Nasal lobular capillary hemangiomas (LCHs) are rare,1 rapidly growing hypervascular benign lesions whose exact etiopathogenesis is unknown. The most common location is the head and neck region. It has been reported that 76.9% of cases seen in children occur in this region with the gingiva, lips, and tongue being the most common sites and the nasal cavity as a less frequent location (15–20%).2 LCHs bleed easily with little manipulation or digital trauma due to excessive vascularity. Nasal LCHs arise mainly from the soft tissues of the nasal cavity and are often located (80%) on the anterior portion of the nasal septum (Little’s area) and less frequently on the anterior aspect of the inferior turbinate.1–4
Here, we describe an unusual case of a child presenting with unilateral severe nasal bleeding that proved to be a lobular hemangioma lesion arising from the posterior portion of the inferior turbinate. The patient underwent complete excision using an endonasal endoscopic approach.
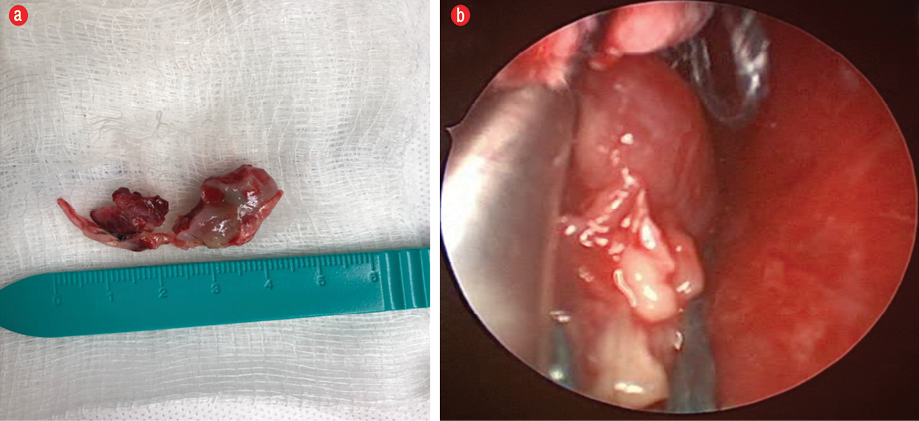
Figure 1: (a) Complete excision and division of the nasal vascular mass after piecemeal excision endoscopically. (b) Endoscopic view of vascular fleshy mass in the right nasal cavity attached to the inferior turbinate wall.
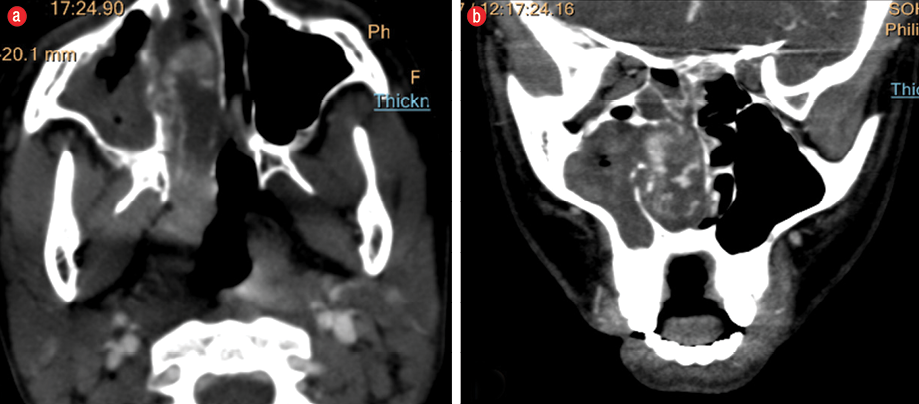
Figure 2: Contrast-enhanced computed tomography of paranasal sinuses and nasopharynx. (a) Axial and (b) coronal images of arterial phase showed a large soft tissue mass filling the right nasal cavity, with peripheral enhancement, more prominent at the side of the right inferior turbinate and with thin linear enhanced vessels within the mass. Note the intact sphenopalatine foramen and pterygopalatine fossa.
