Responding to the global alert by the World Health Organization (WHO) on the Coronavirus disease 2019 (COVID-19) pandemic on 20 January 2020, most countries undertook immediate actions to contain the spread of this disease. Nevertheless, the number of people infected by COVID-19 has increased exponentially since January 2020 due to traveling and contact with COVID-19 infected individuals. Various measures have been contemplated in various parts of the world to curb the proliferation of COVID-19. Despite such undertaking, as of 15 April 2020 more than 2 million cases were confirmed with 138 000 reported deaths worldwide.1
COVID-19 emerged in Wuhan, China, in December 2019, and currently, most countries are at different stages of disease transmission.2 Despite its similarities to the Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) and the Middle East Respiratory Syndrome coronavirus (MERS-CoV),3 COVID-19 is distinct in terms of community spread and severity. Specifically, the nature of COVID-19 and its behavior across populations is still under research. In this regard, the experience from public health preparedness and response for COVID-19 is building up, and these experiences must be described and reported for peer review of public health experts and utilization by various stakeholders.
The WHO has defined four transmission scenarios/phases for COVID-19 worldwide: 1) countries with no cases (no cases); 2) countries with one or more cases, imported or locally detected (sporadic cases); 3) countries experiencing cases clusters in time, geographic location, and/or common exposure (clusters of cases); and 4) countries experiencing larger outbreaks of local transmission (community transmission).1,2 Evidence from China reported the positive impact of quarantine, social distancing, and isolation of infected populations to contain the epidemic in China, which encouraged many other countries to do the same.4 These measures have saved lives and allowed many countries to increase readiness for the appearance of COVID-19.
On 10 March 2020, His Majesty the Sultan of Oman, Sultan Haitham bin Tariq Al-Said, gave orders to initiate a supreme committee to implement the necessary measures at the appropriate scale to reduce COVID-19 transmission and any anticipated public and socio-economic impacts. The committee was chaired by the Minister of Interior Affairs and included different governmental sectors, including the Ministry of Health (MoH). The preparedness and response initiated by the MoH for COVID-19 were thus scaled up, aimed at strengthening the health emergency response systems, increase capacity to screen/detect and manage patients, ensure availability of adequate medical supplies and necessary personnel, and develop life-saving medical interventions.
Primary health care (PHC) is the gate to health care and captures the vast majority of the population, making it an ideal setting for the first line of defense from COVID-19.5 Ideally, the PHC provides curative, preventive, health-promoting, and rehabilitative services. Delivery of PHC services in Oman conducted by trained physicians, nurses, and allied professions such as health educators and dietitians.
At the beginning of 2018, the national population estimates were 4 660 153, with approximately 45% being non-Omanis, indicating significant growth (or immigration). About 32% of the total population live in Muscat.6 In Muscat governorate, there are 30 PHC centers, three polyclinics, and three hospitals all under the direct administration of the Directorate General of Health Services. The health centers are scattered across six willayats/regions in Muscat: A'Seeb (n = 9), Bawshar (n = 6), Mutrah (n = 5), Muscat (n = 3), Al Amirat (n = 4), and Qurayyat (n = 3).
The purpose of this paper is to summarise the trend of COVID-19 positive cases in Muscat governorate from 1 January to mid-April 2020 and describe the related responses to COVID-19 in PHC settings. The descriptive analysis frameworks are the epidemiology of case scenarios in Oman7 and the six WHO building blocks of the health care system framework.8,9 The stepped case scenarios include phase one: preparedness, phase two: high risk of imported cases, phase three: imported cases, phase four: clusters of secondary local transmission, and phase five: clusters of community transmission.7
Methods
This is a descriptive cross-sectional study aimed to describe the trends of laboratory-confirmed positive COVID-19 cases in Muscat and the responses against the disease utilizing the health system building blocks including: 1) health care leadership and governance; 2) health workforce; 3) service delivery; 4) medical products and technologies; 5) health information systems; and 6) health system financing.
Data were extracted from the health information system within the department of diseases surveillance and control, Muscat. Information on the scaled-up organizational response was derived from the regional alert reports prepared fortnightly by the department of disease surveillance and control. Responses were categorized to fit the definitions of WHO health system building blocks. The categorization was cross-checked independently by three researchers (LA, HA, and FA). The final categorization was revised by an expert researcher (KP) as a further measure of inter-rater reliability. Continuity of reporting responses was ensured by one researcher (TA), responsible for the data management and analysis. Written responses were re-visited whenever conflicting interpretations occurred. Ethical approval was obtained from the regional research review and ethical approval committee.
