The number of people aged 60 years old or over is increasing worldwide. A World Health Organization (WHO) report projected that between 2000 to 2050, the proportion of the world’s population over 60 years will double from about 11% to 22%.1 Oman is no exception, with around 150 000 people ≥ 60 years of age accounting for 4% of the total population in 2013. Oman’s elderly population is expected to rise with the improvement in healthcare across the country.2 Elderly people usually suffer from multiple comorbidities and, as a result, become exposed to multiple drugs; this situation is often referred to as “polypharmacy.” Polypharmacy is a public health concern and is more serious in the elderly population since geriatric patients often suffer from altered pharmacokinetics, reduced drug clearance, and cognitive deficits.3 Moreover, polypharmacy is associated with a higher risk of adverse drug reactions and drug-drug interactions, subjecting patients to a greater number of adverse drug events and affecting their adherence levels.4–6 Polypharmacy in the elderly was shown to be a statistically significant predictor of hospitalization, nursing home placement, malnutrition, hypoglycemia, fractures, impaired mobility, pneumonia, and death.7 Furthermore, polypharmacy in the elderly is not only a health and safety concern, but it also results in additional costs to the healthcare system, accounting for more than one-third of prescription drugs.5
The definition of polypharmacy varies in the literature, but it ranges from the concurrent use of ≥ 2 to ≥ 5 prescription drugs.8–10 The prevalence of polypharmacy in the elderly has also varied, ranging from 21% in an Australian study11 to 86% in a Korean study.12 In the United States, the prevalence of polypharmacy in an elderly population quadrupled in 10 years.13 A study on the prevalence of polypharmacy in adult patients in a tertiary care hospital in Saudi Arabia reported a rate of 89%.14 Less research has been done on polypharmacy in hospitalized patients, but the studies that have addressed the issue reported high prevalence rates (74–90%).15–17
To our knowledge, no prior study in Oman has determined the prevalence of polypharmacy specifically in hospitalized elderly patients upon hospital discharge. The main objective of this study was to measure the prevalence of polypharmacy (for this investigation, defined as the concurrent use of ≥ 5 drugs) in relation to the covariates of comorbidity, gender, and age in patients aged ≥ 60 years on discharge from Sultan Qaboos University Hospital.
Methods
This cross-sectional study was conducted at Sultan Qaboos University Hospital between February and July 2014. All patients aged 60 years and above who were admitted to the medical wards for more than 24 hours and discharged on at least one medication were included. Patients admitted under teams other than medical specialties, those admitted for surgical procedures, and those discharged on no medication were excluded. Electronic medical notes were used to gather patients’ clinical and demographic information (including age, gender, admission diagnoses, number and types of comorbidities, length of stay, and the number and pharmacological class of the prescription drugs on discharge).
Descriptive statistics were used to describe the data. For categorical variables, frequencies and percentages were reported. The differences between groups were analyzed using Pearson’s chi-squared test or Fisher’s exact tests (for values < 5). For continuous variables, the mean and standard deviation (SD) or median and interquartile range (IQR) were used to summarize the data. A priori two-tailed level of significance was set at 0.050. The data were processed and analyzed using SPSS Statistics (SPSS Statistics Inc., Chicago, US) version 23.
Results
During the six-month study, a total of 431 patients met the inclusion criteria. Table 1 shows their demographic and clinical characteristics. The patient’s mean age was 72.0±8.3 years. Both genders were equally represented. Fifty-two percent of patients were between 60 and 70 years old, and 76.8% had more than one comorbidity. The prevalence of polypharmacy was 76.3% among all patients.
Cardiovascular disorders were the most common cause of admission during the study period (31.0%), followed by infections (23.0%). Renal disease accounted for only 3.2% of all admissions [Figure 1]. The median (IQR) of the number of medications prescribed at discharge was 7 (5, 9) with cardiovascular drugs accounting for the largest proportion (48.0%), followed by gastrointestinal drugs (11.0%) and medications acting on the endocrine system (9.2%) [Figure 2].
Age (adjusted odds ratio (aOR), 0.98; 95% CI 0.95, 1.00, p = 0.075) and gender (aOR, 1.17; 95% CI 0.73, 1.88, p = 0.502) were not associated with polypharmacy [Table 2]. However, polypharmacy was significantly associated with number of comorbidities (aOR, 1.31; 95% CI [1.12, 1.54],
p = 0.001) and having cardiovascular disease as an admitting diagnosis (aOR, 2.66; 95% CI 1.49, 4.75, p = 0.001).
