| Introduction
Leprosy is feared in almost every culture because of the severe deformities and disabilities it can bring in the absence of early and effective treatments. The mystery surrounding leprosy contagion causes people to reject individuals with signs of leprosy as members of the community. Moreover, because of poverty and the kinds of odd jobs the patients do for a living, they are at risk of infection and/or body damage.1,2
Infections, deformities and ulceration, which result in leprosy patients’ ostracism, could increase their inaccessibility to health- care programs. If this inaccessibility is to be discouraged, then individuals, families and communities must be enabled to develop quality care for discharged patients.3 Whereas continuous medical services are central to care and support of discharged patients, the general philosophy of healthcare workers in settlements is that once leprosy patients have been cured and discharged home, the most essential service is proper reintegration of the patients with their family members. But World Health Organization’s (WHO) global strategies for controlling leprosy demands a holistic treatment hence there may be a relapse because leprosy essentially affects the peripheral nerves.4-6
Studies have shown that leprosy patients discharged home have a higher burden of disease, limited opportunities to access healthcare prevention programs than the leprosy patients residing in settlements.7,8 This conflicting data on quality of healthcare services available to discharged leprosy patients motivated the researchers to examine the medical rehabilitation of discharged leprosy patients in the communities.
Further, studies have highlighted a number of personal, psychosocial, economic, medical and health service factors that militate against effective and efficient service delivery to leprosy patients. However, the current WHO key strategy for leprosy elimination depends largely on the efficiency of healthcare workers in providing healthcare services to leprosy patients uninhibited. Uninhibited healthcare services will reduce noncompliance and improve leprosy disease control programs.9-12
Despite the right of every individual including discharged leprosy patients to HIV prevention, healthy fulfilling sexual life and reproductive choices, factors like discrimination, rejection, stigmatization, and isolation negatively influence such rights for discharged leprosy patients.13-17 Excluding leprosy patients from preventive healthcare programs could present severe health risks for communicable diseases including HIV infection,18-21 recurrent ulcers, deformities and other health problems.22,23
The problem is that reproductive health and policy planners sometimes fail to recognize the complexity of peoples’ lives and the context in which people should receive services.24-26 For instance, the poor socio-economic and environmental conditions of discharged leprosy patients in the communities, especially those with leaking ulcers, and large numbers of children make some healthcare workers conclude that such patients are deviants. These health workers forget that leprosy patients have the right to have sex and children. Health workers need to recognize this and provide leprosy patients with contraceptive advice and services as well as maternal and childcare services.
Health service providers should understand that they contribute to quality life for discharged patients when they make readily accessible treatment and other healthcare services to the patients. The problem is that health providers at times selectively provide healthcare services based on the individual’s social status. The lower the social status of patients, the less accessible health-care services would be.27,28
This selective provision of health services by health workers is part of the difficulty discharged leprosy patients have in getting attention for effective management of ulcers and other complications. This calls for the need to periodically assess the extent to which healthcare programs are available and affordable to discharged leprosy patients in the communities. This study is important because no prior research has focused on the wellbeing of discharged leprosy patients in the communities. Most researches focus on the leprosy patient resident in the settlements to the disadvantage of those discharged home.
Methods
This is a descriptive study which appraised the extent to which medical rehabilitation services are provided to discharged leprosy patients in Ebonyi and Abia States of Nigeria. In appraising the rehabilitation services provided to discharged leprosy patients treated and discharged home in Uzuakoli and Ohaozara leprosy settlements in Abia and Ebonyi States of Nigeria, the extent of after-care services, follow-up visits, healthcare prevention programs (HIV prevention, family planning, health education and others) provided were noted.
The patients treated and discharged home in Uzuakoli and Ohaozara were used because these two settlements are the only functional leprosy settlements in the Southeastern part of Nigeria with some inmates who have been treated are discharged home. These two settlements studied will be interchangeably referred to as Abia and Ebonyi States.
The study sample consisted of all the 33 leprosy patients who were fully treated with multi-drug therapy (MDT) in the two settlements and discharged home. These were made up of 14 discharged leprosy patients in Uzuakoli between 1999 and 2002 and 19 in Ohaozara leprosy settlement within 1998 and 2004, who are resident in the communities and available during the time of the study. Altogether, the sample consisted of 18 (54.5%) males and 15 (45.5%) females. The list of the discharged leprosy patients and their addresses were collected from the settlements where they were treated. This strategy helped the researchers to easily identify and interview the available discharged patients. Further, snowball-sampling method was used to identify the discharged patients whose addresses were difficult to locate. Each discharged patient interviewed was asked to mention other discharged patients living near his or her vicinity. Subsequently, names and vicinity of those mentioned were located and interviewed.
Instruments for data collection were questionnaire, interview guide and checklist. These contained mainly structured questions and were administered. The respondents were essentially those with informal education. The questions in the instruments were coded to reduce factors and conditions that influence accessibility and affordability of healthcare services. The study used seven categories of questions that contained 4-point scale (Strongly agree=SA; Agree=A; Disagree=D; and strongly disagree=SD) to assess medical rehabilitation of discharged patients. This enabled the researchers to note the medical coverage as well as quality of life the patients enjoyed in the communities. Also, a checklist was used to assess the hygienic conditions of the living areas, while the questionnaire assessed medical coverage and health services available to the patients. Data were analysed quantitatively and qualitatively.
