Chronic diseases have become a primary concern for healthcare systems worldwide.1 The World Health Organization states that 24 million people per year (about 50% of all deaths worldwide) die due to chronic conditions.2 In 2006 alone, chronic diseases were responsible for 35 million deaths worldwide.3 Projections are that chronic conditions will account for 60% and 70% of the global disease burden by 2020 and 2035, respectively.4 Chronically, ill patients are frequent and long-term users of health services. The evidence suggests that about two-thirds of patient encounters with health professionals are for the management of chronic conditions.5
One of the major chronic diseases causing worldwide public health challenge is diabetes mellitus (DM).6,7 It is the fifth leading cause of death in high-income countries and is rapidly becoming epidemic in many low and middle-income countries.8 Globally, the number of people who have diabetes in 2014 was estimated at 422 million, and this number is expected to rise to 592 million by 2035, while 175 million people remain undiagnosed.8 Diabetes care is expensive,9 and the condition can lead to serious complications such as kidney failure, myocardial infarction, stroke, blindness, and limb amputation.10 It imposes a huge economic burden on national healthcare systems. Depending on the country, it could take up between 5–15% of total health expenditure.11
Three main types of diabetes are known: 1) type 1 diabetes (caused by the body’s failure to produce insulin), 2) type 2 diabetes (resulting from insulin resistance), and 3) gestational diabetes (which occurs in pregnant women without a previous diagnosis of diabetes).12,13 Of the three, type 2 diabetes is the most common, constituting approximately 95% of all DM cases.8,11 The prevalence varies with age, gender, ethnic background, and genetic susceptibility. It is associated with environmental risk factors such as lack of physical activity, nutritional status, and obesity.12
Available evidence indicates that early diagnosis and effective management increases the chances of preventing harmful and costly complications associated with diabetes.14 Evidence has also been established regarding the benefits associated with glycemic control in reducing the risk for and delaying the progression of diabetes complications.8 Achieving effective glycemic control requires a lifelong adherence to complex lifestyle management, involving regular blood glucose monitoring, self-adjustment of medications, and a physically active lifestyle. Self-management education (SME), which is based on patient empowerment,15 is recognized globally as a tool that enables patients to achieve optimal glucose control by increasing knowledge and awareness and learning behavioral strategies to manage diabetes.6,16
Diabetes self-management education (DSME) is defined as the “ongoing process of facilitating the knowledge, skill, and ability necessary for self-care”.17 The process, guided by evidence-based research, incorporates the needs, goals, and life experiences of people with diabetes.8 The overall objectives of DSME are to support self-care behaviors, problem-solving, informed decision-making, and active collaboration with healthcare teams and improve clinical outcomes, health status, and quality of life.17 The intervention involves various educational programs, ranging from brief instructions by lay leaders, physicians, dieticians, or nurses to more formal and comprehensive programs.14 In the 1960s and 1970s, DSME interventions were individually oriented and mostly delivered in hospital settings by either nurses or dietitians.8 From 1980 onwards, more specific programs have been developed for diabetes patients and their families.18 Health professionals with different backgrounds educate patients in their domain of expertise. In addition to individual education, more cost-effective interventions such as group-based education,19 information technology-based education,20 and self-help and support group programs18 have been developed.
The efficacy of DSME is supported by a large number of studies, including randomized controlled trials. DSME is thought to improve glycemic control by 1% in people with type 2 diabetes.21 A meta-analysis of 18 randomized studies published between 1966 and 1999 found a significant decrease in mean glycated hemoglobin (HbA1c) by 0.43%.22 Another review of 11 studies from 1988 to 2002 also reported a significant HbA1c reduction of 1.4% at 4–6 months.23 More recently, a meta-review of systematic reviews found that 34 out of the 35 included reviews reported a statistically significant improvement in HbA1c following a DSME intervention.24
Given this demonstrated efficacy of the existing interventions on glycemic control,25–30 the current policy challenge is not to find new efficacious treatments but to implement the proven programs more cost-effectively.8 Over the last decades, many reports on factors influencing the efficacy and cost-effectiveness of DSEM programs have been published. Some target intervention attributes such as mode of delivery (group sessions vs. individual teaching),31,32 delivery setting (community gathering places vs. medical settings),33 timing and program content,34,35 and trainer’s background (medical, allied health, or peer).34,36,37 Others focus on patients’ personal characteristics, such as health status,38,39 disease duration,40 age, educational level, and partner’s influence,41,42 economic status,43 language and culture,44 and gender difference.40,45,46
While many of these factors affecting the effectiveness of DSEM programs have been studied extensively, the impact of program length on the clinical outcomes of type 2 diabetics has received little research attention. Self-management interventions vary substantially in terms of duration.47 For instance, the majority of the programs modeled after the Stanford Model usually involve six weeks of education. Others with different theoretical underpinnings have varied time lengths, ranging from one day to five years and above. It is thus vital to ascertain the impact of program duration on the outcomes of these DSME interventions. Such information will inform policy decisions on optimizing the design and implementation of more cost-effective self-management programs.
Recently, in a review to assess the effect of DSME interventions on glycemic control, the authors concluded that program duration (i.e., total hours of engagement) could affect the likelihood of achieving significant improvements in clinical outcomes.48 However, because they included trials enrolling participants with type 1 and type 2 DM patients in their analysis, their conclusion appears more general than being specific to patients with type 2 DM.
Therefore, the present study is a systematic review of the existing, published, randomized controlled trials to assess the impact of DSME program length on HbA1c in adults with type 2 DM. We chose HbA1c as the clinical endpoint of this study because glycemic control has been demonstrated to strongly predict both the microvascular (diabetic, nephropathy, neuropathy, and retinopathy) and the macrovascular (coronary artery disease, peripheral arterial disease, etc.) complications associated with diabetes.49,50 For instance, the UK Prospective Diabetes Study has demonstrated that a 1% reduction in HbA1c is associated with a 21% decrease in diabetes-related endpoints, an 18% reduction in combined fatal and non-fatal myocardial infarction, a 12% decrease in stroke, a 37% decrease in microvascular endpoints, a 25% reduction in diabetes-related deaths, and a 7% decrease in all-cause mortality.51 Moreover, HbA1c has been considered the primary outcome measure in most diabetes SME intervention studies.21–24 This study contributes to the current knowledge of the factors affecting the efficacy and cost-effectiveness of DSME interventions.
Methods
We designed and conducted a systematic literature search according to the Population, Intervention, Comparison, Outcome, and Study design (PICOS) framing. The population of interest was adults with type 2 DM. The intervention considered was DSME program. The comparison groups were patients receiving ‘usual care’ or ‘standard care’. The outcome of interest was glycemic control. Study designs considered were randomized or clinical controlled trials. Our research question was: What is the impact of DSME program length on glycemic control in adults with type 2 DM?
