Sarcoidosis is a systemic disease of unknown etiology affecting multiple organs and is characterized by the presence of non-caseating granulomas.1 Although the etiology is unknown, the evidence points to an exaggerated immune response to an unidentified antigen as the most likely cause.2 Confirmatory evidence of the presence of non-caseating granuloma is needed to establish the diagnosis. Moreover, other causes of granulomatous disease should be ruled out before diagnosing a patient with sarcoidosis.3 Sarcoidosis commonly affects the lungs, lymphoid system, liver, and skin.3 While sarcoidosis of the male reproductive system (i.e., testis, epididymis, and prostate) has been reported, penile sarcoidosis is rare, and only a few case reports have been published.4–10
Case report
A 63-year-old African man presented to the University Health Center of Sultan Qaboos University, Muscat, Oman with a six-month history of painless penile swelling. The patient denied any history of genital trauma, urethral discharge, or any other urinary symptom. The patient had no other skin lesions. He was married and had no extra-marital relationships. Examination revealed a 1 × 2 cm firm and non-tender nodule in the ventral part of the penis. The patient was referred to the urology clinic where he had an excisional biopsy of the swelling. Histopathology of the lesion showed epithelioid histiocytes palisading around a nuclear dermis with mucin deposition, which was suggestive of granuloma annulare [Figure 1].
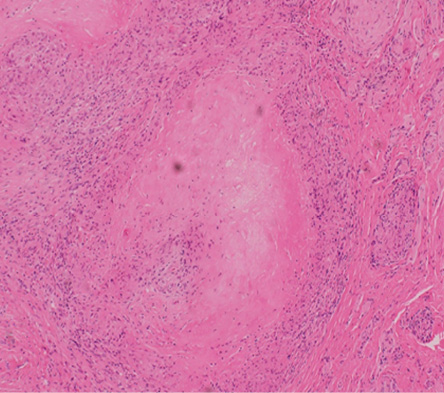
Figure 1: Histological section of the penile lesion showing granuloma annulare. Localized necrotic collagen surrounded by lymphocytes.
Magnification = 10 ×.
One year later, the patient presented with similar painless skin nodules, but over his right upper limb. These skin nodules had subsequently spread to involve his chest and trunk. He did not report any respiratory symptoms, fever, or joint pain. Family history was unremarkable, particularly for any similar symptoms or malignancies.
On examination, the patient was well-built, and he looked comfortable. He had no palpable cervical or axillary lymph nodes. There were multiple 1 × 2 cm, firm and non-tender subcutaneous nodules over the right arm, chest, and trunk. His chest was clear, and his cardiovascular examination was normal.
Laboratory tests, which included complete blood count, fasting blood glucose, and liver function tests, were all normal. His renal function tests showed features suggestive of an acute kidney injury with high creatinine level and low glomerular filtration rate (GFR). The levels of potassium and bicarbonate were within the normal range. A summary of the results of his laboratory tests is shown in Table 1.
Table 1: Summary of laboratory test results in a 68-year-old male with a history of penile swelling.
|
Hemoglobin |
13.1 |
12.1–16.3 g/dL |
|
WBC |
8 |
4.0–11.1 × 109/L |
|
Platelet count |
316 |
150–400 × 109/L |
|
BUN |
8.8 |
2.8–8.1 mmol/L |
|
Creatinine |
205 |
59–104 umol/L |
|
GFR |
28 |
1.73 mL/min/m2 |
|
K |
4.8 |
3.5–5.1 mmol/L |
|
Bicarbonate |
25 |
22–29 mmol/L |
|
ESR |
37 |
0–22 mm/hr |
|
ALT |
23 |
0–41 U/L |
|
AST |
87 |
0–40 U/L |
|
Calcium |
3.35 |
2.15–2.55 mmol/L |
|
PTH |
0.4 |
1.6–9.3 pmol/L |
|
Albumin |
45 |
35–52 g/L |
|
CRP |
<1 |
0–5 mg/L |
WBC: white blood count; BUN: blood urea nitrogen; GFR: glomerular filtration rate; K: potassium; ESR: erythrocyte sedimentation rate;
ALT: alanine aminotransferase; AST: aspartate aminotransferase;
PTH: parathyroid hormone; CRP: C-reactive protein; ACE: angiotensin-converting enzyme.
His chest X-ray revealed a superior mediastinal mass with a bilateral hilar enlargement [Figure 2]. Chest computed tomography showed multiple enlarged mediastinal and hilar lymph nodes with no parenchymal infiltrations [Figure 3]. A repeated excisional biopsy of one of the nodules from the right arm showed non-caseating discrete granulomata with minimal lymphocytic cuff without vasculitis or panniculitis [Figure 4]. Based on the clinical features and the results of the investigations, a diagnosis of sarcoidosis was made.
