|
Introduction
Ovarian adenofibromas are characterized histologically by a prominent fibrous tissue component in addition to epithelial elements. They are classified by the World Health Organization according to epithelial type into serous, endometrioid, mucinous, clear cell and mixed categories and according to the degree of epithelial proliferation and atypia into benign, borderline and malignant variants. The epithelium is usually of the serous type. Tumors with epithelium composed of hobnail, cuboidal or columnar cells with abundant clear or eosinophilic cytoplasm were classified as clear cell. Clear cell adenofibromas are distinctly unusual. Compared to clear cell carcinomas, borderline clear cell tumors are rather rare.1-8 In the present report, we describe a rare case of primary ovarian clear cell adenofibroma of borderline malignancy.
Case Report
A 53-year-old woman (para 6+2) was admitted to our hospital on account of a 3 years history of irregular vaginal bleeding, abdominal pain and fullness. She was 5 years postmenopausal. A left adnexal mass was palpated by the physical examination. Ultrasonography and magnetic resonance imaging showed solid, left adnexal mass measuring 91X56 mm (figure 1). The blood count and blood chemistry were normal. Tumor markers; CA125, CA19-9 and CEA were not elevated. Cervicovaginal cytologic analysis revealed no malignant cells. The clinical suspicion was that of an ovarian malignancy. Laparotomy showed a left ovarian mass with smooth surface and intact capsule. There were no ascite, peritoneal or omental tumor implant at exploration. Evaluation of the frozen histopathologic section of the ovarian mass was consistent with adenofibroma. Total abdominal hysterectomy and bilateral salpingo-oophorectomy were performed.
Macroscopic examination showed that the uterus and the endometrium was normal in size. The left ovary, weighing 35 g, measured 12X10.5X6.5 cm and consisted of well-demarcated solid multinodular mass. The cut surface was firm, homogeneous, yellowish-white (Figure 2). The right ovary was atrophic.
Microscopically, the tumor consisted mainly of fibrous stroma and widely spaced simple glands that were lined by cuboidal cells with eosinophilic or clear cytoplasm (figure 3). Most of the glands composed of a single layer of flattened or cuboidal cells with uniform nuclei. But a few glands, lined by one to three layers of cuboidal cells, with mild to moderate pleomorphic, hyperchromatic nuclei and mitotic figures were observed (figure 4). Some of the glands were cystically dilated and filled with eosinophilic secretion (figure 3).
Histochemically, these luminal secretions were mucicarmine positive but there was no cytoplasmic staining of mucicarmine. The stromal component consisted of short, interlacing fascicles of spindle-shaped cells. There was no component of sex cord stromal tumor or luteinized cells. There was no significant pathologic finding in the endometrium, myometrium and contralateral ovary. The histopathologic diagnosis was borderline clear cell adenofibroma. The patient is alive and well without signs of recurrence 6 months after the operation.
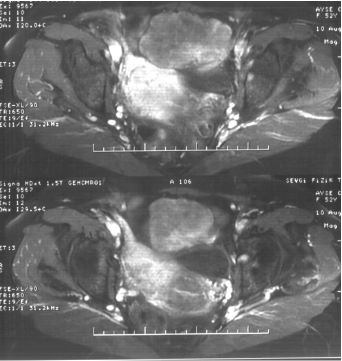
Figure 1: Magnetic resonance imaging shows solid, left adnexal mass.
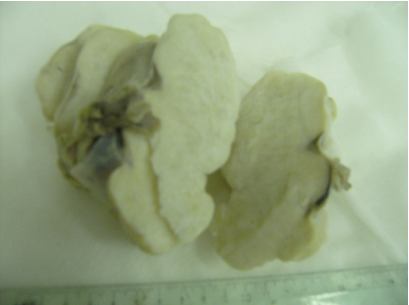
Figure 2: The left ovary measured 12X10.5X6.5 cm and consisted of well-demarcated solid multinodular mass.
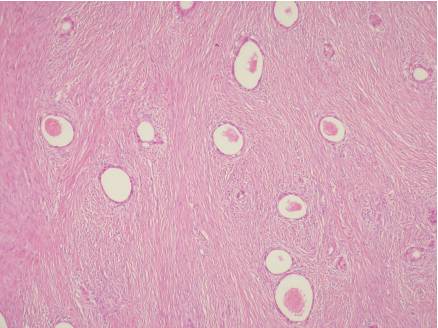
Figure 3: The tumor consisted of fibrous stroma and widely spaced simple glands that were lined by cuboidal cells with eosinophilic or clear cytoplasm (H&E, X40).
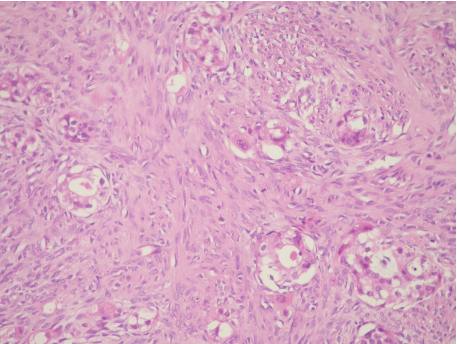
Figure 4: The tumor focally showed glands lined by one to three layers of cuboidal cells with mild to moderate pleomorphic, hyperchromatic nuclei (H&E, X200).
Discussion
Ovarian adenofibromas are subclassified according to the degrees of cytologic and architectural atypicality of the epithelial component and the presence or absence of stromal invasion into some groups. Tumors composed of simple glands lined by one to two layers of epithelium that showed no significant atypia were classified as benign. Tumors that contained glands or small solid nests composed of cells with nuclear characteristics of low-grade malignancy without invasion of the stroma were designated as borderline.1,2 In the present case, the epithelium lining the glands showed stratification; two to three cell layers in some areas. The cells exhibited focally mild to moderate nuclear atypia so the diagnosis was adenofibroma of borderline malignancy.
