Leiomyoma of the uterus is a common smooth muscle tumor in 20−30% of premenopausal women.1 However, an infected leiomyoma containing pus (termed a pyomyoma) is extremely rare and has high morbidity and mortality.2 About 100 cases of pyomyoma have been reported worldwide of which only 19 cases were reported after 1945.3,4
Case Report
A 26-year-old woman with a uterine leiomyoma was referred to our hospital six weeks after a spontaneous abortion with persistent fever. She gave a history of dysmenorrhea and menorrhagia. Magnetic resonance imaging (MRI) performed two years prior showed a large posterior wall leiomyoma (11 × 7 cm). Her first pregnancy ended in intrauterine fetal death at 20 weeks gestation followed one day later by spontaneous abortion. She experienced excessive bleeding after the abortion, which was controlled with curettage. Subsequently, she developed fever with chills ranging from 38−39 ºC, which persisted to date. There was no history of fever or ruptured membranes prior to abortion.
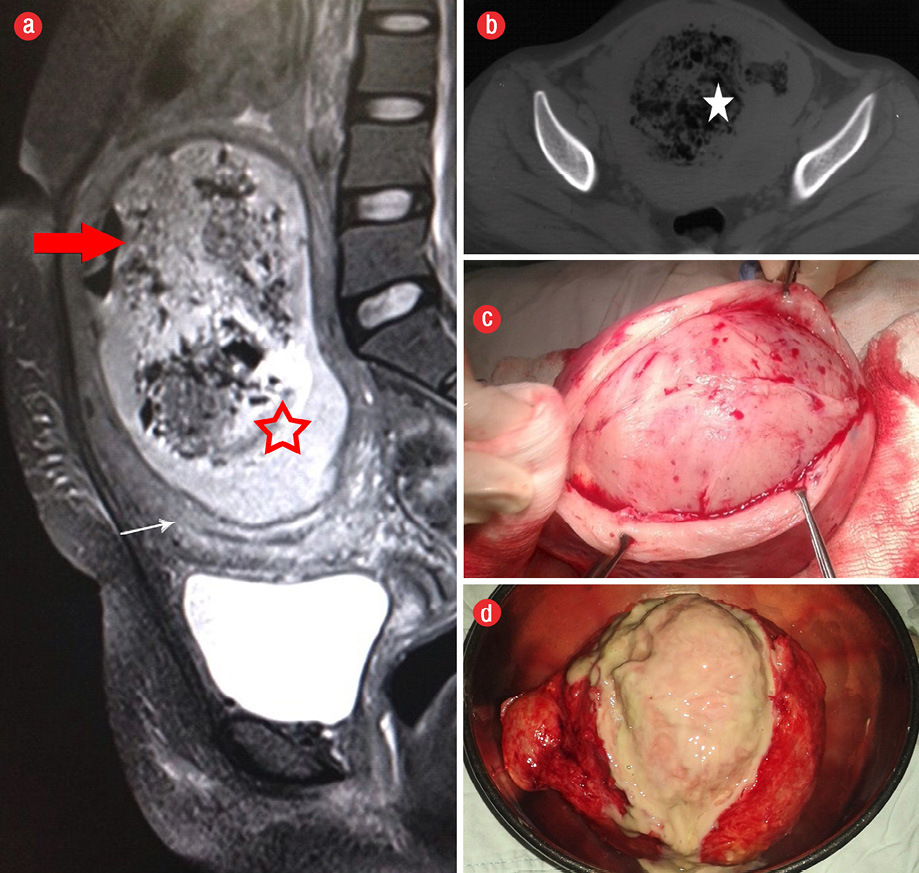
Figure 1: (a) T2-weighted sagittal magnetic resonance image showing ovoid heterogeneously hyper intense lesion (star) in the posterior wall of uterus with air-fluid level (red arrow) in the nondependent part. Endometrium was compressed anteriorly (white arrow). (b) Axial noncontrast computed tomography showing mottled air lucencies in uterus suggestive of collection (star). (c) Pyomyoma after incising the myometrium. (d) Cut section of pyomyoma with purulent content.