We identified relevant literature through electronic searches. A librarian from the School of Medical Sciences, Kwame Nkrumah University of Science and Technology, was consulted in developing our search strategy, which included identifying keywords and medical subject headings (i.e., MeSH terms). Electronic searches were made on Web of Science, PubMed, Scopus, MEDLINE, EMBASE, PsychINFO, and the Cochrane Central Register of Controlled Trials. We restricted the search to only English language medical literature published between January 2000 and April 2019. The medical subject headings searched included: ‘SME program’ combined with: ‘type 2 diabetes’, ‘glycemic control’, and ‘controlled trial’. We identified additional relevant articles by manually searching the bibliographies of the retrieved papers.
After removing duplicate publications, 1081 records were screened for eligibility. We carefully read the titles and abstracts of these 1081 papers focusing on two main criteria: 1) Does the paper discuss diabetic patient/individual? 2) Does it focus on a SME program? A paper had to meet both criteria to be considered in the next stage of our review. Following this procedure, we excluded 804 articles.
The remaining 277 articles were retrieved and read by three reviewers. A study had to fulfill six inclusion criteria to be eligible for inclusion in the final analysis:
- Must not be a review article or a report.
- Should evaluate the effectiveness of the DSME program on HbA1c.
- Should focus on type 2 diabetes patients.
- Should indicate program length or duration.
- Must be a randomized controlled trial, comparing an intervention group to a control group.
- Should not compare two or more educational programs (e.g., group vs. individual education).
Any differences in opinion regarding papers’ eligibility were discussed and resolved by the reviewers.
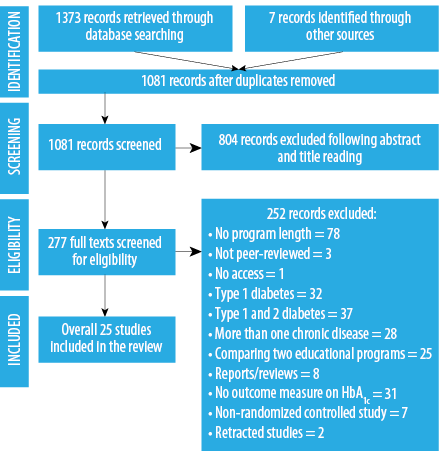
Figure 1: Literature search flow diagram.
A further 252 articles were excluded after reading the full-text. The most common reason for exclusion was a lack of reporting on program length/duration (n = 78). Other common exclusions included: not assessing program effect on HbA1c (n = 31), focusing on either type 1 (n = 32) or both type 1 and type 2 (n = 37) diabetes patients, focusing on more than one chronic disease (n = 28), and comparing the effectiveness of two educational programs
(n = 25). The flow diagram in Figure 1 depicts the stages of study identification and reasons for paper exclusion. Twenty-five articles were included in the final analysis.
Internal validity of the individual studies was assessed using the Cochrane Collaboration Criteria for four types of bias: selection, performance, attrition, and detection biases52 [Table 1]. Studies were scored from 0 to 4, with a score of 4 indicating the absence of the four potential sources of bias and a score of 0 signifying the possibility of the presence of these biases.
Table 1: Assessment of internal validity based on Cochrane Collaboration methodology.
|
Selection bias |
Systematic differences between baseline characteristics of the study and the control groups. |
|
|
|
Performance bias |
Systematic differences between study and control groups in the care that is provided, apart from the intervention being evaluated. |
|
|
|
Attrition bias |
Systematic difference between study groups in withdrawals from a study. |
|
|
Two members of the research team did data extraction from the selected publications. A subsample of the articles was also evaluated by a second assessor (a third member of the research team), yielding an assessor agreement of 95%. The assessors then discussed the differences and reached a consensus. A fourth member verified all the extracted information against each of the selected papers to ensure data consistency and accuracy. The information recorded about each study included: authors and year of publication, study sample, study site (country), study aim/objective, length of the program, SME provider (dietitian, nurse, peer educator, physician, etc.), description of the intervention, study outcome (effect on HbA1c), and conclusions drawn from the findings.
We categorized the studies into three program lengths (short, medium, and long-term) and compared interventions’ effects on HbA1c across these categories. For this study, we defined short-term programs as interventions having a duration of three months or less (i.e., ≤ 3 months); medium-term as between three and 12 months duration (> 3 to < 12 months); and long-term as those lasting 12 months or more (≥ 12 months).
We judged the effectiveness of each program based on the level of significance of the HbA1c mean difference between the intervention and the control groups. Although a section of the literature considers an intervention effective once the experimental subjects achieve a greater reduction in HbA1c levels than those in the control group, we believe that a successful intervention should, in addition to this, have a statistically significant difference in HbA1c change between the two groups. Thus, only programs that reported a significant HbA1c mean difference between the intervention and the control groups were considered effective in the current study.
Results
Validity scores of the 25 studies were moderate, with a mean of 2.1±0.8 (range = 0.0–4.0). Scores for each study on the Cochrane Collaboration Criteria for the four types of bias are shown in the Appendix. Generally, studies (96.0%) met the criteria for a possible absence of performance bias by demonstrating no possibility of contamination between the study and the control groups and no treatment differences between the groups, apart from the DSME intervention. A moderate number of studies (52.0%) met the criteria for an absence of selection bias. However, the marked difference in characteristics between the intervention and the control groups at baseline was a major concern for some of the studies (48.0%). The majority of the studies (56.0%) did not meet the attrition bias absence criteria. These studies either did not meet a retention rate of ≥ 80%, as recommended by the Cochrane Criteria52 or failed to compare the baseline characteristics of those who completed the study and those who dropped out. Almost all of the studies (96.0%) did not meet the criteria for a possible absence of detection bias by failing to report on blinding of those who carried out the outcome assessment and statistical analysis.
A detailed description of the selected studies is presented in Table 2. A total of 28 216 type 2 diabetes patients, made up of 2746 intervention subjects and 25 470 controls, were included in the 25 studies. The mean age of the participants reported was approximately 58.0 years, with the mean percentage of female and male patients being 54.2% to 45.8%, respectively. The majority of the studies were conducted in the USA (40.0%), followed by the UK (16.0%). The remaining studies were carried out in Brazil, the Netherlands, Iran, Japan, Greece, China, Norway, Australia, Taiwan, Iraq, and Kenya. The sample size ranged from 25 to 824. The studies were conducted between 2002 and 2018. Patients were recruited from several settings including primary or general medical practice, hospitals, community health centers, churches, outpatient diabetes clinics, university-affiliated clinics, and the general community (via advertisements and rosters of previous research studies). Most educational interventions were led by health professionals such as dietitians, nurses, clinical pharmacists, physicians, physiotherapists, and community health workers. Two publications did not provide information on SME providers, while two mentioned lay leaders as program instructors.