The logistic model was statistically significant: LRχ2 (4) = 30.5; p < 0.001. The Hosmer–Lemeshow χ2 statistic (a measure of the goodness of fit) was 12.3, and the associated p-value was 0.140 denoting good model fit.
Table 1: Demographic and clinical characteristics of patients (N = 431).
|
Age, mean±SD, years |
72 ± 8.3 |
|
Age, n (%), years |
|
|
60–70 |
226 (52.4) |
|
71–80 |
139 (32.3) |
|
> 80 |
66 (15.3) |
|
Male, n (%) |
216 (50.1) |
|
Number of medications on discharge, median (IQR) |
7 (5, 9) |
|
≥ 5 medications |
329 (76.3) |
|
Number of comorbidities, median (IQR) |
3 (2, 4) |
|
Comorbidity > 1 |
331 (76.8) |
Percentages might not add up to 100 due to rounding off.
SD: standard deviation; IQR: interquartile range.
Table 2: Polypharmacy* in association with other covariates.
|
Age |
0.97 [0.94, 0.99] |
0.013 |
0.98 [0.95, 1.00] |
0.075 |
|
Gender |
1.12 [0.71, 1.73] |
0.631 |
1.17 [0.73, 1.88] |
0.502 |
|
Number of comorbidities |
1.35 [1.15, 1.58] |
< 0.001 |
1.31 [1.12, 1.54] |
0.001 |
*Defined as the use of ≥ 5 medications. Number of patients with polypharmacy = 329. OR: odds ratio; aOR: adjusted odds ratio; CI: confidence interval.
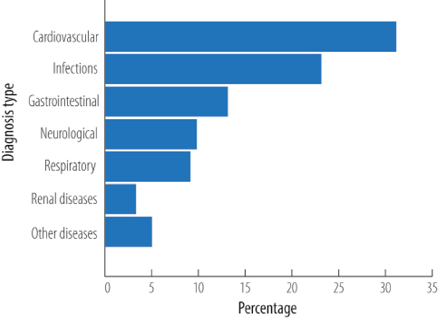
Figure 1: Diagnosis on admission.
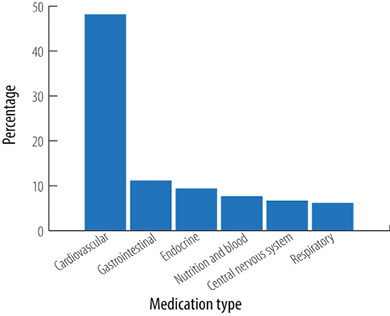
Figure 2: Pharmacological classes of medications prescribed on discharge based on the British National Formulary classification.
Discussion
Polypharmacy, defined for this study as the concurrent use of five or more drugs, was high in this cohort (76.3%). This high percentage can be attributed to the fact that the elderly group admitted to our hospital were expected to have multiple comorbidities and would probably be prescribed additional medications to their usual ones in order to treat an acute condition. Using the same definition for polypharmacy, Mexican researchers found a similar level of polypharmacy (84.5%) in a comparable cohort of elderly patients (> 70 years) hospitalized for cardiovascular disease.18 Other studies have shown a similarly high prevalence of polypharmacy, with 89% of patients in a tertiary care hospital in Abu Dhabi,19 76% in elderly inpatients in Australia,20 and 60% of patients admitted to hospital with rheumatic disease in Norway.21
There was no significant difference in the prevalence of polypharmacy between males and females in this study. Similarly, other studies have reported no impact of gender on polypharmacy.22,23 However, some studies have shown higher polypharmacy rates in females than males,10,13,24 while other studies have found the opposite.12,22 These discrepancies could be attributed to differences in physicians’ prescribing approaches according to gender, in addition to differences between males and females with respect to educational level and socioeconomic status in different settings.25
A significant association between age and polypharmacy was found using bivariate analysis, showing that age was inversely associated with polypharmacy rate: the older the patient, the lower the polypharmacy rate. However, adjustments for gender, comorbidity rate, and cardiovascular disease revealed no significant association. A study in Abu Dhabi19 similarly showed the rate of polypharmacy was less in the older age group (≥ 80 years). However, they did not adjust for confounding factors. According to other investigators, polypharmacy was higher with increasing age.8,10 The studied cohort had a high polypharmacy rate (76.3%) overall, and to show an effect of age on this high rate a larger sample might be needed. The rate of polypharmacy is nevertheless high in this elderly cohort, but this can be attributed to the increased morbidity associated with aging and the resulting tendency to be prescribed a greater number of medications.