In her initial septic work up, she had anemia with hemoglobin (Hb) levels of 7 g/dL and polymorphonuclear leukocytosis (total leukocyte count (TLC) 18 000−24 000/m3, polymorphs 85%), but her blood and urine cultures were sterile. Widal test was negative. She received intravenous antibiotics (ceftriaxone, amikacin, and metronidazole). An ultrasound performed one week later showed a submucosal leiomyoma (15 × 15 cm) with echogenic foci along with pyometra; this was drained by cervical dilatation. She was admitted to the hospital and received antibiotics for four weeks (piperacillin with tazobactum, vancomycin, and meropenem). Thereafter, she was admitted to another hospital for two weeks. Her Hb was 6.4 g/dL for which she received three units of blood. Intravenous antibiotics (imipenem and clindamycin) were administered based on vaginal swab culture showing Escherichia coli. Sagittal T2-weighted MRI showed a large ovoid heterogeneously hyperintense lesion on the posterior wall of the uterus with air fluid level in nondependent part. The endometrium was compressed anteriorly [Figure 1a]. As her MRI two years prior showed a large leiomyoma, the present features were suggestive of degeneration with abscess formation.
On admission to our hospital, she was febrile (38 ºC). Her chest and cardiovascular systems were normal. The uterus was tender, enlarged to 24 weeks size and there was no hepatosplenomegaly. There was no vaginal discharge. Her Hb was 8.3 g/dL, TLC was 12 500/mm3, and renal and liver function tests were normal. Her blood, urine, and cervical swab cultures were sterile. A computed tomography (CT) scan (axial section) showed mottled air lucencies in the uterus suggestive of collection or necrosis with infection in the existing leiomyoma [Figure 1b]. She underwent laparotomy and myomectomy. Both tubes and ovaries were normal. On cutting open the leiomyoma, foul smelling pus was present [Figure 1c and d]. She became afebrile one day after myomectomy. The pus culture from the pyomyoma was sterile. Antibiotics were stopped on the fifth postoperative day, and she was discharged. Histopathology showed leiomyoma with inflammation.
Discussion
A pyomyoma develops due to infection in necrotic foci within a leiomyoma.2 Necrotic foci in a leiomyoma are more common during pregnancy due to rapid growth and hemorrhage, and in postmenopausal women secondary to vascular insufficiency.2 In the postpartum and postabortal period, ascending infection may result in a pyomyoma.2,5 Other factors which contribute are curettage, gynecological surgery, cervical stenosis, or immunodeficiency.6 The incidence of pyomyoma has increased in recent years due to uterine artery embolisation.7,8 A leiomyoma may get infected by direct spread from the adjacent endometrial cavity, bowel or adnexa, and by hematogenous or lymphatic spread.2 Kaler et al9 reported a case of postpartum pyomyoma in a patient with preterm premature rupture of membranes, chorioamnionitis, and postpartum hemorrhage managed with intrauterine balloon tamponade.
A typical triad of its clinical features is sepsis, leiomyoma, and absence of any other source of infection.10 The infection is usually polymicrobial.6 The common organisms include Staphylococcus aureus, Streptococcus haemolyticus, Proteus, Streptococcus agalactiae, E. coli, Enterococcus faecalis, and Sphingomonas paucimobilis.2,6 E. coli were cultured in a vaginal swab in this patient. The most common symptom is fever.6 In a review, fever was observed in 84% and abdominal pain in 57% of patients.4 Differential diagnoses to be considered include: pyometra, tubo-ovarian abscess, red degeneration of leiomyoma, or septic abortion.2
Sonographic features include a heterogeneous mass with echogenic foci suggestive of air.2 Presence of air on CT scan is a characteristic of pyomyoma or gossypiboma.2,10 As there was no prior history of laparotomy or intrauterine packing following abortion, gossypiboma was not considered. On MRI, we observed a large ovoid heterogeneously hyperintense lesion in the posterior wall of the uterus with air fluid level in nondependent part, which were interpreted to be a leiomyoma with degeneration or abscess formation. A subsequent CT with mottled air lucencies in the uterus was also suggestive of pus collection in the leiomyoma resulting in a pyomyoma.