Continuous variables were expressed as whole numbers to show/describe trends over time. Due to the descriptive nature of this study, there were no inferential statistics performed.
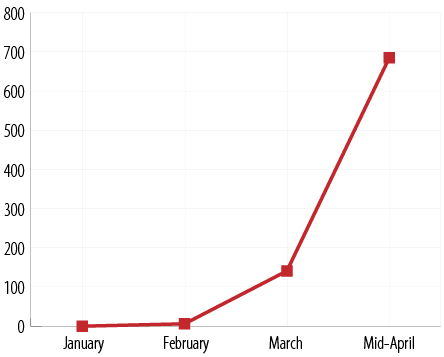
Figure 1: Number of confirmed COVID-19 cases in Muscat governorate from January to mid-April 2020.
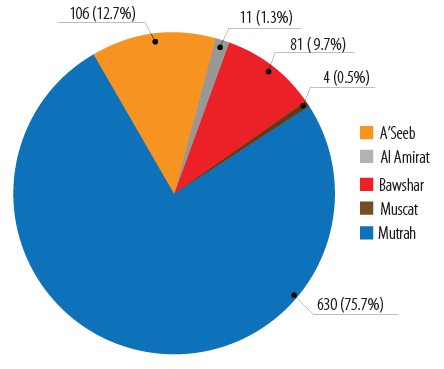
Figure 2: Distribution of COVID-19 confirmed cases across the willayats of Muscat governorate.
Results
The first case of COVID-19 in Muscat governorate was confirmed on the 23 February 2020 linked to travel from abroad. There has been an exponential increase in the number of cases reaching 832 cases in mid-April [Figure 1].
The increase was prominent in community clusters within Mutrah [Figure 2], especially among the expatriates/non-nationals (> 70.0%).
Organizational responses at the PHC level across the WHO building blocks for health care system [Table 1].
With the first alert from China about the COVID-19 in January 2020, the national and regional public health emergency task force groups in MoH were activated. The regional operation center (ROC) is composed of 12 teams, all under the direct command of the director-general of health services. These teams coordinate with one another throughout the phases of the disease to adhere to daily action plans:
- Ports of entry (POE).
- Clinical health care (primary, secondary, and hospital) and support services.
- Infection prevention and control (IPC).
- Disease surveillance and response.
- Health information system.
- Information technology.
- Health services for isolated/quarantined individuals.
- Pharmacy and medical supplies.
- Private establishments.
- Health awareness and social media.
- Administration and finance.
- Studies and research.
In phase one of the epidemiological scenario, the focus was preparedness and risk assessments in all POE, namely Muscat International Airport and Al Fahal and Sultan Qaboos seaports [Table 1]. With the increase in the number of positive cases among travelers from the affected areas, the supreme committee in March 2020 provided coordination between all national sectors. The supreme committee requested a complete closure of air, sea, and land ports and the shutdown of Mutrah where multiple clusters were initially identified, followed by the closure of the whole of Muscat governorate on 10 April 2020. These measures were accompanied by a range of social distancing measures, including the closure of schools, universities, mosques, sports activities, cinemas, parks, and even restricting all movement in some of the most affected regions (Mutrah and Muscat).
Several measures were put in place as the epidemiological case scenarios were progressing. Initially, staff numbers and duties were revised. Then, exposure risk assessment and classification were enhanced throughout the phases. In phase three and four, outreach teams and public-private partnerships were established. Volunteers from the community and non-governmental organizations were actively involved from phase three onwards. They were all trained on IPC measures by the concerned team in the ROC.