Polypharmacy was indeed associated with an increase in comorbidities in our study as seen in other studies.19,20 This can be explained by the need for more medications to address multiple comorbidities. It can also be explained by looking at comorbidity as the result of polypharmacy, not only the cause of it. As described in some studies, medications can cause adverse drug events that may add to the load of illnesses from which elderly patients suffer. 25,26
Cardiovascular disease as a diagnosis on admission was found to be associated with polypharmacy. This is an expected finding, as clinical guidelines for the management of cardiovascular diseases advocate for the use of multiple medications.27 Polypharmacy within the context of cardiovascular illnesses may be justified if used following clinical guidelines, and may not necessarily be associated with adverse outcomes.28 However, the older and frailer the patient, the more susceptible they are to falls and fractures. Medications associated with drowsiness or blood pressure control may pose a higher risk for this group of elderly patients.23 Additionally, polypharmacy is naturally associated with taking more pills (pill burden), which may present an additional concern of lack of adherence, especially in the elderly.27
Cardiovascular diseases were the most commonly encountered condition on admission, followed by infections and gastrointestinal diseases; these findings are similar to those of other studies.24,29,30 This is expected, as the elderly are more likely to suffer from heart diseases, hypertension, and infections. As a result, drugs acting on the cardiovascular system were the most commonly prescribed, followed by gastrointestinal medications and medications acting on the endocrine system.
The strength of our study is that it reviewed polypharmacy in hospitalized elderly patients upon discharge, and not much work has been done in this category of patients. It is also the first study to examine the relationship between age, gender, comorbidity, and polypharmacy in elderly patients in Oman. The study had limitations due to its small sample size and the fact that there were no data on the number of pills the patient had to take every day, nor on any non-prescription drugs and supplements taken, as this information was not available in the medical records.
Conclusion
Our study revealed an alarmingly high rate of polypharmacy (76.3%) in an already frail, elderly group with multiple comorbidities. Gender and age did not have a significant impact on polypharmacy, but comorbidity and having a cardiovascular diagnosis on admission did. Efforts should be made to improve medication use and minimize inappropriate polypharmacy. Locally designed and delivered educational programs need to be implemented and can improve the awareness of prescribers and other healthcare providers. The contribution of clinical pharmacists is essential, as they have a key role in improving the appropriate use of medications. The impact of polypharmacy on medication adherence and other health outcomes was not investigated and needs to be addressed in future studies.
Disclosure
The authors declared no conflicts of interest. No funding was received for this work. The research was submitted and approved by Sultan Qaboos University, College of Medicine and Health Sciences Ethics Committee.
references
- 1. World Health Organization. Facts About Ageing 2014. [cited 2016 January 10]. Available at: http://www.who.int/ageing/about/facts/en/.
- 2. National Center for Statistics and Information. Statistical Year Book 2014. Ministry of National Economy. Muscat. 2014.
- 3. Dagli RJ, Sharma A. Polypharmacy: a global risk factor for elderly people. J Int Oral Health 2014 Nov-Dec;6(6):i-ii.
- 4. Ballentine NH. Polypharmacy in the elderly: maximizing benefit, minimizing harm. Crit Care Nurs Q 2008 Jan-Mar;31(1):40-45.
- 5. Fulton MM, Allen ER. Polypharmacy in the elderly: a literature review. J Am Acad Nurse Pract 2005 Apr;17(4):123-132.
- 6. Cooney D, Pascuzzi K. Polypharmacy in the elderly: focus on drug interactions and adherence in hypertension. Clin Geriatr Med 2009 May;25(2):221-233.
- 7. Frazier SC. Health outcomes and polypharmacy in elderly individuals: an integrated literature review. J Gerontol Nurs 2005 Sep;31(9):4-11.
- 8. Bjerrum L, Søgaard J, Hallas J, Kragstrup J. Polypharmacy: correlations with sex, age and drug regimen. A prescription database study. Eur J Clin Pharmacol 1998 May;54(3):197-202.
- 9. Bikowski RM, Ripsin CM, Lorraine VL. Physician-patient congruence regarding medication regimens. J Am Geriatr Soc 2001 Oct;49(10):1353-1357.
- 10. Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivelä SL, Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol 2002 Aug;55(8):809-817.
- 11. Haider SI, Ansari Z, Vaughan L, Matters H, Emerson E. Prevalence and factors associated with polypharmacy in Victorian adults with intellectual disability. Res Dev Disabil 2014 Nov;35(11):3071-3080.
