A 31-year-old man presented with left facial discomfort over the maxillary sinus area lasting for one year. It was associated with hyposmia. He had a history of intermittent attacks of facial pains that responded temporarily to antibiotics. He had no history of allergy. On examination, tenderness was elicited over the left maxillary sinus. Intraorally, postnasal discharge was noted on the posterior pharyngeal wall. Nasal endoscopy revealed a greenish purulent discharge on the floor of the left nasal cavity originating from the left middle meatus. A radiograph was requested [Figure 1]. The provisional diagnosis was left chronic maxillary sinusitis. A computed tomography scan (CT) of paranasal sinuses was requested [Figure 2].

Figure 1: Water’s view for nasal sinuses of a 31-year-old man presenting with left facial discomfort.
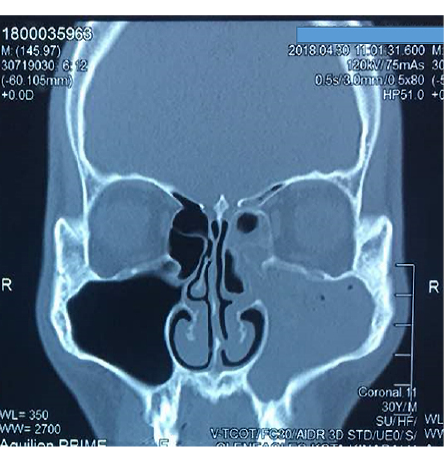
Figure 2: CT scan of the patient.
Question
1. What is the abnormality shown in the radiological pictures that led to left maxillary sinusitis?
a. Nasal polyposis.
b. Dental cause.
c. Deviated septum.
d. Antrochoanal polyp.
e. Pneumatized middle turbinate.
Answer
e. Pneumatized middle turbinate.
Waters’ view skull radiograph [Figure 1] showed the near-complete opacity of the left maxillary sinus with no sclerotic changes in the maxillary surrounding bone and minimal bowing of the nasal septum towards the right. The frontal sinuses are preserved bilaterally.
Besides, the CT scan demonstrated a generalized mucosal thickening of nasal turbinates in both sides together with left ethmoidal air cells
[Figure 2]. The left maxillary ostium was obliterated and obstructed by the pneumatized left middle turbinate
(concha bullosa).
Discussion
This patient was diagnosed with left chronic
maxillary sinusitis because the condition lasted more than 90 days.1 Unilateral sinusitis can develop secondary to ipsilateral dental problems (in 5% to 10% of chronic cases), fungal infection, or nasal foreign body.1,2 Nasal malignancy or inverted papilloma should be ruled out in the presence of progressive nasal blockage and epistaxis.3 Obstruction to the sinus drainage is also one of the important predisposing factors.
A nasal examination using light and a Thudichum speculum was performed to look for the site and the nasal discharge: its amount, color, odor, and character. It was followed by throat examination to look for postnasal drip from the nasal cavity.
Secondly, a diagnostic nasal endoscopy was performed to explore the entire nasal cavity and postnasal space thoroughly. Imaging is crucial to determine the cause and subsequently to plan the treatment. CT scan helps to study the structural bony abnormalities. In this case, pneumatized middle turbinate (concha bullosa) has led to mechanical obstruction of the maxillary sinus’s natural opening and hindered its ventilation and drainage,1 eventually, causing left chronic maxillary sinusitis. Concha bullosa is present in one-third of healthy individuals.4
In this case of acute on chronic sinusitis, we instituted medical therapy first in the form of broad-spectrum antibiotics (co-amoxiclav) for seven days,1 systemic decongestant, and analgesics. Locally, the patient used alkaline nasal douching to clear the nasal discharge before applying the local nasal decongestant spray.1 The treatment aimed to open the maxillary ostia and to restore the sinus ventilation. However, the clinical condition did not improve, and surgical intervention was determined. Functional endoscopic sinus surgery was undertaken to remove the concha bullosa and widen the maxillary ostium. After the surgery, the patient was clinically asymptomatic, and endoscopically the nose and pharynx were free of purulent discharge.
Acknowledgements
We would like to thank the patient for his consent.
references
- 1. Croton L. GP management of sinusitis.2012. GP online. 2019 [cited 2019 June 30]. Available from: https://www.gponline.com/gp-management-sinusitis/article/1117255.
- 2. Paz Silva M, Pinto JM, Corey JP, Mhoon EE, Baroody FM, Naclerio RM. Diagnostic algorithm for unilateral sinus disease: a 15-year retrospective review. Int Forum Allergy Rhinol 2015 Jul;5(7):590-596.
- 3. Kountakis ES, Onerci M, editors. Rhinological and sleep apnea surgical techniques. Springer Publications; 2007.
- 4. Simmen D, Jones N. Manual of endoscopic sinus surgery: and its extended applications. Thieme publications; 2011.