Table 2: Characteristics of the included studies.
|
Wolf et al,53 |
USA |
To assess the efficacy of a lifestyle intervention program that can be translated into clinical practice for obese patients with type 2 diabetes. |
144
(intervention = 73, control = 71) |
Registered dietitians |
|
Samuel-Hodge
et al,54 |
USA |
To develop and test a culturally appropriate, church-based intervention to improve diabetes self-management. |
201
(intervention = 117, control = 84) |
Peer educators, registered dietitian |
|
Scain et al,55 |
Brazil |
To evaluate the effectiveness of a structured, group education program in metabolic control in type 2 diabetics. |
104
(intervention = 52, control = 52) |
Trained nurse educators |
|
Goudswaard et al,56 |
The Netherlands |
To evaluate the short and long-term efficacy of a self-management education (SME) program in type 2 diabetes patients treated in primary care. |
58
(intervention = 28, control = 30) |
Diabetes nurses |
|
Shakibazadeh
et al,57 |
Iran |
To assess the effectiveness of a Persian Diabetes Self-Management Education program. |
280
(intervention = 140, control = 140) |
A nurse, dietitian, and counselor |
|
Deakin et al,58 |
UK |
To develop a patient-centered, group-based self-management program and assess its effectiveness on clinical and psychological outcomes. |
314
(intervention = 157, control = 157) |
Diabetes research dietitian |
|
Forjuoh et al,59 |
USA |
To assess the effectiveness of the Chronic Disease Self-Management Program on glycated hemoglobin and selected self-reported measures. |
196
(intervention = 101, control = 95) |
Peer educators |
|
Moriyama et al,60 |
Japan |
To develop and assess the efficacy of a 12-month-SME program for type 2 diabetics. |
65
(intervention = 42, control = 23) |
Nurse educator |
|
Merakou et al,61 |
Greece |
To assess the impact of a brief patient group education intervention in people with type 2 diabetes. |
193
(intervention = 138, control = 55) |
Trained health visitors |
|
Spencer et al,62 |
USA |
To assess the effectiveness of a culturally tailored, behavioral theory-based community health worker intervention for improving glycemic control. |
164
(intervention = 72, control = 92) |
Community health workers |
|
Sun et al,63 |
China |
To evaluate a structured and integrated intervention on diabetes management in type 2 diabetics. |
150
(intervention = 100, control = 50) |
Nutritionists |
|
Choe et al,64 |
USA |
To evaluate the effect of case management by a clinical pharmacist on glycemic control and preventive measures in type 2 diabetics. |
80
(intervention = 41, control = 39) |
Clinical Pharmacist |
|
Sevick et al,65 |
USA |
To evaluate behavioral intervention with technology-based self-monitoring on bio-physiologic outcomes. |
296
(intervention = 147, control = 149) |
Clinical diabetes educators |
|
Rosal et al,66 |
USA |
To test whether a theory-based, literacy, and culturally tailored self-management intervention improves glycemic control among low-income Latinos with type 2 diabetes. |
252
(intervention = 128, control = 124) |
A trained team of 2 leaders and an assistant |
|
Jacobs et al,67 |
USA |
To demonstrate that pharmacists working with physicians and other providers in an ambulatory care setting can improve glucose, blood pressure, and lipid control for patients with type 2 diabetes. |
396
(intervention = 195, control = 201) |
Pharmacists |
|
Johansen et al,68 |
Norway |
To compare a structured education program with standard care. |
120
(intervention = 60, control = 60) |
Nurse, physician, nutritionist, physiotherapist |
|
Rosal et al,69 |
USA |
To determine the feasibility of conducting a clinical trial of an innovative self-management intervention to improve metabolic control and to obtain preliminary data on possible intervention effects. |
25
(intervention = 15, control = 10) |
Nutritionist, nurse, and intervention assistant |
|
Brown et al,70 |
USA |
To determine the effects of a culturally competent diabetes self-management intervention. |
252
(intervention = 126, control = 126) |
Nurses, dietitian, and CHWs |
|
Davies et al,71 |
UK |
To evaluate the effectiveness of a structured group education program on biomedical, psychosocial, and lifestyle measures in people with newly diagnosed type 2 diabetes. |
824
(intervention = 437, control = 387) |
Trained health professionals |
|
Dyson et al,72 |
UK |
To develop a video-based lifestyle education program for people newly diagnosed with type 2 diabetes and evaluate changes in knowledge, biomedical indices, and quality of life. |
42
(intervention = 21, control = 21) |
|
|
William et al,73 |
Australia |
To evaluate an Australian Telephone-Linked Care diabetes program designed to improve diabetes management. |
117
(intervention = 57, control = 60) |
|
|
Huang et al,74 |
Taiwan |
To evaluate the effect of registered dietitian-led management of diabetes on glycemic control and macronutrient intake in type 2 diabetic patients in primary care. |
154
(intervention = 75, control = 79) |
Registered dietitians |
|
Abdulah et al,75 |
Iraq |
To examine the impact of a three-month self-management intervention on glycemic control. |
45
(intervention = 22, control = 23) |
|
|
Khunti et al,76 |
UK |
To determine whether the benefits of a structured program for newly diagnosed type 2 diabetes patients are sustainable. |
604
(intervention = 332, control = 272) |
Trained health professionals |
Table 3: Studies classified as short-term self-management education (SME) programs and their effects on glycated hemoglobin (HbA1c).