Table 1: Responses to COVID-19 across the epidemiological case scenarios utilizing the WHO health system building blocks.
|
Definition |
No cases (preparedness) |
First case detected (imported cases) |
Clusters of secondary local transmission |
Clusters of cases |
Clusters of community transmission |
|
Aim |
Preparedness planning, risk assessment, coordination, and resource mobilization |
Quarantine, stop transmission, and prevent spread |
Limit extend of transmission to contain within clusters and continuing mitigation efforts |
Containment measures, slow transmission, end community outbreaks |
|
Focus |
Preparedness and risk management (using declaration forms) at ports of entry |
Screen arrivals
from affected countries activate quarantine facilities and emergency responses |
Social distancing measures
Revise industrial policies |
Early identification of hotspots and detection of cases
Isolation of positive cases |
Early identification of clusters Isolation of Mutrah 1 April 2020
Expand geographical isolation of areas (Muscat governorate)
10 April 2020
Enhance surveillance activities |
|
Leadership and governance |
National and regional COVID-19 task force |
Supreme national committee Suspend flights from the affected
countries |
Activation of the National Committee of Civil Defence
Add other countries to quarantine list (China, South Korea, Japan, Singapore, and Iran)
Activation of vital sectors: the national medical and public health response, rescue and sheltering
Isolation of areas with clusters of community transmission |
|
Health workforce |
Human resource deployment and remobilization |
Enhance health care workers exposure risk assessment and classification
Initiation of outreach teams
Facilitate public-private partnership
Organize support from volunteers |
Augment medical services access for all at the ground level by reorienting HCW
Establish efficient triaging mechanism for detection of high risk cases through orientation training |
|
Service delivery |
|
|
|
|
|
|
Health care services |
Revise essential health care needs, human resources, and
working hours
Liaise with hospitals |
Identify COVID-19 primary care center
(North Al Khuwair) |
Strengthen referral protocols, IPC, swab taking, and transfer of specimens to the central laboratories |
Expand services at Mutrah health center
Preparation of a community areas/tent to perform a community surveillance activity in Mutrah
Identify outreach teams
Expand isolation facilities especially for foreigners |
| |
Prepare plans for a surge in the number of cases
Use telemedicine |
Identify doctors on call to answer public queries
Monitor out-patient department visits |
Arrange continuity of services for vulnerable groups and immunization program |
Provide multiple testing facilities (Mutrah, Darset, Asharadi,
and Russail) |
|
Emergency response mechanisms |
Preparedness phase |
Enhancing patient referral pathways and coordination between tertiary hospitals and with private institution
Arranging ambulance services |
Activate emergency response mechanisms
Scale-up emergency response mechanisms |
|
Case management and related
guidelines |
Set-up screening and triage protocols at points of access to the primary care |
Setting up facilities for isolation of suspected cases
(arrivals from abroad)_22 hotel
Test suspected cases according to the case definition |
Scale-up surge plans for health and isolation facilities (suspected and positive cases)
Set-up COVID-19 hotlines to strengthen the referral system to hospitals |
Prepare mass isolation facilities for positive mild cases
Strengthen outbreak control measures in Mutrah area
Enhancing passive surveillance in other willayats
Enhancing capacity for testing and medical services in Mutrah health center (HC)
Support private sector participation in Mutrah HC |
|
Drills and simulation exercises |
Practice regular exercises to test plans, protocols, communication, multi-sectoral coordination, and operational capabilities.
Enhance capacity building and strengthening activities |
|
Medical products and technologies |
|
Laboratory testing |
Ensure availability of testing tools.
Test all individuals meeting the suspected case definition. |
Activate laboratory
contingency plans |
Implement prioritized testing and measures that can reduce spread |
|
Pharmacy |
Review daily
inventories and requirements |
Scale-up stock from regular consumption
Provide institutional isolation facilities with the required supplies |
Activate WhatsApp services to prepare prescriptions
Create safe windows to pick up medication in health centers
Start home delivery services
Use social media platforms to inform the public on collection, uses, and information about medication |
|
Surveillance activities |
|
Case finding, contact tracing and management |
Prepare resources.
Conduct active case finding, contact tracing, and monitoring; quarantine of contacts |
Enhance active case finding, contact tracing, monitoring, quarantine of contacts, and isolation of cases |
Intensify case finding, contact tracing, monitoring, quarantine, and isolation facilities |
Continue active case finding, contact tracing where possible, especially in newly infected areas
Implement COVID-19 surveillance
Start “al trassud” web-based notification (government
and private)
Assign focal points in all institutes for data update |
ROC: regional operation center; HCW: health care worker; IPC: infection prevention and control; POE: ports of entry; GIS: geographical information system; ARI: acute respiratory tract infection.