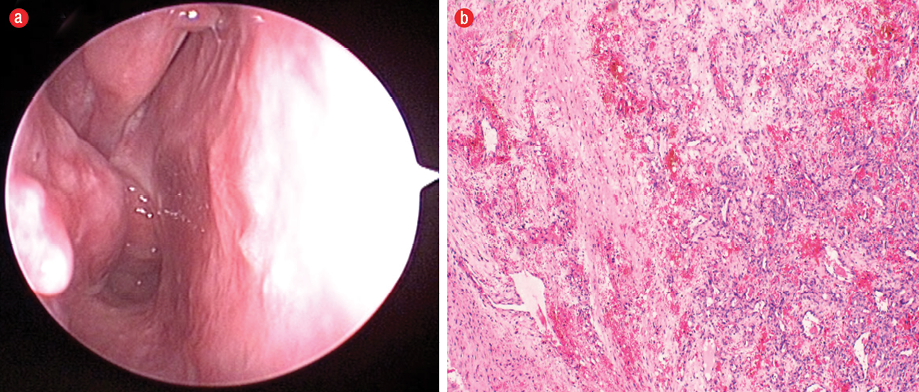
Figure 3: (a) Six-month postoperative endoscopic view of the right nasal cavity shows no recurrence. (b) Microscopic view of lobular hemangioma composed of small capillaries lined with endothelial cells (hematoxylin and eosin stain, magnification = 20 ×).
Case report
A 12-year-old girl presented to the emergency room with severe epistaxis from the right nasal cavity. The nasal bleed was controlled after insertion of an anterior nasal pack. She had a history of recurrent epistaxis over the previous two months, the most recent being three days before her presentation; each episode lasted for 15–20 minutes as the bleeding stopped spontaneously after applying pressure to the nose. She denied any history of nasal trauma or nasal surgery, and there was no history of prolonged bleeding. After 24 hours, the anterior nasal pack was removed and nasal endoscopic evaluation revealed a fragile, pink colored mass occupying the right nasal cavity [Figure 1a], which bled on touch.
Subsequent contrast-enhanced computed tomography (CT) showed a large soft tissue mass filling the right nasal cavity and extending to the nasopharynx [Figure 2].
Consent for endoscopic excision of the mass was received from her parents after the anesthetist evaluated her condition. Owing to the low hemoglobin level of the child on arrival at the hospital (8.61 g/dL), she was transfused with one unit of blood before surgery and one unit during surgery.
The procedure was carried out under general anesthesia using the four-hand technique (i.e., two surgeons working together with four hands in same nostril) under endoscopic control. It started with a detailed examination of the mass and relevant nasal anatomy. Then cautery was used to coagulate the tissues before debulking and dissecting the mass out in piecemeal fashion until reaching the feeding vessel. This was followed by cauterization of the stump of the inferior turbinate and control of the associated branch of the sphenopalatine artery. A nasal pack was inserted [Figure 1b].
The pieces of the lesion (4.5 × 1.6 cm) were collected together and sent to histopathology for analysis. It was subsequently reported as lobular hemangioma. In the first postoperative day, the nasal pack was removed, and the patient was kept under observation for a few days before being discharged home. She was followed-up in the clinic at one, three, nine, and 11 months postoperatively with no evidence of local recurrence [Figure 3].
Discussion
LCH or pyogenic granuloma is a benign rapidly growing vascular lesion that is rarely found on the surface mucosa of the nasal cavity. It was first described as pyogenic granuloma in 1940 but renamed lobular capillary hemangioma in 1980 owing to its microscopic features.5 There are different types of lobular hemangioma: capillary, cavernous, and mixed hemangioma. The pathophysiology of LCH is unknown, but it is associated with trauma, pregnancy, oral contraceptive use, and several cases have been reported as a result of excessive bipolar cautery used in inferior turbinate surgery.6,7 During puberty, the gestational hormones can lead to rapid growth of the lesion and with increased symptoms, as in our case; however, hemangiomas are often confused with more aggressive lesions such as angiofibroma and hemangiopericytomas, which are more common in young boys and in pregnancy, respectively. The typical presentation of LCHs is as intermittent, painless unilateral epistaxis. On clinical examination, the mass appears as a fleshy, vascular lesion that is often ulcerated and friable with gentle touching.