|
Scain et al,55 |
An eight-hour interactive education program, delivered in weekly sessions of two hours each, to a group of 8–10 subjects. |
1 |
HbA1c significantly differed between the IG and CG by 0.4% (p = 0.007) at four months, 0.5% (p = 0.009) at eight months, and 0.4%
(p = 0.04) at 12 months. |
The program improved glycemic control in patients with type 2 diabetes. |
|
Shakibazadeh et al,57 |
Eight 2.5-hour educational workshops offered over four weeks, followed by two booster sessions, each two weeks apart. |
2 |
HbA1c differed between the IG and the CG by 0.78%, 0.2 to 1.36 (p = 0.008). |
The program was effective in improving HbA1c levels. |
|
Deakin et al,58 |
Six weekly sessions, each lasting two hours, with an average of 16 participants plus four to eight carers. |
1.5 |
The IG had a greater reduction in HbA1c compared with the CG. Mean HbA1c difference between the two groups was 0.4%
(95% CI: 0.1–0.7, p <0.001) at four months and 0.7% (95% CI: 0.3–1.0, p < 0.001) at 14 months. |
Participation in the SEM program (X-PERT) led to improvements in glycemic control. |
|
Forjuoh
et al,59 |
A six-week classroom-based program teaching participants techniques to facilitate enhanced decision making, action planning, and effective communication. |
1.5 |
Reductions in HbA1c did not differ significantly beween the two groups (mean difference = 0.016%, p = 0.885). |
The SME program did not lower HbA1c levels any better than routine care. |
|
Merakou
et al,61 |
A structured group educational program using Conversation Maps; participants were divided into 19 groups (3–8 people per group), and each group attended a six-hour educational program, spread in three sessions, over three weeks. |
< 1 |
Significant difference in mean HbA1c was observed between the groups, 1.4% (95% CI: 1.1–1.7, p < 0.001). |
The intervention was more effective, compared with routine care, in diabetes self-management. |
|
Rosal et al,69 |
The intervention involved: one hour individual session, 10 group sessions (lasting 2.5 to 3 hours per session), and two 15-minute individual sessions. |
2.5 |
HbA1C significantly differed between the IG and the CG by 0.56% (p < 0.05) at three months and 0.73% (p < 0.01) at six months. |
The program resulted in significant improvements in HbA1c levels. |
|
Davies et al,71 |
A six-hour long, structured group education program delivered in either one day or two half-day equivalents and facilitated by two educators. |
< 1 |
The difference in HbA1c levels between the IG and the CG was not significant: 0.05% (95% CI: 0.10%–0.20%). |
The program resulted in no significant improvements in HbA1c levels. |
|
Abdulah
et al,75 |
A structured group education program for six hours delivered in the community by two trained professional educators. |
< 1 |
No significant difference in HbA1c between the IG and the CG: -0.02 (95% CI: -0.22–0.17). |
The program resulted in no improvement in HbA1c. |
CI: confidence interval; IG: intervention group; CG: control group.
The selected studies and their outcomes are grouped under the short, medium, and long-term classifications in Tables 3, 4, and 5, respectively. In all, 16 (64.0%) studies53,55-58,60–64,67–70,73,74 reported significant differences in HbA1C changes between the intervention and the control groups. Nine (36.0%) studies showed no significant effects. One study reported66 a significant difference in HbA1c change between the groups at the initial stage of the intervention (0.53%, p = 0.008), but this decreased and lost significance during the follow-up assessment (0.25%, p = 0.293). In the remaining eight studies,54,59,65,71,72,75–77 though significant reductions were recorded at the end of the interventions, between-group differences were not significant.
Nine studies were classified as short-term programs; five55,57,58,61,69 reported significant differences in changes in HbA1c between the intervention and the control groups, while four59,71,75,76 showed no significant differences [Table 3]. The overall difference in the mean change in HbA1c between the intervention and the control subjects for the nine studies was 0.4±0.3%
(range = 0.02–1.40). With the medium-term programs, eight studies were identified; four56,62,63,73 reported significant differences in between-group changes, while four65,66,72,77 showed no significant differences [Table 4]. The overall difference in the mean change in HbA1C between the groups was 0.4±0.2% (range = 0.1–0.8). The long-term interventions had eight studies; seven53,60,64,67,68,70,74 recorded significant differences in between-group changes, whereas one54 indicated no significant difference [Table 5]. The studies recorded an overall difference in between-group HbA1C mean change of 0.6±0.3% (range = 0.2–1.2).
Table 4: Studies classified as medium-term self-management education (SME) programs and their effects on glycated hemoglobin (HbA1c) .
|
Goudswaard et al,56 |
Six educational sessions, given at three to six-week intervals; sessions took between 15 and 45 minutes, resulting in a total contact time of 2.5 hours. |
6 |
HbA1C changed from 8.2 to 7.2 in the IG and from 8.8 to 8.4 in the CG. Mean HbA1c% in the study group fell by 0.7 more than in the CG (95% CI: 0.1–1.4; p = 0.025). |
The education was effective in improving glycemic control and delaying the need for insulin therapy for diabetes patients. |
|
Spencer et al,62 |
Three-activity intervention: 1) education classes, 2) two home visits per month to address participants’ specific self-management goals, and 3) one clinic visit with the participant and his/her care provider. |
6 |
HbA1C significantly reduced from 8.6 to 7.8 in the IG. Change in HbA1c level for the CG was not significant. The difference in the change in HbA1C level between the two groups was 0.80%. |
Intervention participants had significantly greater improvements in HbA1C levels compared with the control group. |
|
Sun et al,63 |
Education with frequent blood glucose monitoring, nutritional counseling, meal plans with diabetes-specific nutritional meal replacement, and weekly progress updates with study staff. |
6 |
HbA1c level significantly reduced by 0.85% in the IG, while the CG recorded no change. Mean HbA1c differed between the two groups
by 0.85%. |
The program resulted in significant improvements in HbA1C levels. |
|
Sevick et al,65 |
Group counseling sessions guided by Social Cognitive Theory were held weekly in the first two months, biweekly in the subsequent two months, and monthly in the last two months. |
6 |
HbA1c reduced in the IG by 0.5% (p < 0.001) at three months and 0.6% (p < 0.001) at six months, and the CG by 0.3% (p < 0.001) at three months and 0.2% (p < 0.05) at six months; but between-group differences (0.2% at three months and 0.4% at six months) were not significant. |
Though the intervention was effective in improving glycemic control, no significant between-group differences were observed. |
|
Rosal et al,66 |
An intensive phase of 12 weekly sessions and a follow-up phase of eight monthly sessions - the first session was an individual one-hour meeting; the remaining sessions were conducted in groups lasting for approximately 2.5 hours. |
11 |
A significant difference in HbA1C change between the groups was observed at four months (0.53%, p = 0.008), but this decreased and lost significance at 12 months (0.25%, p = 0.293). |
Immediate effects could not be sustained throughout the intervention. |
|
Dyson et al,72 |
Video intervention involving three lifestyle videos watched by patients in their own time. |
6 |
The difference in the HbA1c level between the two groups (0.1%) was not significant
(p = 0.843). |
The intervention could not improve HbA1c levels significantly over the six-month period. |
|
Williams
et al,73 |
A telephone-linked care diabetes system designed to improve diabetes management. Participants were trained to make weekly calls to the system over six months. Topics covered with the calls were: blood glucose monitoring, healthy eating, physical activity, and medication taking. |
6 |
HbA1c levels decreased by 0.8% in IG compared with 0.2% in the CG, resulting in a significant difference of 0.6% between the two groups. |
The intervention resulted in significant improvements in HbA1c levels. |
CI: confidence interval; IG: intervention group; CG: control group.
