Blunt chest trauma is associated with high mortality. Injury to coronary vessels can include dissection, contusion, and intramural hematoma. Coronary angiography can identify the location but may be able to identify the mechanism of injury. Multi-detector computed tomography (MDCT) can locate and elucidate the nature of coronary artery injury on admission and during follow-up. Utilizing multimodal imaging, including cardiac CT and cardiac magnetic resonance imaging (MRI), can help understand the nature of coronary artery injury and guide management.
Case report
A 58-year-old female with a history of morbid obesity, hypertension, hyperlipidemia, bipolar disorder, depression, and hypothyroidism presented to our emergency department (ED) with two days of chest pain. Her pain started after sustaining a left lateral chest wall contusion in a motor vehicle collision. Upon arrival to the ED, an initial electrocardiogram (ECG) was unremarkable [Figure 1], with positive troponin that peaked at 37 ng/dL. Upon presentation, she was tachycardiac and tachypneic with soft blood pressure. A CT angiography of the chest did not reveal any evidence of pulmonary embolism or aortic dissection. Subsequently, a bedside echocardiogram showed a left ventricular ejection fraction of 55% with basal and mid inferolateral hypokinesis. The patient was admitted to the cardiac floor as a case of non-ST segment elevation myocardial infarction. Given the increasing severity of chest pain, the decision was made to proceed with an urgent coronary angiography that showed abrupt high-grade narrowing of the distal circumflex (LCx) and first obtuse marginal branch (OM-1) with TIMI 3 flow.
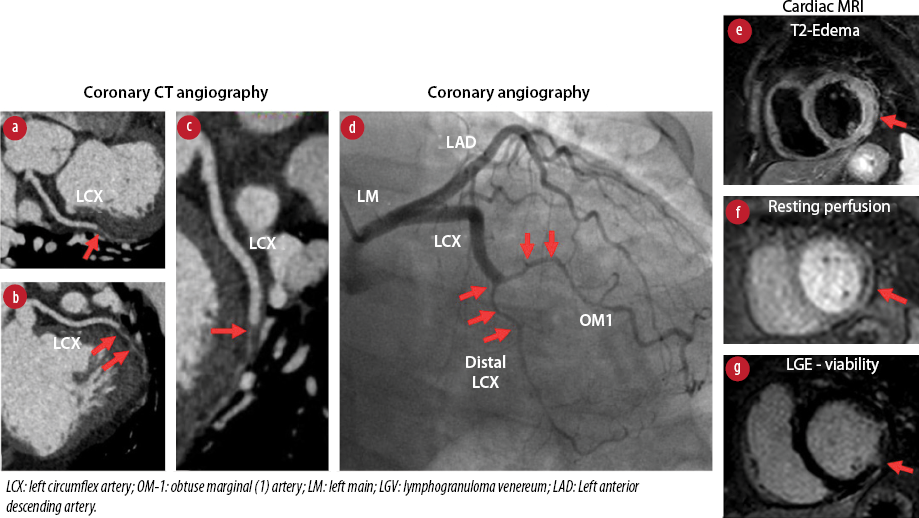
Figure 1: ECG at presentation to the emergency department.
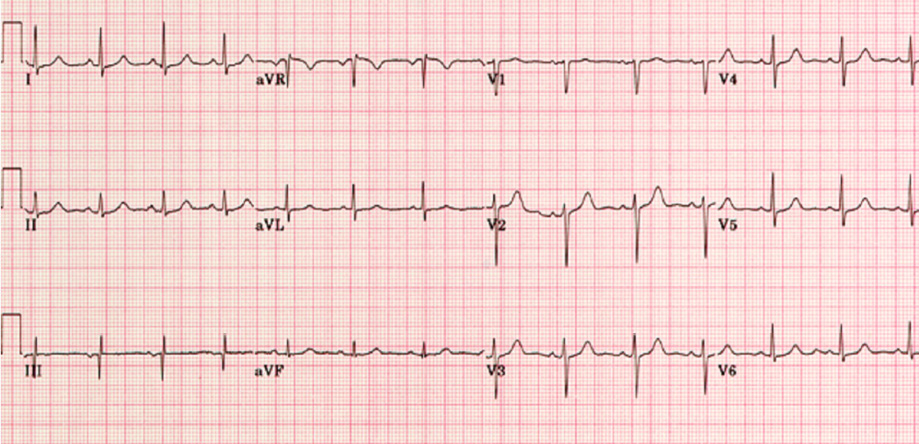
Figure 2: Multimodality imaging of intramural hematoma of distal LCX and OM-1.