Clear cell adenofibroma has been suggested as a precursor for clear cell adenocarcinoma. Yamamoto et al determined that loss of heterozygosities on 5p, 10q and 22q were frequently present in both clear cell adenofibroma and clear cell adenocarcinoma. They also demonstrated that clear cell adenofibromatous components especially borderline type have been coexisted in ovarian clear cell adenocarcinomas.3-5 Veras et al divided clear cell carcinomas into cystic and adenofibromatous groups and discovered that the adenofibromatous group was often diagnosed in more advanced stage, showed less frequency with endometriosis and a less favorable outcome.6 But Yamamoto et al observed that clear cell adenocarcinomas associated with adenofibromatous areas were more likely to be low grade and had a more favorable prognosis.3 Recently a study of Zhao et al proposed that endometriosis is the underlying precursor for both the cystic and the adenofibromatous types of clear cell carcinoma.7 All the evidence implies that there are two different pathogenetic pathways of ovarian clear cell adenocarcinomas; endometriosis associated and adenofibroma-associated pathway.3-7 In the present case there was no associated endometriosis or foci of clear cell carcinoma.
Since clear cell carcinoma sometimes is accompained by benign and borderline adenofibromas, extensive sampling of any adenofibroma is essential to exclude areas of carcinoma. Identification of the foci of stromal invasion can be difficult. Small solid masses of clear cells in the stroma raise the question of invasion. Bell et al proposed some criteria for invasion like the presence of glands, small solid nests of malignant cells, or single malignant cells extending irregularly into the stroma and the presence of a desmoplastic, myxoid or edematous stromal reaction.1 Occasionally minute foci of invasion can be identified and these tumors are designated ‘microinvasive’.2 In the present case, tumor focally showed glands lined by one to three layers of cuboidal cells with mild to moderate pleomorphic, hyperchromatic nuclei. But we did not observe any evidence of stromal invasion. When nuclear atypia is more marked with coarse chromatin clumping, prominent nucleoli and increased mitotic activity then the tumor is best designated as ‘borderline clear cell adenofibromas with intraepithelial carcinoma’.1,2
The largest series of borderline clear cell adenofibroma was reported by Bell et al. In their series with 11 patients, the mean age was 61 years, tumors ranged in diameter from 6.5 to 23 cm (mean 14 cm) and the presenting complaints of the women were non-specific; irregular vaginal bleeding, abdominal fullness and pelvic pain. 10 of 11 tumors were unilateral.1 The clinical features of the present case; a 53 years old woman complaining of irregular vaginal bleeding, abdominal tenderness and unilateral ovarian mass, are consistent with the literature findings.
Borderline adenofibromatous tumors including those with intraepithelial carcinoma and microinvasion have a benign course following removal of the ovary. Bell et al reported only one patient who had a questionable lung metastasis 4 years after presentation and another patient with microinvasive tumor had a pelvic recurrence 3.3 years postoperatively.1,2 The present case has no signs of recurrence 6 months after the operation.
Conclusion
Clear cell adenofibromas of borderline malignancy are extremely rare tumors. The clinicopathologic and prognostic features are limited. Because of common association with typical clear cell carcinomas, extensive sampling is advised. Identification of the foci of microinvasion is also important to alert the clinician for long-term follow-up
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Bell DA, Scully RE. Benign and borderline clear cell adenofibromas of the ovary. Cancer 1985 Dec;56(12):2922-2931.
2. Tavassoli FA, Devilee P, eds. World Health Organization classification of tumours. In Pathology and Genetics of Tumours of the Breast and Female Genital Organs. IARC Press: Lyon, 2003; 218- 228.
3. Yamamoto S, Tsuda H, Takano M, Hase K, Tamai S, Matsubara O. Clear-cell adenofibroma can be a clonal precursor for clear-cell adenocarcinoma of the ovary: a possible alternative ovarian clear-cell carcinogenic pathway. J Pathol 2008 Sep;216(1):103-110.
4. Yamamoto S, Tsuda H, Yoshikawa T, Kudoh K, Kita T, Furuya K, et al. Clear cell adenocarcinoma associated with clear cell adenofibromatous components: a subgroup of ovarian clear cell adenocarcinoma with distinct clinicopathological characteristics. Am J Surg Pathol 2007;93:798-806.
5. Liu JL, Chu PY, Yeh KT, Huang RH. Borderline clear cell adenofibroma with extensive hemorrhagic necrosis. Hematol Oncol Stem Cell Ther 2010;3(3):158-160.
6. Veras E, Mao TL, Ayhan A, Ueda S, Lai H, Hayran M, et al. Cystic and adenofibromatous clear cell carcinomas of the ovary: distinctive tumors that differ in their pathogenesis and behavior: a clinicopathologic analysis of 122 cases. Am J Surg Pathol 2009 Jun;33(6):844-853.
7. Zhao C, Wu LS, Barner R. Pathogenesis of ovarian clear cell adenofibroma, atypical proliferative (borderline) tumor, and carcinoma: clinicopathologic features of tumors with endometriosis or adenofibromatous components support two related pathways of tumor development. J Cancer 2011;2:94-106.
8. Sugiyama T, Nishida T, Kataoka A, Okura N, Iwanaga S, Yakushiji M. A pregnant woman with clear cell adenocarcinoma of the ovary arising from endometriosis and with benign and borderline adenofibroma of the clear cell and endometrioid types. Eur J Obstet Gynecol Reprod Biol 1997 Mar;72(1):47-50.
|