Table 5: Studies grouped as long-term self-management education (SME) programs and their effects on glycated hemoglobin (HbA1c).
|
Wolf et al,53 |
Individual and group education and support: participants attended six four-hour individual sessions and six one-hour small group sessions; support was provided via brief monthly phone contacts. |
12 |
HbA1C differed between the IG and the CG by 0.57% (p = 0.008) at four months; 0.35%, (p = 0.10) at eight months; and 0.20% (p = 0.45) at 12 months. |
The intervention improved glycemic control in patients with type 2 diabetes. |
|
Samuel-Hodge
et al,54 |
An eight-month intensive phase, consisting of one individual counseling visit, 12 group sessions, monthly phone contacts and three encouragement postcards; followed by a four-month reinforcement phase, including monthly phone contacts. |
12 |
At eight months, participants’ mean HbA1C was 7.4% for IG and 7.8% CG, with a difference of 0.4% (95% CI: 0.1–0.6, p = 0.009). At 12 months, the mean difference between groups (0.2%) was not statistically significant (p = 0.33). |
The program was effective at improving short, but not long-term metabolic control. |
|
Moriyama
et al,60 |
Monthly face-to-face individual interview sessions, lasting 30 minutes for each patient, and biweekly telephone calls throughout the intervention period. |
12 |
HbA1C changed from 7.44 to 6.85 in the IG, and from 7.28 to 7.25 in the CG. Mean HbA1C% in the IG fell by 0.56 more than in the CG. |
The program worked successfully in improving patients’ HbA1C levels. |
|
Choe et al,64 |
The case management involved the evaluation and modification of pharmacotherapy, SME, and reinforcement of diabetes complications screening processes through clinic visits and telephone follow-up. |
12 |
The IG achieved greater reduction in HbA1C levels than those in the CG (2.1% vs. 0.9%, p = 0.03). Mean HbA1C difference between the two groups was 1.2%. |
The intervention was successful at improving glycemic control and diabetes process-of-care measures. |
|
Jacobs et al,67 |
The intervention included: obtaining a comprehensive medication review, performing a physical assessment, ordering laboratory tests, reviewing, modifying, and monitoring patients’ medication therapy, facilitating self-monitoring of blood glucose, and providing reinforcement on dietary guidelines and exercise. |
12 |
Significant improvement in HbA1C occurred in the IG compared with the CG (a reduction of 1.8% in the IG compared with 0.8% in the CG). Mean HbA1C difference between the two groups was 1.0% (p = 0.003). |
The study demonstrated substantial improvements in HbA1C levels. |
|
Johansen
et al,68 |
The program involved: an educational course, one individual appointment with a nutritionist, free participation in a 10-week training program, and an encouragement to exercise at least three times a week. |
24 |
Improvement in HbA1C was greater among the IG patients than those in the CG (between-group change of 1.0% (p = 0.001). |
The study showed improved patient outcomes. |
|
Brown
et al,70 |
The intervention involved three months of weekly instructional sessions on nutrition, self-monitoring of blood glucose, exercise, other self-care topics, and six months of weekly support group sessions to promote behavior change. |
12 |
Mean HbA1C significantly differed between the IG and the CG by 0.76%. |
The intervention successfully lowered patients’ HbA1C levels. |
CI: confidence interval; IG: intervention group; CG: control group.
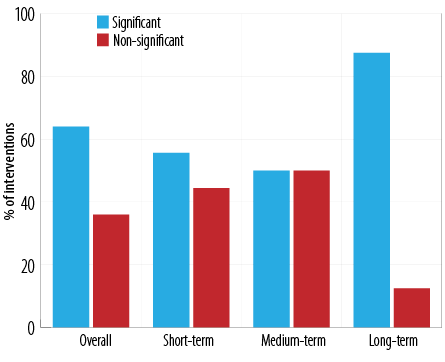
Figure 2: Effects of the diabetes self-management education interventions on glycated hemoglobin.
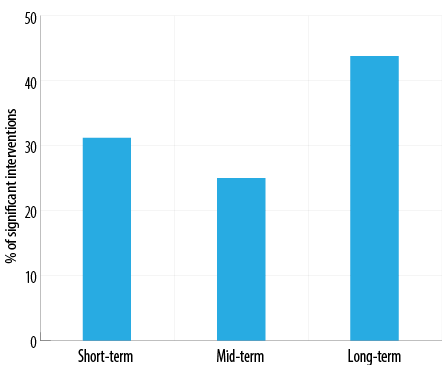
Figure 3: Interventions with significant glycated hemoglobin mean difference between cases and controls (n = 16).
The long-term studies were associated with the greatest number of interventions achieving statistically significant differences in changes in HbA1C between the intervention and the control groups (87.5% significant vs. 12.5% non-significant, and accounting for 43.8% of the 16 studies that reported significant changes). This was followed by the short-term interventions (55.6% significant vs. 44.4% non-significant, and representing 31.2% of the 16 significant studies). In comparison, the medium-term programs were associated with the least number (50.0% significant vs. 50.0% non-significant, and accounting for 25.0% of the 16 significant studies) [Figures 2 and 3].
Discussion
Diabetes is a complex, chronic condition that requires both high-quality clinical care and effective self-management. While many factors affecting the effectiveness of SEM programs have been studied extensively, the impact of program length on the clinical outcomes of type 2 diabetics has received little research attention. The current study was, therefore, conducted as an attempt to fill this gap.
Generally, the outcomes reported by the studies showed positive effects. None of the studies that showed no significant changes indicated that patients’ HbA1c levels worsened after participating in the educational programs. Our findings support the literature that diabetes SME programs produce beneficial effects on patients’ glycemic control.78,79
Our analysis revealed that the majority of the long-term interventions were more effective on changes in HbA1c levels. Participants enrolled in the long-term programs also achieved the greatest overall mean reduction in HbA1c than the control subjects. Although not enough published studies on the topic exist for detailed comparisons, a 2009 technical report presented to the Ontario Health Technology Advisory Committee in Canada shares our findings. The report, which was based on a systematic review of type 2 diabetes SEM programs, concluded that interventions with the largest effects on glycemic control lasted at least one year in duration.79
One factor that differentiated the long-term studies from both the short and medium-term interventions was that most of the participants enrolled in the long-term programs received ongoing reinforcement in addition to the educational sessions. This was done through clinic visits,60,67 weekly support group sessions,70 and follow-up telephone calls.53,60,64,68 Reinforcing the themes addressed during the educational sessions might have provoked thoughts and emotional experiences, thus consolidating educational experiences. This may partly explain why most long-term interventions were more effective on changes in levels.
The claim that initial improvements in SME outcomes diminish after six months80,81 is partly supported by our review. The long-term studies had most (87.5%) of the interventions lasting six months. Initially, the interventions recorded significant improvements. However, not all could sustain these gains to the end or immediately after program implementation. It is possible the short-term interventions would have reported similar results if long term follow-up assessments were made. This suggests that one-time education is not sufficient for patients to sustain a lifetime of diabetes care. As theories of science and behavior changes argue: “Changing one’s health behavior is a complex process which does not occur rapidly”.82 Thus, patients will need ongoing self-management and support for a sustained behavior change.
