Fibrosarcoma is a rare mesenchymal tumor with smooth-muscle differentiation. About 5–10% of fibrosarcomas arise in the head and neck, nose and paranasal sinuses, with skin and subcutaneous tissue being the prime location.1 Oral fibrosarcomas primarily involve the maxillary sinus and the maxillary or mandibular bone.
This malignant mesenchymal tumor of the fibroblasts rarely affects the oral cavity proper. The etiology of fibrosarcoma remains obscure, with many associated risk factors like radiation exposure, trauma, Paget’s disease of bone, fibrous dysplasia, and chronic osteomyelitis. Fibrosarcomas primarily occur in the soft tissues, but intraosseous lesions have also been reported.2 The clinical presentation of oral fibrosarcomas are pain, swelling, paraesthesia, loosening of the teeth and ulceration of the overlying mucosa. We present a rare case of gingival fibrosarcoma of the lower alveolar tissue in a 25-year-old female.
Case Report

Figure 1: Examination of the oral cavity revealed a nodular, well-defined, reddish, mobile lesion of 3.0 cm in diameter with normal overlying mucosa.
A 25-year-old woman presented with left molar mandibular gingival enlargement leading to difficulty in chewing. A nodular, well-defined reddish, mobile lesion of 3.0 cm in diameter, with normal overlying mucosa, was noted on local examination [Figure 1].
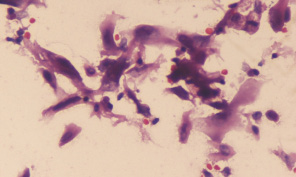
Figure 2: Fine-needle aspiration cytology of the mass showed a loosely cohesive population of spindle-shaped cells with oval hyperchromatic nuclei and pulled out cytoplasmic strands. Papanicolaou staining, magnification = 40 ×.
Aspiration cytology of the mass revealed loosely cohesive clusters of spindle-shaped cells with oval hyperchromatic nuclei and pulled out cytoplasmic strands [Figure 2].
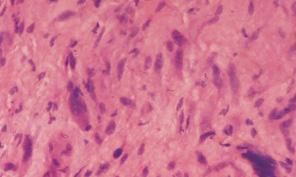
Figure 3: Microscopically, the tumor was composed of interlacing fascicles of spindle-shaped cells with elongated, blunt-ended nuclei and eosinophilic cytoplasm. Mitoses, both typical and atypical, and scattered necrotic foci were present. Hematoxylin and eosin staining, magnification = 40 ×.
The tumor was excised completely, formalin-fixed and paraffin embedded, and the sections examined. Microscopically, the tumor mass comprised of interlacing fascicles of spindle-shaped cells with oval to plump nuclei and moderate eosinophilic cytoplasm. Foci of necrosis with intense mitotic activity was also seen [Figure 3]. Vimentin showed diffuse cytoplasmic positivity in the tumor cells [Figure 4]. Adjuvant chemotherapy with six cycles of cisplatin (50 mg/m2) was administered. Our patient survived and there were no signs of recurrence of the disease after two years follow-up.
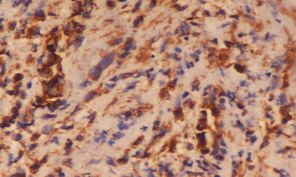
Figure 4: Diffuse cytoplasmic vimentin immunoreactivity was demonstrated in the tumor cells. Vimentin immunostaining, magnification = 40 ×.