Adaptations across primary, secondary, and tertiary care services included strengthening the emergency response mechanisms, risk communication and public engagement, public health measures, IPC, case management, and drills with simulation exercises.
Despite reductions in out-patient department visits from 115 324 in January to 109 719 in March, essential health services were ensured in all health centers, primarily for vulnerable groups, women, and children.
A COVID-19 model health center was established in phase two to provide coordinated support with all ROC teams. With the situation escalating in Mutrah, health centers in Mutrah were opened for 24 hours to ensure that testing and isolation procedures were in place.
Care services were restructured to implement COVID-19 triaging, screening, and quarantine/isolation algorithms as indicated. All staff underwent several trainings and exercises on protocols, communication, multi-sectoral coordination, and operational capabilities, swab taking, referrals and management of symptomatic/asymptomatic patients.
Phone consultations and virtual communications were utilized to respond to public queries. Moreover, public health awareness campaigns on the importance of social distancing and hand hygiene were carried out. Importantly, the nursing cadre took the responsibility of setting up isolation facilities for suspected cases (arrivals from abroad) and positive cases; and thus, 22 hotels were arranged for this purpose. Additionally, mass isolation facilities for positive mild positive cases in phases three and four were arranged (e.g., the Oman National Engineering and Investment (ONEIC)).
Overall, shortages of supplies have been reported on personal protective equipment (PPE) and face masks, and it has been a concern in all regions leading to strict measures of use. Every effort was made to reduce the influx of patients to health centers via scaling up pharmacy stock from regular consumption and implementing WhatsApp and home delivery services to transport regular drugs to patients.
Furthermore, two central stores for PPE (Mutrah and A'Seeb) were opened in phases three and four to accommodate the escalating demand. Also, the pharmacy and medical supply team in ROC was responsible for providing institutional isolation facilities with the required pharmaceutical supplies.
The use of technology was implemented throughout the epidemiological phases, as most health centers conducted phone consultations and video conferencing to share experiences. The geographical information system was introduced in February 2020 to ease data management and graphical interpretations.
Data sharing, specifically the number of confirmed cases, was widely considered to have been provided by authorities at all levels promptly via social media.
Because MoH is a public health care delivery system, finance management was not within this paper’s scope. However, with the economic recession, additional financial resources are warranted to support the implementation of COVID-19 interventions.
Discussion
This is the first paper to report the changes in primary care responses with the increase in cases of COVID-19 utilizing the WHO health system building blocks in an Arabic speaking country, Oman. Based on the experiences described in Table 1 and ‘real-life’ scenarios, this discussion is structured to highlight approaches to strengthen the medical and public health responses to mass crisis.
A comprehensive multi-sectoral approach was especially crucial as new cases of the COVID-19 continued to surge in Muscat. This approach potentially alleviated the fear of exhausting current health care resources and shortages of competent health care personnel and essential medical supplies.10 With the experience from Muscat governorate, It was clear that an effective pandemic response required a whole-of-government, whole-of-society approach.11,12 This mandated the involvement and partnership with multi-sectoral capacities and resources including the private sector, non- governmental organizations and civil society.13
Additionally, with the disease surge among expatriates (the case in Mutrah willayat), there was a growing acknowledgment that the public and the private partnerships were compulsory to solidify Universal Health Coverage defined as equity and social justice to accessing health care.13,14 In Oman, the Sultan of Oman, declared free of charge medical services against COVID-19 to all expatriates living in Oman in April 2020 until a decreased transmission rate
is achieved.
Similar to the experience in Muscat (Mutrah willayat and ONEIC), a private network in the UAE made staff and hospital bed capacity available to government use as needed.15 Also, in Bahrain, licenses were provided to private healthcare providers for the management of COVID-19.16 However, the role of the private health sector could be expanded to enroll hospitals and laboratories to fill gaps in healthcare provision and coverage.13 Other potential areas of engagement could be nursing home facilities and social support and care to vulnerable populations.
Responding to the COVID-19 outbreak in Muscat revealed the need for public health/field epidemiologist expertise in PHC. In crises of such an over whelming scale, using the best available evidence is essential to save lives. Public health responses to emerging pandemics works on sound principles of established infectious disease epidemiology. Hence, knowledge of such principles and skills are essential in health care. Further research is required to explore effective methods to institutionalize and strengthen public health/epidemiological strategies within the health care setting.17
Technologies such as the use of geographical information technologies for big data are fundamental to maximize public health responses.18 Countries such as Taiwan, used location sharing in phones to track people inquarantine.18 Future direction may consider accelerating the use of novel technology, such as artificial intelligence, digital tools, and machine learning to achieve better medical and public health outcomes.