Program length in terms of days, weeks, months, or years may not be the same as program length in terms of total hours of engagement. For instance, we found that two61,71 of the included studies had the same total hours of engagement (six hours). Whereas one61 was spread over three weeks, and the other71 was delivered in either one day or two half-day equivalents. In another study,56 though the total contact time was short (2.5 hours), educational sessions were spread over six months (sessions were given at intervals of three to six weeks and took between 15 and 45 minutes per session). Thus, depending on program intensity, an intervention can last several days, but with few contact hours. Therefore, it is vital for researchers to clarify this difference when analyzing the effect of program length on SEM interventions’ outcomes.
We observed that most of the studies included in this review did not blind those measuring and analyzing the interventions’ main outcomes. This observation is not surprising because research indicates that few randomized controlled studies report blinding data analysts and outcome assessors.83 As argued, outcome assessors who are aware of the actual treatment may unintentionally or consciously alter their assessment, thereby posing the risk of detection bias.84 Blinding data collectors, outcome assessors, and data analysts are crucial to ensure unbiased ascertainment of outcomes.85 Researchers find it difficult to blind outcome assessors because, in most cases, as we observed in our analysis, the principal investigators are themselves the outcome adjudicators. Future research should consider using independent individuals unaware of treatment allocations as outcome assessors to avoid this methodological error.
This study is among the few that have attempted to investigate the impact of DSME program length on glycemic control in adults with type 2 diabetes. It provides scientific evidence that may inform policy decisions about more cost-effective ways of implementing SEM interventions. Conclusions are based on high-quality evidence, as randomized controlled trials are considered the strongest research design for evaluating the effects of health interventions.86 That notwithstanding, the study has some methodological limitations which are worth acknowledging. A meta-analysis would have been the most appropriate method for determining the summary effects of the interventions in each of the three program lengths. However, because of intervention heterogeneity, it was not suitable to conduct a meta-analysis. The interventions differed with respect to a number of factors, including participants’ personal characteristics, mode of program delivery (e.g., group, individual, telephone, mail, online, video, etc.), and SME provider type. These factors could impact the programs’ outcomes hence, the inappropriateness of meta-synthesizing the information. Another limitation pertains to the rigorous inclusion and exclusion criteria we adopted. For instance, restricting the search strategy to only studies published in peer-reviewed English journals from January 2000 to April 2019 may have resulted in excluding useful information that may not have been peer-reviewed, in other languages, or published before 2000. Finally, focusing the analysis on only one clinical endpoint (HbA1C) may not represent a comprehensive evaluation of the success of the interventions. HbA1C was not the only primary outcome measure of the included studies; other physical, behavioral, and psychological endpoints were also considered.
Based on the evidence presented, one-time education may not be an effective intervention for achieving longer-term glycemic control in adults with type 2 diabetes. However, while one-time educational programs are not recommended, the current situation, where most SME interventions are organized separately from healthcare systems (mostly by voluntary organizations), makes it difficult for long-term, ongoing SEM programs to be provided. Integrating SME programs into diabetes care pathways is the surest way to achieve lifelong patient education and support. As full integration has not been attained yet, organizers of SME interventions should consider providing additional sessions periodically to reinforce what patients are taught in the educational programs. This will not only ensure cost-efficiency but will also result in long-lasting benefits to health and psychosocial outcomes.
Conclusion
Our findings suggest that program length may change the effectiveness of educational interventions. Long-term SMEs with reinforcement components appear to have the largest effects on glycemic control. Achieving sustained improvements in patients’ HbA1C levels will require long-term, ongoing SME, and support. However, it is worth noting that none of the included publications in this review directly measured the association between program length and SME outcomes. The effects of the interventions we observed may be due to factors other than program duration. For instance, we observed that the long-term interventions employed a mix of program delivery modes. Also, patients recruited into the various interventions had different baseline HbA1C values. Moreover, disease duration varied among the study participants. Our findings be interpreted as suggestive rather than being conclusive. This points to the need for more methodologically rigorous research to be conducted with diverse subject populations in real-world clinical and community settings to understand the actual impact of SME program length on physiological, behavioral, and patient-reported outcomes. Our study could provide background information for further developments.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Okpala P. Harnessing the power of collaborative leadership in the management of chronic health conditions. Int J Healthc Manag 2019;12(4):302-307.
- 2. World Health Organization. Innovative care for chronic conditions: building blocks for action: global report. Geneva: World Health Organization; 2002.
- 3. Samb B, Desai N, Nishtar S, Mendis S, Bekedam H, Wright A, et al. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet 2010 Nov;376(9754):1785-1797.
- 4. Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006 May;367(9524):1747-1757.
- 5. O’Halloran J, Miller GC, Britt H. Defining chronic conditions for primary care with ICPC-2. Fam Pract 2004 Aug;21(4):381-386.
- 6. Debussche X, Rollot O, Le Pommelet C, Fianu A, Le Moullec N, Régnier C, et al. Quarterly individual outpatients lifestyle counseling after initial inpatients education on type 2 diabetes: the REDIA Prev-2 randomized controlled trial in Reunion Island. Diabetes Metab 2012 Feb;38(1):46-53.
- 7. Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: a review of current trends. Oman Med J 2012 Jul;27(4):269-273.
- 8. Schinckus L, Van den Broucke S, Housiaux M; Diabetes Literacy Consortium. Assessment of implementation fidelity in diabetes self-management education programs: a systematic review. Patient Educ Couns 2014 Jul;96(1):13-21.
- 9. Pemu PE, Quarshie AQ, Josiah-Willock R, Ojutalayo FO, Alema-Mensah E, Ofili EO. Socio-demographic psychosocial and clinical characteristics of participants in e-HealthyStrides©: an interactive ehealth program to improve diabetes self-management skills. J Health Care Poor Underserved 2011;22(4)(Suppl):146-164.
- 10. Al-Lawati JA. Diabetes mellitus: a local and global public health emergency! Oman Med J 2017 May;32(3):177-179.
- 11. Bloom DE, Cafiero ET, Jané-Llopi E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. Global economic burden of non-communicable diseases. Program on the global demography of dging; 2012.
- 12. Saxe-Custack A, Weatherspoon L. A patient-centered approach using community-based paraprofessionals to improve self-management of type 2 diabetes. Am J Health Educ 2013;44(4):213-220 .
- 13. Samad N, Samad N, Abdallah S. Use of social marketing in diabetes control in the UAE context. Int J Healthc Manag 2018;11(1):1-7.