Discussion
Fibrosarcoma is a rare mesenchymal malignant tumor and commonly occurs in the whole head and neck region, accounting for about 1% of all tumors in this region.1-4 Mandible is the prime foci of the intraosseous form of fibrosarcoma in the head and neck region.3 The overall ten-year survival of low and high-grade sarcoma of the bone is 83.0% and 34.0% respectively.5
The predominant age group for the occurrence of fibrosarcoma is between the second and sixth decades of life with equal gender predisposition.6
The typical presentation of the lesion is swelling, with associated pain and paraesthesia.1,3,7 Fibrosarcomas on radiologic imaging appear as radiolucent lesions with marked osteolysis and bone destruction, devoid of calcific or osseous areas.5,6 The absence of tumoral calcification or ossification helps to differentiate fibrosarcomas from other malignancies such as chondrosarcomas and osteosarcomas.8
The grade of fibrosarcomas from low to high, depend on the number of mitotic figures, tumor differentiation, and the presence of tumor necrosis.6,8,9 Low-grade tumors with complete surgical resection have a good prognosis.1,2,4 The need for adjuvant radiotherapy and/or chemotherapy is still unclear, but they are indicated in high-grade tumors so as to minimize microscopic metastases and recurrence.6,10
The need for prophylactic neck dissection is still controversial and not advocated in all cases.11,12 Our case was treated with surgical resection and reconstructive mandibular surgery followed by adjuvant chemotherapy.
Conclusion
Intraoral fibrosarcomas are an unusual finding. Accurate diagnosis and prompt treatment of the lesion is mandatory for prolonged disease-free survival, and to avoid tumor recurrence.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Petrone G, Perrotti V, Fioroni M, Rubini C, Piattelli A. Haemangiopericytoma of the maxillary gingiva: report of a case. J Clin Periodontol 2005 Aug; 32(8):921-924.
- 2. Lo Muzio L, Favia G, Farronato G, Piattelli A, Maiorano E. Primary gingival leiomyosarcoma. A clinicopathological study of 1 case with prolonged survival. J Clin Periodontol 2002 Feb; 29(2):182-187.
- 3. Pereira CM, Jorge J Jr, Di Hipólito O Jr, Kowalski LP, Lopes MA. Primary intraosseous fibrosarcoma of jaw. Int J Oral Maxillofac Surg 2005 Jul; 34(5):579-581.
- 4. Gosau M, Draenert FG, Winter WA, Mueller-Hoecker J, Driemel O. Fibrosarcoma of the childhood mandible. Head Face Med 2008; 4:21-25.
- 5. Soares AB, Lins LH, Macedo AP, Pereira-Neto JS, Vargas PA. Fibrosarcoma originating in the mandible. Med Oral Patol Oral Cir Bucal 2006 May; 11(3):E243-E246.
- 6. Leitner C, Hoffmann J, Kröber S, Reinert S. Low-grade malignant fibrosarcoma of the dental follicle of an unerupted third molar without clinical evidence of any follicular lesion. J Craniomaxillofac Surg 2007 Jan; 35(1):48-51.
- 7. Theodorou DJ, Theodorou SJ, Sartoris DJ. Primary non-odontogenic tumors of the jawbones: an overview of essential radiographic findings. Clin Imaging 2003 Jan-Feb; 27(1):59-70.
- 8. Kahn LB, Vigorita V. Fibrosarcoma of bone. In: Fletcher CDM, Unni KK, Mertens F, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press, Lyon, France; 2002. p: 289-290.
- 9. Orhan K, Orhan AI, Oz U, Pekiner FN, Delilbasi C. Misdiagnosed fibrosarcoma of the mandible mimicking temporomandibular disorder: a rare condition. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 Oct; 104(4):e26-e29.
- 10. Fletcher CD, Sudaram M, Rydholm A, Coindre JM, Singer S. Soft tissue tumours: Epidemiology, clinical features, histopathological typing and grading. In: Fletcher CDM, Unni KK, Mertens F, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press, Lyon, France; 2002. p. 14-18.
- 11. Yamaguchi S, Nagasawa H, Suzuki T, Fujii E, Iwaki H, Takagi M, et al. Sarcomas of the oral and maxillofacial region: a review of 32 cases in 25 years. Clin Oral Investig 2004 Jun; 8(2):52-55.
- 12. Wadhwan V, Chaudhary MS, Gawande M. Fibrosarcoma of the oral cavity. Indian J Dent Res 2010 Apr-Jun; 21(2):295-298.