mean ± SD |
9.6 ± 0.7 |
9.9 ± 0.1 |
0.015* |
|
Admission to NICU, n (%) |
|
Yes |
2 (4.9) |
2 (2.3) |
SD: standard deviation; NICU: neonatal intensive care unit.
*Statistically significant.
Most of the large uterine fibroids were located on the anterior uterine wall (n = 27, 65.9%) and posterior (n = 8, 19.5%). Six (14.6%) were located in the lower uterine segment, lateral uterine wall, and cervix.
Based on the sample size and proportion of CS (primary outcome) in both groups, the observed power (post-hoc power) is 87.3%.
Discussion
Fibroids are the most common pelvic tumors in pregnancy. The reported incidence of fibroids in pregnancy ranges from 0.1–10.7% of all pregnancies and increases with age.8,9 The prevalence of uterine fibroids complicating pregnancy over the study period was 0.3%.
Fibroids are associated with advanced maternal age and subfertility.5,10 Aromatase in fibroid tissue allows for endogenous production of estradiol, and fibroid stem cells express estrogen and progesterone receptors that facilitate tumor growth in the presence of these hormones.11 In our study, 16 women with large uterine fibroids were aged > 35 years. The median parity was 0, and this was statistically significant, which could be explained by the increased miscarriage rate due to distortion of uterine cavity in these women. Klatsky et al,6 reported an increased risk of miscarriage in women with uterine fibroids compared to women without fibroids.
Complications of fibroids in pregnancy occurred more commonly with larger fibroids (> 5 cm in size), including preterm labor, placental abruption, and CS.5,12 Hence, we did not include pregnant women with small fibroids (< 5 cm).
Fibroids are responsible for bleeding after delivery by mechanically interfering with the contractility of muscle fibers, which impact the overall contractility of the uterus.13 Fibroids located in the lower uterine segment are especially associated with a higher CS rate and retained placenta.8,14 Cervical fibroids can lead to failure of fetal head engagement and malpresentation.5
Table 4: Summary of different studies that evaluated maternal outcomes in women with fibroids.
|
Klatsky et al,6 |
2008 |
|
2098/4322 (48.4%) |
87/3535 (2.5%) |
116/721
(16.1%) |
123/1247
(9.9%) |
112/961
(11.7%) |
466/3585 (13%) |
15/1069 (1.4%) |
|
Mollica et al,12 |
1996 |
88 |
34.1% |
- |
21.6% |
22.7% |
4.5% |
- |
- |
|
Shavell et al,15 |
2012 |
42 |
- |
- |
Yes (mean 36.5 weeks) |
14.3% |
- |
- |
- |
|
Radhika et al,1 |
2015 |
15 |
- |
41.6% |
26.6% |
6.6% |
33.3% |
- |
- |
CS: cesarean section; PPH: postpartum hemorrhage; PTL: preterm labor; PPROM: preterm premature rupture of membranes; FGR: fetal growth restriction; SQUH: Sultan Qaboos University Hospital.
Table 4 summarizes the studies by different authors with the number of cases and maternal outcomes. In our study, the incidence of preterm labor was 7.3%, which is much lower than the incidence of 16.1–26.6% reported by other authors. The incidence of PPROM was also significantly lower at 2.4% compared to 6.6–22.7% reported in other studies. Malpresentations were seen in 4.9% of our study group compared to 13% as per Klastky et al.6 The incidence of retained placenta was similar. In our study, the incidence of fetal growth restriction was 24.4% compared to 11.7–33.3% in other studies. Regarding mode of delivery, the CS rate in our study group was 41.0% compared to 34.1–48.4% in other studies.
We found a statistically significant increase in the rate of PPH, secondary to atonic uterus with blood loss ranging from 900–3000 mL. All cases were managed with uterotonic medications. Around 30% required blood transfusion and other blood products.
We also found an increased rate of CS (41.0%), the main indication being obstructed labor in 62.5%, which is probably because large uterine fibroids interfere with descent of the head and cervical dilation, prolonging labor. This is supported by Klastksy et al,6 who quoted a CS rate of 48.4%. Deveer et al,16 reported a cesarean rate of 56%, and the leading indication was malpresentation followed by previous section and labor dystocia.
A growing body of evidence suggests that myomectomy undertaken at the time of CS is safe and cost-effective in selected cases.17 Fibroids causing difficulty in the closure of the uterine incision, myomectomy to facilitate safe delivery of the fetus, and large subserous fibroids > 6 cm in diameter are indications for this procedure.7,18–20 In our study, all cases who underwent CS myomectomy had either large cervical fibroids or lower segment uterine fibroids, ranging in size from 8–10 cm. All these cases had preoperative bilateral uterine balloon catheter placement to minimize blood loss, adequate blood products, and uterotonics available. Only two cases had a blood loss of 1200 mL; the others had a blood loss between 600–800 mL. None of the cesarean myomectomy patients had any postoperative complications and were discharged on the fourth or fifth postoperative day.
