A two-year-old girl had an alleged trivial fall from a chair. There was no loss of consciousness or ear bleeding during the incident. After the incident, her parents noticed she was not responding to sound. She had normal hearing and speech development before the trauma. There was no history of otalgia or otorrhea. Additionally, the parents noticed that child had an unsteady gait upon walking, which lasted for
one week.
Upon examination, the patient looked comfortable. There was no feature of dysmorphism. Otoscopic examination appeared normal external auditory canals and intact tympanic membranes bilaterally. Brainstem evoked response test showed absent of wave V at 99 dBnHL bilaterally, suggestive of profound hearing loss at high frequencies. Similarly, there was no response at 117 dB across all frequencies in the auditory steady-state response test, which suggested bilateral profound sensorineural hearing loss (SNHL). Repeated hearing assessment four months post-trauma showed significant improvement in her hearing to moderate SNHL. Her hearing level improved to mild SNHL at eight months post-trauma. High-resolution computed tomography (HRCT) of the temporal bone was performed as shown in Figure 1.
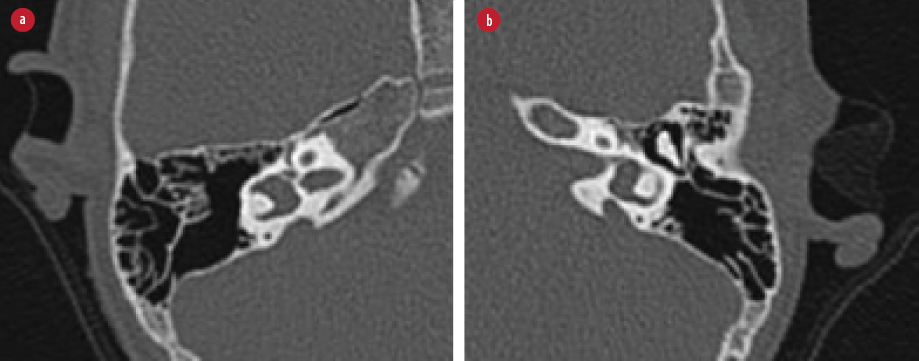
Figure 1: High-resolution computed tomography of (a) right and (b) left temporal bone.
Question
What is the possible diagnosis?
a) Hypoplastic semicircular canals.
b) Large vestibular aqueduct syndrome (LVAS).
c) Enlarged internal acoustic meatus.
d) Congenital absence of cochlear duct.
Answer
b) LVAS.
Discussion
LVAS is a congenital malformation of the inner ear. The prevalence of LVAS was estimated to be 13% among pediatric patients with SNHL.1 It is characterized by bony enlargement of the vestibular aqueduct causing abnormal dilatation of the endolymphatic sac. LVAS was also related to other inner ear abnormalities or syndromes such as Pendred and Waardenburg syndromes.2 There is a predilection in females compared to males.1 Most patients do not experience hearing loss at birth. The nature of hearing loss varies and is either progressive or fluctuating, as depicted by interval audiograms;3 28% suffered from fluctuating hearing loss while 51% had stable hearing loss.1 The hearing loss can also be precipitated by trivial head trauma, as experienced in this case. Serial audiological assessments are important in determining the progression of hearing loss. On the other hand, vestibular symptoms were found in 48% of pediatric patients with LVAS.3
Clinical suspicion is raised when the child experiences sudden hearing loss following a minor head injury. It is postulated that the auditory and vestibular symptoms are contributed by the excessive accumulation of the endolymph within the enlarged endolymphatic sac, causing increased endolymph osmotic pressure. Subsequently, there is reflux of the fluid into the vestibule. It causes alteration in biochemical activity and destruction of the neuroepithelium.2,4 As a result, patients will experience hearing loss and vertigo. LVAS is known to have a genetic predisposition, with the SLC26A4 gene associated with this condition.4

Figure 2: The red arrows point to the (a) right and (b) left enlarged vestibular aqueducts.
The diagnosis of LVAS is made based on radiological findings. Therefore, HRCT of the temporal bone and magnetic resonance imaging (MRI) of the inner ear are important to evaluate the abnormalities. HRCT of the temporal bone provides details on the bony enlargement of the vestibular aqueduct, while MRI of the inner ear demonstrates the distension of the endolymphatic sac. HRCT alone was sufficient to diagnose LVAS because the findings on both imaging produced similar sensitivity in detecting this anomaly.5 In normal findings, the vestibular aqueduct is hardly appreciated in the HRCT. The vestibular aqueduct is considered enlarged when the diameter at the midpoint is > 1.5 mm.6 In this case, the HRCT of the temporal bone showed bilateral enlargement of the vestibular aqueducts as outlined by the arrows [Figure 2].
The treatment for LVAS depends on the severity of the hearing impairment. The mainstay of the treatment is to avoid any precipitating factors, such as preventing head trauma.2 Hearing rehabilitation is indicated in patients with evidence of hearing impairment. Cochlear implantation should be considered in patients who do not benefit from hearing aids. Although cochlear implant is thought to be challenging in LVAS, the incidence of perilymph gusher in this condition is relatively small compared to cochlear aqueduct anomaly.7 Study had shown that the auditory outcome for patients with LVAS following cochlear implantation was comparable to those without any inner ear abnormality.8
Disclosure
The authors declared no conflicts of interest. Written consent had been taken from patient’s parents to publish this case report.
references
- 1. Madden C, Halsted M, Benton C, Greinwald J, Choo D. Enlarged vestibular aqueduct syndrome in the pediatric population. Otol Neurotol 2003 Jul;24(4):625-632.
- 2. Gleeson M. Pathology of the vestibular system. In: Bagger-Sjoback D, Rask-Andersen H, editors. Scott-Brown’s otorhinolaryngology, head and neck surgery. 7th ed. UK. Hodder Arnold; 2008. p. 3683-3685.
- 3. Grimmer JF, Hedlund G. Vestibular symptoms in children with enlarged vestibular aqueduct anomaly. Int J Pediatr Otorhinolaryngol 2007 Feb;71(2):275-282.
- 4. Griffith AJ, Wangemann P. Hearing loss associated with enlargement of the vestibular aqueduct: mechanistic insights from clinical phenotypes, genotypes, and mouse models. Hear Res 2011 Nov;281(1-2):11-17.
- 5. Connor SE, Dudau C, Pai I, Gaganasiou M. Is CT or MRI the optimal imaging investigation for the diagnosis of large vestibular aqueduct syndrome and large endolymphatic sac anomaly? Eur Arch Otorhinolaryngol 2019 Mar;276(3):693-702.
- 6. Valvassori GE, Clemis JD. The large vestibular aqueduct. Laryngoscope 1978;88(5):723-728.
- 7. Bianchin G, Polizzi V, Formigoni P, Russo C, Tribi L. Cerebrospinal fluid leak in cochlear implantation: Enlarged cochlear versus enlarged vestibular aqueduct. Int J Otolaryngol 2016;2016:6591684.
- 8. Song MH, Yoo JE, Choi JY, Choi HS. Auditory outcome of cochlear implantation n adolescent and adult patients with enlarged vestibular aqueduct and biallelic SLC26A4 mutations. Korean J Otorhinolaryngol-Head Neck Surg 2017;60(12):605-613.