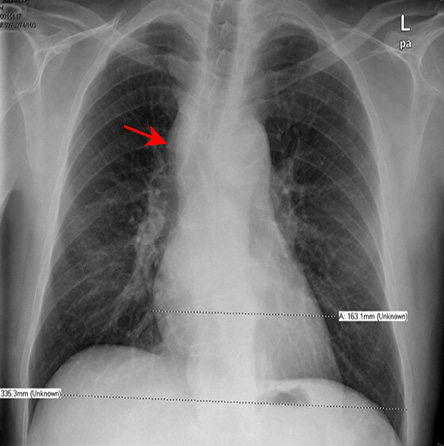
Figure 2: Chest X-ray showing superior mediastinal mass (red arrow).
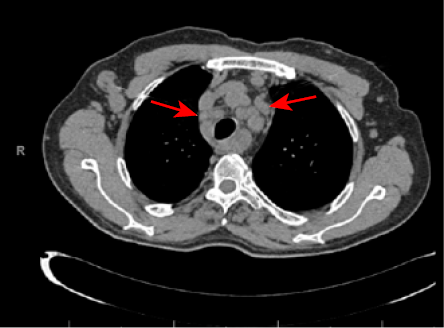
Figure 3: Axial computed tomography scan showing lymphadenopathy at the mediastinal area (red arrows) with clear lung parenchyma.
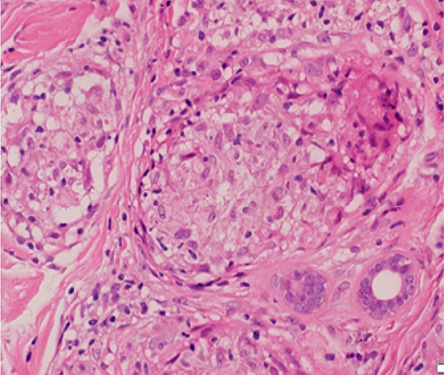
Figure 4: Histological section of right arm nodule showing a collection of epithelioid histiocytes surrounded by a thin cuff of lymphocytes, which composes non-caseating discrete granulomata. Magnification = 20 ×.
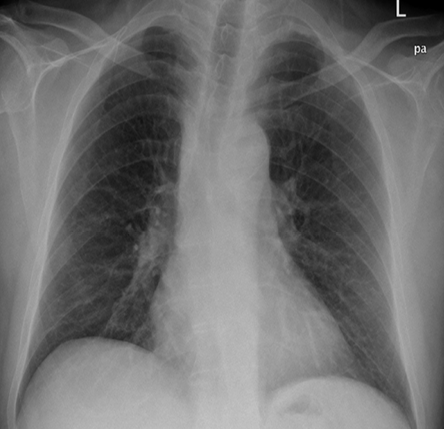
Figure 5: Chest X-ray showing regression of the superior mediastinal mass after treatment with steroid.
Given the patient’s acute kidney injury and hypercalcemia, he was admitted to the hospital for hydration and treatment with calcitonin, after which he improved, and his renal function tests became better. The patient was started on prednisolone 35 mg/day (0.4 mg/kg) and this was tapered down later once his clinical and biochemical parameters improved.
Upon follow-up after four weeks, he was asymptomatic. Serum calcium level and renal function tests had normalized. A repeat chest X-ray, which was done three months later, showed regression in the size of the mediastinal and hilar lymphadenopathy [Figure 5]. The dose of steroids was reduced gradually until a maintenance dose of 10 mg daily was reached. The patient has been seen regularly at the outpatient clinic and has been in good condition since.
Discussion
Sarcoidosis is a systemic disease of unknown etiology affecting multiple organs and is characterized by the presence of non-caseating granulomas.1 Although about 80% of cases affect people between the ages of 20 and 50, a second peak may occur in those between 50 and 65 years of age.1,11 Although sarcoidosis may affect anyone, it is more common in specific ethnic populations such as Swedes, Danes, and African-Caribbeans.1 Dry cough, shortness of breath, and chest pain are common clinical presentations and occur in almost 50% of cases.1 Constitutional symptoms such as fever, weight loss, and fatigue occur in one-third of patients.1 Lungs, lymphoid system, liver, and skin are often involved in sarcoidosis. The penis is rarely affected. Diagnosis is usually made based on the clinical presentation and radiological findings. However, the presence of non-caseating granuloma is typical and required to make the diagnosis.3 Other differential diagnoses such as tuberculosis, infections, and malignancies should be ruled out.