Mollica et al,12 concluded that around 9.1% of newborns had a birth weight < 2.5 kg. There was no statistically significant difference in the mean birth weight between the two groups in our study. This could most probably be explained by the placenta being located away from the fibroids. Hence, there was no impact on fetal blood flow nor distortion of the uterine cavity. The significant finding of lower Apgar scores in the study group could be attributed to the effect of general anesthesia, prolonged incision delivery time of the baby due to adhesions, or large fibroids posing a difficult and challenging delivery.
The retrospective nature of the study could be a limiting factor in our study. In addition, the study was conducted at one tertiary center, which explains the limited number of cases.
Conclusion
Women with large uterine fibroids measuring > 5 cm in diameter are more likely to develop obstetric complications, including PPH and a higher cesarean risk. Therefore, women with large fibroids should be closely monitored during pregnancy and counseled in detail regarding unfavorable obstetric outcomes. Also, specific recommendations can be made from these results regarding the value of myomectomy before conception in such women.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Radhika BH, Naik K, Shreelatha S, Vana H. Case series: pregnancy outcome in patients with uterine fibroids. J Clin Diagn Res 2015 Oct;9(10):QR01-QR04.
- 2. Sampat K, Alleemudder DI. Fibroid in pregnancy: management and outcome. TOG 2018;20(3):187-195 .
- 3. Lee HJ, Norwitz ER, Shaw J. Contemporary management of fibroids in pregnancy. Rev Obstet Gynecol 2010;3(1):20-27.
- 4. Ciavattini A, Delli Carpini G, Clemente N, Moriconi L, Gentili C, Di Giuseppe J. Growth trend of small uterine fibroids and human chorionic gonadotropin serum levels in early pregnancy: an observational study. Fertil Steril 2016 May;105(5):1255-1260.
- 5. Mitra D, Bhatti S, Iskaros JP. 86 outcome of pregnancies with uterine leiomyoma: a population based retrospective study. Arch Dis Child Fetal Neonatal Ed 2013;98(Suppl 1):A104-A105.
- 6. Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol 2008 Apr;198(4):357-366.
- 7. Machado LS, Gowri V, Al-Riyami N, Al-Kharusi L. Caesarean myomectomy: feasibility and safety. Sultan Qaboos Univ Med J 2012 May;12(2):190-196.
- 8. Laughlin SK, Baird DD, Savitz DA, Herring AH, Hartmann KE. Prevalence of uterine leiomyomas in the first trimester of pregnancy: an ultrasound-screening study. Obstet Gynecol 2009 Mar;113(3):630-635.
- 9. Somigliana E, Vercellini P, Daguati R, Pasin R, De Giorgi O, Crosignani PG. Fibroids and female reproduction: a critical analysis of the evidence. Hum Reprod Update 2007 Sep-Oct;13(5):465-476.
- 10. Kwon DH, Song JE, Yoon KR, Lee KY. The safety of cesarean myomectomy in women with large myomas. Obstet Gynecol Sci 2014 Sep;57(5):367-372.
- 11. Bulun SE. Uterine fibroids. N Engl J Med 2013 Oct;369(14):1344-1355.
- 12. Mollica G, Pittini L, Minganti E, Perri G, Pansini F. Elective uterine myomectomy in pregnant women. Clin Exp Obstet Gynecol 1996;23(3):168-172.
- 13. Szamatowicz J, Laudanski T, Bulkszas B, Akerlund M. Fibromyomas and uterine contractions. Acta Obstet Gynecol Scand 1997 Nov;76(10):973-976.
- 14. Romero R, Chervenak FA, DeVore G, Tortora M, Hobbins JC. Fetal head deformation and congenital torticollis associated with a uterine tumor. Am J Obstet Gynecol 1981 Dec;141(7):839-840.
- 15. Shavell VI, Thakur M, Sawant A, Kruger ML, Jones TB, Singh M, et al. Adverse obstetric outcomes associated with sonographically identified large uterine fibroids. Fertil Steril 2012 Jan;97(1):107-110.
- 16. Deveer M, Deveer R, Engin-Ustun Y, Sarikaya E, Akbaba E, Senturk B, et al. Comparison of pregnancy outcomes in different localizations of uterine fibroids. Clin Exp Obstet Gynecol 2012;39(4):516-518.
- 17. Mu YL, Wang S, Hao J, Shi M, Yelian FD, Wang XT. Successful pregnancies with uterine leiomyomas and myomectomy at the time of caesarean section. Postgrad Med J 2011 Sep;87(1031):601-604.
- 18. Rothmund R, Taran FA, Boeer B, Wallwiener M, Abele H, Campo R, et al. Surgical and conservative management of symptomatic leiomyomas during pregnancy: a retrospective pilot study. Geburtshilfe Frauenheilkd 2013 Apr;73(4):330-334.
- 19. Hassiakos D, Christopoulos P, Vitoratos N, Xarchoulakou E, Vaggos G, Papadias K. Myomectomy during cesarean section: a safe procedure? Ann N Y Acad Sci 2006 Dec;1092:408-413.
- 20. Song D, Zhang W, Chames MC, Guo J. Myomectomy during cesarean delivery. Int J Gynaecol Obstet 2013 Jun;121(3):208-213.