To further evaluate the pathology of the LCx lesion, a cardiac CT angiography showed a faint flow of contrast with intramural hematoma along the distal LCx and OM-1. Cardiac MRI showed hypokinesis, edema, resting perfusion defects, and transmural late gadolinium enhancement in the basal-to-mid anterolateral and basal-to-mid inferolateral segments, suggestive of acute/subacute myocardial infarction in the LCx/OM-1 territory [Figure 2].
We suspected that this traumatic injury was related to the blunt chest trauma. However, given the worsening symptoms and increasing chest pain severity, we preceded with cardiac CT and MRI. An intramural hematoma was identified in the area of narrowing along the distal LCx and OM-1 branch on cardiac CT. Cardiac MRI confirmed wall motion abnormalities in this coronary distribution. We treated this patient in the same manner as one presenting with spontaneous coronary artery dissection and did not pursue percutaneous coronary intervention. The patient was discharged after five days of hospitalization on dual antiplatelet therapy. She was followed up at one and three months, and continued to do well with no new symptoms. A follow-up cardiac CT showed mild disease in the mid LCx artery consistent with ‘healed’ prior dissection.
Discussion
Blunt chest trauma has been associated with rib fractures, pneumothorax, pulmonary contusion, and cardiac and aortic injury.1 Mortality rates have been reported in the literature up to 5.5%.2 Cardiac injuries have been reported in 10–15% of chest trauma cases.3 A multitude of unpredictable mechanisms include direct trauma to the organs of the thoracic cavity, deceleration injury, and acute increases in aortic pressure.4 Frequent cardiac injuries include contusion with arrhythmias, effusion, and even tamponade in the setting of direct, blunt trauma.
Five kinds of coronary lesions are described in the literature. Intimal tear leading to dissection, thrombosis secondary to artery compression, external compression or sub intimal edema causing a stenotic lesion, coronary rupture, and coronary fistula.5,6 Coronary occlusion can result from vasospasm, intimal injury with thrombosis, or compression by an epicardial hematoma or intramural hematoma. The left anterior descending artery has been described as the most commonly involved.7 However, the mechanism of injury and vector of forces can influence the injury of the other epicardial coronary vessels, as in our case.
The diagnosis of potential coronary injury post-trauma requires the clinician to have a high degree of suspicion as the typical chest pain scenario can be confounded by soft tissue injury-related pain. One would have to employ several tools, including ECG, cardiac enzymes, echocardiogram, and coronary CT imaging or angiography. It is important to consider acute coronary syndrome in the differential diagnosis of chest pain following blunt chest trauma.
The differential diagnosis of chest pain with elevated troponins in the setting of a recent blunt chest trauma includes acute coronary syndrome due to coronary artery dissection or ruptured plaque, aortic dissection, coronary spasms, coronary embolism, and myocardial contusion.
Despite being less common compared to left anterior descending artery or right coronary artery, LCx is prone to dissection, especially in left lateral chest trauma. There should be a high degree of suspicion in those presenting with chest pain, troponin release +/- ischemic ECG changes.
Conclusion
Blunt chest trauma is associated with high mortality. Injury to coronary vessels can include dissection, contusion, and intramural hematoma. Coronary angiography is the gold standard diagnostic tool to diagnose this pathology. However, cardiac CT adds valuable information to the nature and mechanism of coronary injury. Coronary artery dissection is generally managed medically with an overall good prognosis.
Disclosure
The authors declared no conflicts of interest. A consent was obtained from the patient.
references
- 1. James MM, Verhofste M, Franklin C, Beilman G, Goldman C. Dissection of the left main coronary artery after blunt thoracic trauma: Case report and literature review. World J Emerg Surg 2010 Jul;5(1):21.
- 2. Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand J Trauma Resusc Emerg Med 2017 Apr;25(1):42.
- 3. Yousef R, Carr JA. Blunt cardiac trauma: a review of the current knowledge and management. Ann Thorac Surg 2014 Sep;98(3):1134-1140.
- 4. Chirtwood WR, Austin EH. Cardiac trauma: penetrating and blunt. In: Moylan JA, editor. Trauma surgery. Philadelphia, PA: Lipincott; 1988. p. 123-181.
- 5. Kahn JK, Buda AJ. Long-term follow-up of coronary artery occlusion secondary to blunt chest trauma. Am Heart J 1987 Jan;113(1):207-210.
- 6. Voyce SJ, Ball SP, Gore JM, Shine WJ, Weiner BH. Angiographically documented thrombotic coronary artery occlusion secondary to mild nonpenetrating thoracic trauma. Cathet Cardiovasc Diagn 1991 Nov;24(3):179-181.
- 7. Lobay KW, MacGougan CK. Traumatic coronary artery dissection: a case report and literature review. J Emerg Med 2012 Oct;43(4):e239-e243.