It is very rare for patients with sarcoidosis to present initially with a penile lesion only. A total of five similar case reports are published. The first was similar to our case report in which a patient presented with a six-month history of a penile mass and was diagnosed later with sarcoidosis based on the histopathological findings.6 The second reported a 29-year-old male who developed a penile lesion five years after being diagnosed with sarcoidosis.7 The third and fourth case reports were similar as they both reported patients with ulcerated penile lesions who responded well initially to steroids, but the penile lesions recurred. Both patients underwent partial penile amputation and one of them required ablation by radiotherapy because of recurrence at the scar site.8,9 The fifth case report involved a 53-year-old patient who presented initially with tender and erythematous swelling along with multiple yellowish subcutaneous nodules over the dorsal aspect of the glans penis and was diagnosed later with sarcoidosis.10
The first histopathology report of our patient showed features of granuloma annulare. This is a self-limiting and benign inflammatory skin lesion of unknown etiology.12 Although it is rare, penile granuloma annulare should have raised the clinician’s suspicion of chronic granulomatous disease given the suggestive clinical presentation of the patient.13 Our patient later developed widespread skin lesions over his chest and trunk. This is a much more common presentation of the disease and has been reported to occur in 25–35% of patients.14
Acute kidney injury has been reported as a rare and serious manifestation of the disease.15 The most common underlying pathology was tubulointerstitial nephropathy.15 Hypercalcemia occurs in 2–10% of patients with sarcoidosis and is due to dysregulation of calcium metabolism.3 The inflammatory process in sarcoidosis enhances the conversion of the inactive 25-hydroxyvitamin D to the active 1,25 dihydroxyvitamin D, which leads to increased absorption of calcium and thus the occurrence of hypercalcemia and/or hypercalciuria.14 Even though serum angiotensin-converting enzyme is raised in 75% of patients with sarcoidosis, it has low specificity.16 While the use of systemic corticosteroids in sarcoidosis remains controversial, certain features may necessitate its use. Hypercalcemia, cardiac, and neurological involvement are considered clear indications for therapy with steroids.1
In terms of prognosis, nearly two-thirds of patients with sarcoidosis will experience spontaneous remission while 10–30% may progress to a chronic and progressive stage of the disease.1
Conclusion
Because of the multi-system involvement of sarcoidosis, it can present in many different ways. Clinicians should consider sarcoidosis as one of the possible differential diagnosis whenever they encounter a patient with a suspicious penile lesion. Sarcoidosis should be considered a possibility even if histopathology showed only granuloma annulare in the presence of suggestive clinical features. Steroids, when indicated, are the mainstay of treatment for this clinical condition.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Newman LS, Rose CS, Maier LA. Sarcoidosis. N Engl J Med 1997 Apr;336(17):1224-1234.
- 2. Nunes H, Bouvry D, Soler P, Valeyre D. Sarcoidosis. Orphanet J Rare Dis 2007 Nov;2:46.
- 3. Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med 1999 Aug;160(2):736-755.
- 4. Ryan DM, Lesser BA, Crumley LA, Cartwright HA, Peron S, Haas GP, et al. Epididymal sarcoidosis. J Urol 1993 Jan;149(1):134-136.
- 5. Hausfeld KF. Primary sarcoidosis of the scrotum: case report. J Urol 1961 Aug;86:269-272.
- 6. Semiz H, Kobak S. Sarcoidosis presenting as penile mass. Lung India 2017 May-Jun;34(3):275-277.
- 7. Vitenson JH, Wilson JM. Sarcoid of the glans penis. J Urol 1972 Aug;108(2):284-289.
- 8. Whittaker M, Anderson CK, Clark PB. Sarcoidosis of the penis treated by radiotherapy. Br J Urol 1975 Jun;47(3):325-330.
- 9. Mahmood N, Afzal N, Joyce A. Sarcoidosis of the penis. Br J Urol 1997 Jul;80(1):155.
- 10. Rubinstein I, Baum GL, Hiss Y. Sarcoidosis of the penis: report of a case. J Urol 1986 May;135(5):1016-1017.
- 11. Baughman RP, Teirstein AS, Judson MA, Rossman MD, Yeager H Jr, Bresnitz EA, et al; Case Control Etiologic Study of Sarcoidosis (ACCESS) research group. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med 2001 Nov;164(10 Pt 1):1885-1889.
- 12. Barron DF, Cootauco MH, Cohen BA. Granuloma annulare. A clinical review. Lippincotts Prim Care Pract 1997 Mar-Apr;1(1):33-39.
- 13. Chopra A, Mitra D, Sharma L, Agarwal R. Granuloma annulare skin lesions in a case of sarcoidosis. Indian Dermatol Online J 2018 Mar-Apr;9(2):117-119.
- 14. Iannuzzi MC, Rybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med 2007 Nov;357(21):2153-2165.
- 15. Mahfoudhi M, Mamlouk H, Turki S, Kheder A. Systemic sarcoidosis complicated of acute renal failure: about 12 cases. Pan Afr Med J 2015 Sep;22:75.
- 16. Soto-Gomez N, Peters JI, Nambiar AM. Diagnosis and management of sarcoidosis. Am Fam Physician 2016 May;93(10):840-848.