Imaging studies are frequently used to diagnose an intranasal mass that shows contrast enhancement and to determine the extent of the lesion, as well as to rule out other vascular neoplasms. Both CT with intravenous contrast and magnetic resonance imaging (MRI) (hyperintense lesion on T1- and T2-weighted images) can also identify typical features of the various histologic subtypes of hemangioma such as soap bubble or honeycomb patterns seen in cavernous hemangiomas.1,8
In our case, contrast-enhanced CT images in the venous phase were consistent with those reported in a previous study, which found that the central intense enhancing portion of the mass correlated histologically with the lobular area, and the iso- or hypoattenuating cap of variable thickness might correspond to the superficial ulcerative area.9 In children, congenital malformations such as meningoceles, dermoid cysts, angiomatous polyps, schwannomas, angiofibromas, and gliomas should be considered in the differential diagnosis of an intranasal mass and can be differentiated by CT or MRI.10,11 Apart from hemangioma, none of these lesions has a central enhanced lobular part with a hypoattenuating cap.8
The location of intranasal LCH is variable.2 In another case report, the hemangioma was attached to the lateral nasal wall whereas in our case the lesion was found attached to the posterior end of the inferior turbinate.12 This is interesting as it proved to be a rare location for such a lesion.
The treatment of intranasal hemangioma is complete surgical excision. We performed transnasal endoscopic resection of the large hemangioma arising from the inferior turbinate branch of the sphenopalatine artery in this 12-year-old girl after her presentation to the emergency room with epistaxis. The important steps in surgical excision are: (1) understanding the anatomy of the sinus and pterygopalatine fossa; (2) using the four-hand technique to clear the surgical field and facilitate the excision; and (3) using instruments such as a microdebrider and electrocautery to debulk the mass and control the feeding pedicle under endoscopic view. In our case, follow-up for 11 months revealed that the patient was asymptomatic with no signs of recurrence or complications.
Conclusion
Intranasal LCH is a rare diagnosis and can be a life-threatening condition in children when accompanied by severe epistaxis. Therefore, an otolaryngologist or emergency physician must be highly vigilant to diagnose and manage these cases. Endonasal endoscopic excision is an effective treatment option with low surgical morbidity and favorable long-term outcome.
Disclosure
The authors declared no conflict of interest.
references
- 1. Ozcan C, Apa DD, Görür K. Pediatric lobular capillary hemangioma of the nasal cavity. Eur Arch Otorhinolaryngol 2004 Sep;261(8):449-451.
- 2. Pagliai KA, Cohen BA. Pyogenic granuloma in children. Pediatr Dermatol 2004 Jan-Feb;21(1):10-13.
- 3. Jones JE, Nguyen A, Tabaee A. Pyogenic granuloma (pregnancy tumor) of the nasal cavity. A case report. J Reprod Med 2000 Sep;45(9):749-753.
- 4. Miller FR, D’Agostino MA, Schlack K. Lobular capillary hemangioma of the nasal cavity. Otolaryngol Head Neck Surg 1999 May;120(5):783-784.
- 5. Mills SE, Cooper PH, Fechner RE. Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol 1980 Oct;4(5):470-479.
- 6. Gregorio LL, Wu CL, Busaba NY. Lobular capillary hemangioma formation: an unusual complication of submucous resection with power instrumentation of the inferior turbinate. Laryngoscope 2015 Dec;125(12):2653-2655.
- 7. Shirazi N, Bist SS, Selvi TN, Harsh M. Spectrum of sinonasal tumors: a 10-year experience at a tertiary care hospital in north India. Oman Med J 2015;30(6):435-440.
- 8. Puxeddu R, Berlucchi M, Ledda GP, Parodo G, Farina D, Nicolai P. Lobular capillary hemangioma of the nasal cavity: a retrospective study on 40 patients. Am J Rhinol 2006 Jul-Aug;20(4):480-484.
- 9. Lee DG, Lee SK, Chang HW, Kim JY, Lee HJ, Lee SM, et al. CT features of lobular capillary hemangioma of the nasal cavity. AJNR Am J Neuroradiol 2010 Apr;31(4):749-754.
- 10. Katori H, Tsukuda M. Lobular capillary hemangioma of the nasal cavity in child. Auris Nasus Larynx 2005 Jun;32(2):185-188.
- 11. Karagama YG, Howarth K, Steel PR, Spencer MG. Lobular capillary haemangioma of the nasal vestibule: a rare entity. Int J Pediatr Otorhinolaryngol 2002 Oct;66(1):71-75.
- 12. Ahmad R, Norie A. Endonasal endoscopic resection of intranasal haemangioma. Med J Malaysia 2006 Dec;61(5):644-646.