- 14. Fan L, Sidani S. Effectiveness of diabetes self-management education elements: a meta-analysis. Can J Diabetes 2009;33(1):18-26.
- 15. Ayed MB, Aoud NE. The patient empowerment: a promising concept in healthcare marketing. Int J Healthc Manag 2017;10(1):42-48.
- 16. Simmons D, Cohn S, Bunn C, Birch K, Donald S, Paddison C, et al. Testing a peer support intervention for people with type 2 diabetes: a pilot for a randomised controlled trial. BMC Fam Pract 2013 Jan;14(1):5.
- 17. Habibzadeh H, Sofiani A, Alilu L, Gillespie M. The effect of group discussion-based education on self-management of adults with type 2 diabetes mellitus compared with usual care: a randomized control trial. Oman Med J 2017 Nov;32(6):499-506.
- 18. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care 2012 Jan;35(Suppl 1):S101-S108.
- 19. Duke SA, Colagiuri S, Colagiuri R. Individual patient education for people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2009 Jan;21(1):CD005268.
- 20. Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, Peacock R, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev 2013 Mar;3(3):CD008776.
- 21. Anderson JW, Kendall CW, Jenkins DJ. Importance of weight management in type 2 diabetes: review with meta-analysis of clinical studies. J Am Coll Nutr 2003 Oct;22(5):331-339.
- 22. Siminerio L, Ruppert K, Huber K, Toledo FG. Telemedicine for Reach, Education, Access, and Treatment (TREAT): linking telemedicine with diabetes self-management education to improve care in rural communities. Diabetes Educ 2014 Nov-Dec;40(6):797-805.
- 23. Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ 2003 May-Jun;29(3):488-501.
- 24. Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2005 Apr;(2):CD003417.
- 25. Captieux M, Pearce G, Parke HL, Epiphaniou E, Wild S, Taylor SJ, et al. Supported self-management for people with type 2 diabetes: a meta-review of quantitative systematic reviews. BMJ Open 2018 Dec;8(12):e024262.
- 26. Boren SA, Gunlock TL, Schaefer J, Albright A. Reducing risks in diabetes self-management: a systematic review of the literature. Diabetes Educ 2007 Nov-Dec;33(6):1053-1077, discussion 1078-1079.
- 27. Duncan I, Birkmeyer C, Coughlin S, Li QE, Sherr D, Boren S. Assessing the value of diabetes education. Diabetes Educ 2009 Sep-Oct;35(5):752-760.
- 28. Gregg EW, Chen H, Wagenknecht LE, Clark JM, Delahanty LM, Bantle J, et al; Look AHEAD Research Group. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012 Dec;308(23):2489-2496.
- 29. Martin AL, Lipman RD. The future of diabetes education: expanded opportunities and roles for diabetes educators. Diabetes Educ 2013 Jul-Aug;39(4):436-446.
- 30. Morrison F, Shubina M, Turchin A. Lifestyle counseling in routine care and long-term glucose, blood pressure, and cholesterol control in patients with diabetes. Diabetes Care 2012 Feb;35(2):334-341.
- 31. Deakin TA, McShane CE, Cade JE, Williams R. Group-based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Collaboration; 2009.
- 32. Berzins K, Reilly S, Abell J, Hughes J, Challis D. UK self-care support initiatives for older patients with long-term conditions: a review. Chronic Illn 2009 Mar;5(1):56-72.
- 33. Zwar N, Harris M, Griffiths R, Roland M, Dennis S, Powel Davies G, Hassan I. A systematic review of chronic disease management. Research Centre for Primary Health Care and Equity, School of Public Health and Community Medicine, UNSW; 2006.
- 34. Chaplin H, Hazan J, Wilson P. Self-management for people with long-term neurological conditions. Br J Community Nurs 2012 Jun;17(6):250-254, 256-257.
- 35. Naylor C, Imison C, Addicott R. Transforming our health care system: ten priorities for commissioners. King’s Fund, London. 2013 [cited 2017 January 21]. Available from: http://tinyurl.com/d35hlhb.
- 36. Foster G, Taylor SJ, Eldridge S, Ramsay J, Griffiths CJ. Self-management education programmes led by lay leaders for people with chronic health conditions. Cochrane Collaboration; 2009.
- 37. Coleman S, Briffa K, Conroy H, Prince R, Carroll G, McQuade J. Short and medium-term effects of an education self-management program for individuals with osteoarthritis of the knee, designed and delivered by health professionals: a quality assurance study. BMC Musculoskelet Disord 2008 Sep;9(1):117.
- 38. Anderson RM, Barr PA, Edwards GJ, Funnell MM, Fitzgerald JT, Wisdom K. Using focus groups to identify psychosocial issues of urban black individuals with diabetes. Diabetes Educ 1996 Jan-Feb;22(1):28-33.
- 39. Artinian NT, Magnan M, Christian W, Lange MP. What do patients know about their heart failure? Appl Nurs Res 2002 Nov;15(4):200-208.
- 40. Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nurs 2008 Apr;62(1):74-83.
- 41. Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Ann Behav Med 2010 Dec;40(3):325-342.
- 42. Sousa VD, Zauszniewski JA, Musil CM, Price Lea PJ, Davis SA. Relationships among self-care agency, self-efficacy, self-care, and glycemic control. Res Theory Nurs Pract 2005;19(3):217-230.
- 43. Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med 2005 Feb;20(2):175-184.
- 44. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract 2011 Jul;93(1):1-9.
- 45. Fitzgerald JT, Anderson RM, Davis WK. Gender differences in diabetes attitudes and adherence. Diabetes Educ 1995 Nov-Dec;21(6):523-529.
- 46. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs 2005 Dec;52(5):546-553.
- 47. Lillyman S, Farquharson N. Self-care management education models in primary care. Br J Community Nurs 2013 Nov;18(11):556-560.
- 48. Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: A systematic review of the effect on glycemic control. Patient Educ Couns 2016 Jun;99(6):926-943.
- 49. Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes 2008;26(2):77-82 .
- 50. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998 Sep;352(9131):854-865.
- 51. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al; UK Prospective Diabetes Study Group. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000 Aug;321(7258):405-412.
- 52. Higgins JP, Green S. Cochrane Handbook for systematic reviews of interventions, version 5.1.0. Cochrane Collaboration; 2011.
- 53. Wolf AM, Conaway MR, Crowther JQ, Hazen KY, L Nadler J, Oneida B, et al; Improving Control with Activity and Nutrition (ICAN) Study. Translating lifestyle intervention to practice in obese patients with type 2 diabetes: Improving Control with Activity and Nutrition (ICAN) study. Diabetes Care 2004 Jul;27(7):1570-1576.
- 54. Samuel-Hodge CD, Keyserling TC, Park S, Johnston LF, Gizlice Z, Bangdiwala SI. A randomized trial of a church-based diabetes self-management program for African Americans with type 2 diabetes. Diabetes Educ 2009 May-Jun;35(3):439-454.