A serious complication of a pyomyoma is its spontaneous rupture, which presents as an acute abdomen with septicemic shock.4 Discontinuity of the wall of a leiomyoma along with the presence of intraperitoneal air plus free fluid is suggestive of rupture of a pyomyoma.11 In our patient, abortion followed by curettage and a submucosal location contributed to the development of a pyomyoma. The mortality associated with a pyomyoma varies from 21−30%, hence, early diagnosis is important to manage this potentially life-threatening condition.2 The definitive treatment is hysterectomy or myomectomy if fertility is desired along with antibiotics.2 De Maio et al12 reported a case where pyomyoma was removed vaginally thereby avoiding major abdominal surgery. CT guided drainage of pyomyoma related to pregnancy has also shown success as a minimally invasive option, hence preserving fertility.13,14
Conclusion
Our patient presented with postabortal fever secondary to pyomyoma (i.e., infection in the leiomyoma). Sonographic features of pyomyoma include a heterogeneous mass with echogenic foci suggestive of air. The presence of air on CT scan is a characteristic of pyomyoma. Early diagnosis is important to manage this potentially life-threatening condition. Surgical treatment is the management of choice. Gynecologists should consider the diagnosis of pyomyoma in women with a leiomyoma and sepsis in the absence of any apparent source of infection.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Al-Wadaani HA. Anterior abdominal wall leiomyoma arising de novo in a perimenopausal woman. Oman Med J 2012 Jul;27(4):323-325.
- 2. Gupta A, Gupta MM, Manaktala U. Ascending infection causing pyomyoma in a young woman. The Egyptian Journal of Radiology and Nuclear Medicine 2014;45:1017-1020.
- 3. Mubarak MY, Noordini MD. A case report of pyomyoma radiological diagnosis of a potentially fatal complication of uterine leiomyoma. Int Med J Malays 2008;7:63-65.
- 4. Yeat SK, Chong KM, Pan HS, Cheng WC, Hwang JL, Lee CC. Impending sepsis due to a ruptured pyomyoma with purulent peritonitis: a case report and literature review. Taiwan J Obstet Gynecol 2005;44:75-79.
- 5. Mason TC, Adair J, Lee YC. Postpartum pyomyoma. J Natl Med Assoc 2005 Jun;97(6):826-828.
- 6. Del Borgo C, Maneschi F, Belvisi V, Morelli F, Vetica A, Marocco R, et al. Postpartum fever in the presence of a fibroid: Sphingomonas paucimobilis sepsis associated with pyomyoma. BMC Infect Dis 2013 Dec;13:574.
- 7. Rosen ML, Anderson ML, Hawkins SM. Pyomyoma after uterine artery embolization. Obstet Gynecol 2013 Feb;121(2 Pt 2)(Suppl 1):431-433.
- 8. Shukla PA, Kumar A, Klyde D, Contractor S. Pyomyoma after uterine artery embolization. J Vasc Interv Radiol 2012 Mar;23(3):423-424.
- 9. Kaler M, Gailer R, Iskaros J, David AL. Postpartum Pyomyoma, a Rare Complication of Sepsis Associated with Chorioamnionitis and Massive Postpartum Haemorrhage Treated with an Intrauterine Balloon. Case Reports in Obstetrics and Gynecology 2015, Article ID 609205, 6 pages [cited 2015 July]. Available from: https://www.hindawi.com/journals/criog/2015/609205/.
- 10. Greenspoon JS, Ault M, James BA, Kaplan L. Pyomyoma associated with polymicrobial bacteremia and fatal septic shock: case report and review of the literature. Obstet Gynecol Surv 1990 Sep;45(9):563-569.
- 11. Karcaaltincaba M, Sudakoff GS. CT of a ruptured pyomyoma. AJR Am J Roentgenol 2003 Nov;181(5):1375-1377.
- 12. DeMaio A, Doyle M. Pyomyoma as a Rare Source of Postpartum Sepsis Case Reports in Obstetrics and Gynecology Volume 2015 (2015), Article ID 263518, 2 pages [cited 2015 July]. Available from: https://www.hindawi.com/journals/criog/2015/263518/.
- 13. Laubach M, Breugelmans M, Leyder M, Demey J, Foulon W. Nonsurgical treatment of pyomyoma in the postpartum period. Surg Infect 2011;2013: 65–68.
- 14. Adeoye TO, Abdul MA, Bawa US, MaduguN, AyanwuyiS, Umaru SH. Acute Gynaecological Abdomen Secondary to Pyomyoma: A Case Report.J Clin Case Rep 2015;5:595.