- 12. Kim HA, Shin JY, Kim MH, Park BJ. Prevalence and predictors of polypharmacy among Korean elderly. PLoS One 2014;9(6):e98043. . Accessed 15 Jan 2016.
- 13. Aparasu RR, Mort JR, Brandt H. Polypharmacy trends in office visits by the elderly in the United States, 1990 and 2000. Res Social Adm Pharm 2005 Sep;1(3):446-459.
- 14. Salih SB, Yousuf M, Durihim H, Almodaimegh H, Tamim H. Prevalence and associated factors of polypharmacy among adult Saudi medical outpatients at a tertiary care center. J Family Community Med 2013 Sep;20(3):162-167.
- 15. Harugeri A, Joseph J, Parthasarathi G, Ramesh M, Guido S. Prescribing patterns and predictors of high-level polypharmacy in the elderly population: A prospective surveillance study from two teaching hospitals in India. Am J Geriatr Pharmacother 2010 Jun;8(3):271-280.
- 16. Mizokami F, Koide Y, Noro T, Furuta K. Polypharmacy with common diseases in hospitalized elderly patients. Am J Geriatr Pharmacother 2012 Apr;10(2):123-128.
- 17. Gamble JM, Hall JJ, Marrie TJ, Sadowski CA, Majumdar SR, Eurich DT. Medication transitions and polypharmacy in older adults following acute care. Ther Clin Risk Manag 2014;10:189-196.
- 18. Martínez-Arroyo JL, Gómez-García A, Sauceda-Martínez D. [Polypharmacy prevalence and potentially inappropriate drug prescription in the elderly hospitalized for cardiovascular disease]. Gac Med Mex 2014 Dec;150(Suppl 1):29-38.
- 19. Mubarak N. Makramalla E, Umniya A, Rao P. Prevalence of Poly-pharmacy in the Elderly: Implications of Age, Gender, Co-morbidities and Drug Interactions. SOJ Pharm Pharm Sci 2014;1(3):1-7.
- 20. Hubbard RE, Peel NM, Scott IA, Martin JH, Smith A, Pillans PI, et al. Polypharmacy among inpatients aged 70 years or older in Australia. Med J Aust 2015 Apr;202(7):373-377.
- 21. Viktil KK, Enstad M, Kutschera J, Smedstad LM, Schjøtt J. Polypharmacy among patients admitted to hospital with rheumatic diseases. Pharm World Sci 2001 Aug;23(4):153-158.
- 22. Jyrkkä J, Enlund H, Lavikainen P, Sulkava R, Hartikainen S. Association of polypharmacy with nutritional status, functional ability and cognitive capacity over a three-year period in an elderly population. Pharmacoepidemiol Drug Saf 2011 May;20(5):514-522.
- 23. Pan HH, Li CY, Chen TJ, Su TP, Wang KY. Association of polypharmacy with fall-related fractures in older Taiwanese people: age- and gender-specific analyses. BMJ Open 2014;4(3):e004428.
- 24. Ribeiro AQ, Rozenfeld S, Klein CH, César CC, Acurcio FdeA. [Survey on medicine use by elderly retirees in Belo Horizonte, Southeastern Brazil]. Rev Saude Publica 2008 Aug;42(4):724-732.
- 25. Bierman AS, Pugh MJ, Dhalla I, Amuan M, Fincke BG, Rosen A, et al. Sex differences in inappropriate prescribing among elderly veterans. Am J Geriatr Pharmacother 2007 Jun;5(2):147-161.
- 26. Blanco-Reina E, Ariza-Zafra G, Ocaña-Riola R, León-Ortíz M, Bellido-Estévez I. Optimizing elderly pharmacotherapy: polypharmacy vs. undertreatment. Are these two concepts related? Eur J Clin Pharmacol 2015 Feb;71(2):199-207.
- 27. Volpe M, Chin D, Paneni F. The challenge of polypharmacy in cardiovascular medicine. Fundam Clin Pharmacol 2010 Feb;24(1):9-17.
- 28. Appleton SC, Abel GA, Payne RA. Cardiovascular polypharmacy is not associated with unplanned hospitalisation: evidence from a retrospective cohort study. BMC Fam Pract 2014;15:58.
- 29. Wawruch M, Zikavska M, Wsolova L, Kuzelova M, Tisonova J, Gajdosik J, et al. Polypharmacy in elderly hospitalised patients in Slovakia. Pharm World Sci 2008 Jun;30(3):235-242.
- 30. Rozenfeld S. [Prevalence, associated factors, and misuse of medication in the elderly: a review]. Cad Saude Publica 2003 May-Jun;19(3):717-724.