This pandemic has demonstrated that sharing real-time information is critical and mandatory. Lack of data sharing and a transparent reporting system may weaken health systems and may open windows for ‘infodemic’, false social media.19,20 The efforts in Muscat governorate in line with the national level mandates have been building a platform for data sharing and this has been affected by the surveillance platform that integrated quarantine services, patient records, laboratory data as well as follow-up information of confirmed cases. This platform is a success story in the development of robust, sustainable platforms for the future.
Conclusion
PHC is considered as the first responder for a mass crisis, namely COVID-19. It is crucial to enhance capacities and resources across the health system building blocks as the epidemiological case scenarios surge. Building a comprehensive, multi-sectoral approach, partnership with the private sectors, use of innovative technologies, and data sharing are the core for an effective medical and public health response.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
We would like to thank Dr. Padma Mohan Kurup for his outstanding contribution and care in strengthening the public health and epidemiological skills within the regional response to COVID-19.
references
- 1. World Health Organization. Coronavirus disease (COVID-2019) situation reports. 2020. [cited 2020 April 16]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- 2. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020 Apr;382(18):1708-1720.
- 3. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020 Feb;395(10223):497-506.
- 4. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020 Mar;395(10228):931-934.
- 5. World Health Organization Decleration. Declaration of Alma-Ata. 1978. [cited 2020 March 22]. Available from: http://www.who.int/publications/almaata_declaration_en.pdf.
- 6. National Centre For Statistics and Information. 2018.[cited 2020 April 23]. Available from: https://ncsi.gov.om/Pages/NCSI.aspx.
- 7. Ministry of Health. Regional plan of Action. In: control Dsa, editor. Oman; 2020.
- 8. Legido-Quigley H, Mateos-García JT, Campos VR, Gea-Sánchez M, Muntaner C, McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health 2020 May;5(5):e251-e252.
- 9. World Health Organization. Innovative Care for Chronic Conditions: Building Blocks for Action. Geneva: WHO; 2002.
- 10. Horowitz J. Italy’s Health Care System Groans Under Coronavirus a Warning to the World. The New York Times. 2020.
- 11. Kim D-H. Structural Factors of the Middle East Respiratory Syndrome Coronavirus Outbreak as a Public Health Crisis in Korea and Future Response Strategies. J Prev Med Public Health 2015 Nov;48(6):265-270.
- 12. Schwartz J, Yen MY. Toward a collaborative model of pandemic preparedness and response: Taiwan’s changing approach to pandemics. Journal of microbiology, immunology, and infection Wei mian yu gan ran za zhi 2017;50(2): 125-32.
- 13. World Health Organization. The private sector and universal health coverage. 2019. [cited 2020 April 19]. Available from: https://www.who.int/bulletin/volumes/97/6/18-225540/en/.
- 14. Shepp J. Coronavirus Is the Last Thing the Middle East Needs Right Now. 2020. [cited 2020 April 12]. Available from: https://nymag.com/intelligencer/2020/03/coronavirus-is-the-last-thing-themiddle.
- 15. Khaleej Times. Coronavirus crisis: Thumbay Group aligns with UAE government’s precautionary policies. 2020.
- 16. Bahrain Ministry of Health. Coronavirus (COVID-19) latest update 2020. [cited 2020 April 15]. Available from: https://www.moh.gov.bh/COVID19/Details/4064.
- 17. Koon AD, Windmeyer L, Bigdeli M, Charles J, El Jardali F, Uneke J, et al. A scoping review of the uses and institutionalisation of knowledge for health policy in low- and middle-income countries. Health Res Policy Syst 2020 Jan;18(1):7.
- 18. Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA 2020 Apr;323(14):1341-1342.
- 19. World Health Organization. An action plan to engage the private sector in the response to COVID-19. 2020. [cited 2020 April 16]. Available from: https://hsgovcollab.org/en/node/4365.
- 20. Lu D, Jennifer B. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerging. Infect Dis J 2020;26(7).