- 55. Scain SF, Friedman R, Gross JL. A structured educational program improves metabolic control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Educ 2009 Jul-Aug;35(4):603-611.
- 56. Goudswaard AN, Stolk RP, Zuithoff NP, de Valk HW, Rutten GE. Long-term effects of self-management education for patients with Type 2 diabetes taking maximal oral hypoglycaemic therapy: a randomized trial in primary care. Diabet Med 2004 May;21(5):491-496.
- 57. Shakibazadeh E, Bartholomew LK, Rashidian A, Larijani B. Persian Diabetes Self-Management Education (PDSME) program: evaluation of effectiveness in Iran. Health Promot Int 2016 Sep;31(3):623-634.
- 58. Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X-PERT Programme makes a difference. Diabet Med 2006 Sep;23(9):944-954.
- 59. Forjuoh SN, Ory MG, Jiang L, Vuong AM, Bolin JN. Impact of chronic disease self-management programs on type 2 diabetes management in primary care. World J Diabetes 2014 Jun;5(3):407-414.
- 60. Moriyama M, Nakano M, Kuroe Y, Nin K, Niitani M, Nakaya T. Efficacy of a self-management education program for people with type 2 diabetes: results of a 12 month trial. Jpn J Nurs Sci 2009 Jun;6(1):51-63.
- 61. Merakou K, Knithaki A, Karageorgos G, Theodoridis D, Barbouni A. Group patient education: effectiveness of a brief intervention in people with type 2 diabetes mellitus in primary health care in Greece: a clinically controlled trial. Health Educ Res 2015 Apr;30(2):223-232.
- 62. Spencer MS, Rosland AM, Kieffer EC, Sinco BR, Valerio M, Palmisano G, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health 2011 Dec;101(12):2253-2260.
- 63. Sun J, Wang Y, Chen X, Chen Y, Feng Y, Zhang X, et al. An integrated intervention program to control diabetes in overweight Chinese women and men with type 2 diabetes. Asia Pac J Clin Nutr 2008;17(3):514-524.
- 64. Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care 2005 Apr;11(4):253-260.
- 65. Sevick MA, Korytkowski M, Stone RA, Piraino B, Ren D, Sereika S, et al. Biophysiologic outcomes of the enhancing adherence in type 2 diabetes (ENHANCE) trial. J Acad Nutr Diet 2012 Aug;112(8):1147-1157.
- 66. Rosal MC, Ockene IS, Restrepo A, White MJ, Borg A, Olendzki B, et al. Randomized trial of a literacy-sensitive, culturally tailored diabetes self-management intervention for low-income latinos: latinos en control. Diabetes Care 2011 Apr;34(4):838-844.
- 67. Jacobs M, Sherry PS, Taylor LM, Amato M, Tataronis GR, Cushing G. Pharmacist assisted medication program enhancing the regulation of diabetes (PAMPERED) study. J Am Pharm Assoc (2003) 2012 Sep-Oct;52(5):613-621.
- 68. Johansen OE, Gullestad L, Blaasaas KG, Orvik E, Birkeland KI. Effects of structured hospital-based care compared with standard care for Type 2 diabetes-The Asker and Baerum Cardiovascular Diabetes Study, a randomized trial. Diabet Med 2007 Sep;24(9):1019-1027.
- 69. Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med 2005 Jun;29(3):225-235.
- 70. Brown SA, Garcia AA, Kouzekanani K, Hanis CL, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care 2002 Feb;25(2):259-268.
- 71. Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, et al; Diabetes Education and Self Management for Ongoing and Newly Diagnosed Collaborative. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ 2008 Mar;336(7642):491-495.
- 72. Dyson PA, Beatty S, Matthews DR. An assessment of lifestyle video education for people newly diagnosed with type 2 diabetes. J Hum Nutr Diet 2010 Aug;23(4):353-359.
- 73. Williams ED, Bird D, Forbes AW, Russell A, Ash S, Friedman R, et al. Randomised controlled trial of an automated, interactive telephone intervention (TLC Diabetes) to improve type 2 diabetes management: baseline findings and six-month outcomes. BMC Public Health 2012 Aug;12(1):602.
- 74. Huang MC, Hsu CC, Wang HS, Shin SJ. Prospective randomized controlled trial to evaluate effectiveness of registered dietitian-led diabetes management on glycemic and diet control in a primary care setting in Taiwan. Diabetes Care 2010 Feb;33(2):233-239.
- 75. Abdulah DM, Hassan AB, Saadi FS, Mohammed AH. Impacts of self-management education on glycaemic control in patients with type 2 diabetes mellitus. Diabetes Metab Syndr 2018 Nov;12(6):969-975.
- 76. Khunti K, Gray LJ, Skinner T, Carey ME, Realf K, Dallosso H, et al. Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ 2012 Apr;344(2):e2333.
- 77. Gathu CW, Shabani J, Kunyiha N, Ratansi R. Effect of diabetes self-management education on glycaemic control among type 2 diabetic patients at a family medicine clinic in Kenya: A randomised controlled trial. Afr J Prim Health Care Fam Med 2018 Nov;10(1):e1-e9.
- 78. Steinsbekk A, Rygg LO, Lisulo M, Rise MB, Fretheim A. Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv Res 2012 Jul;12(1):213.
- 79. Medical Advisory Secretariat. Behavioural interventions for type 2 diabetes: an evidence-based analysis. Ont Health Technol Assess Ser 2009;9(21):1-45.
- 80. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care 2010 Jan;33(Suppl 1):S89-S96.
- 81. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002 Jul;25(7):1159-1171.
- 82. Ryan P. Integrated Theory of Health Behavior Change: background and intervention development. Clin Nurse Spec 2009 May-Jun;23(3):161-170, quiz 171-172.
- 83. Karanicolas PJ, Bhandari M, Taromi B, Akl EA, Bassler D, Alonso-Coello P, et al. Blinding of outcomes in trials of orthopaedic trauma: an opportunity to enhance the validity of clinical trials. J Bone Joint Surg Am 2008 May;90(5):1026-1033.
- 84. Probst P, Grummich K, Heger P, Zaschke S, Knebel P, Ulrich A, et al. Blinding in randomized controlled trials in general and abdominal surgery: protocol for a systematic review and empirical study. Syst Rev 2016 Mar;5(1):48.
- 85. Karanicolas PJ, Farrokhyar F, Bhandari M. Practical tips for surgical research: blinding: who, what, when, why, how? Can J Surg 2010 Oct;53(5):345-348.
- 86. Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, et al; CONSORT GROUP (Consolidated Standards of Reporting Trials). The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med 2001 Apr;134(8):663-694.