For ease of analysis, the 4-points scales were reduced to two extremes, positive and negative responses. Positive responses attracted ‘1’ while negative responses attracted "0." In this study, higher scores meant more health services available to the patients and this translated to better medical rehabilitation.
In the analysis, medical coverage, availability of healthcare services, after-care services, follow-up visits and living conditions of the patients were the inventory used to measure medical rehabilitation for the patients. This method helped the researchers to identify the proportion of discharged leprosy patients who benefited from preventive healthcare and other national programs. It also enabled the researchers to determine the factors and conditions that influenced medical rehabilitation among the discharged patients.
The consents of the Medical Officers and Directors in charge of the two settlements as well as that of the community leaders were sought and their approvals enabled the researchers to interview the patients. The University ethics committee approved the study before the study commenced.
The main limitation of the study is that the discharged leprosy patients studied were those who were treated and discharged in the two leprosy settlements in Abia and Ebonyi States. Those not treated in these two settlements were excluded because of the difficulty in locating them. Societal prejudices about leprosy forced some individuals treated of leprosy to conceal their health conditions from public knowledge. It might be possible that those excluded could be the ones that are well rehabilitated. Again in this study, the researchers used primary data collected by recall methods from the patients and therefore the respondents’ short memory and forgetfulness during interview may give inaccurate information. Also, the collection of secondary data was difficult to some extent because of lack of authentic data from both the settlements and governments.
However, a major strength of this research is that the discharged leprosy patients were encouraged to identify the deficiencies and difficulties in the services provided to them by the health workers. They were also encouraged to analyze their problems from their own perspectives. Through this process, the leprosy patients did not only become aware of the results of the study, they also made important contributions to the research process by assisting the researchers to identify strategies for improving their lives in the communities. The study was carried out only on leprosy patients treated and discharged home in leprosy settlements. Therefore the findings of this study are relevant to discharged leprosy patients treated in leprosy settlements. Also the study used a total sample of leprosy patients fully treated with MDT and discharged home in the two settlements studied.
Results
Because of the relatively small number of discharged leprosy patients found in the settlements in Abia and Ebonyi States, the researchers pooled and analyzed the data from both States. Ebonyi State was created from Abia State in 1992 and therefore, both States have some similarities.
The marital status of the patients consisted of 15 (45.5%) married, 2 (6.1%) single, 6 (18.2%) divorced/separated, and 10 (30.3%) widowed. The ages of the discharged patients were widely distributed. The findings showed that 1 (3%) of the patients was 20-29 years, 4 (12.1%) were 30-39 years, 8 (24.2%) 40-49 years, 7 (21.2%) 50-59 years, 4 (12.1%) were 60-69 while 9 (27.2%) were 70 years and above (mean age 55.8 years±15.2).
A total of 28 (84.8%) of the discharged patients had children while 5 (15.2%) had none. During the study, 9 (27.3%) of them were found either pregnant or nursing a baby. The mean number of children for the leprosy patients was 3.8±2.5.
A good number of the patients 21 (63.7%) had informal education, 11 (33.3%) had primary education, while 1 (3%) had post-secondary. Majority of the patients 27 (81.8%) were Christians, while 6 (18.2%) practiced traditional religion. For the patients’ occupation, 1 (3%) was in public service, 5 (15.2%) were artisans, 2 (6.1%) were palm wine tapers while 25 (75.8%), were subsistent farmers.
Findings on the number of years the patients stayed at home after discharge showed that 20 (60.6%) patients stayed 1-10 years, while 13 (39.4%) patients stayed 11 years and above with mean stay of 12.8 years±12.5. On the number of rooms the patients occupied with their family members, findings revealed that 20 (60.6%) patients occupied only 1-2 rooms, while 13 (39.4%) others lived in 3-4 rooms, with mean number of individuals living with the patients in a room as 4.3±3.2.
Medical coverage, prevention services like (HIV counseling, family planning, health education and others), after-care services, follow-up visits, as well as a checklist of environmental conditions of the patients’ houses were used to assess the extent of medical rehabilitation the discharged patients received.
The patients were asked to state within the last 12 months the extent to which the health workers treated them for minor ailments. The finding showed that within the period under review, the patients received treatment for minor ailments from several places and for various types of ailments, as shown in Table 1.
Table 1 shows that the patients received several modes of treatment from various healthcare institutions but the two common places where they received treatment were the hospitals in the settlements 17 (51.5%), and the traditional healing home 13 (39.4%).
Further investigation from the patients revealed that the patients, irrespective of where they received treatments, they paid for the cost of their treatments. From the data presented in Table 1, it is obvious that none of the patients mentioned health education, HIV counseling or family planning as part of the services they received. Based on this, the patients were asked to state national healthcare services they have ever benefited along with others in the communities. Table 2 contains a summary of their responses.
Table 2 shows that except for immunization services that were accessible to 15 (45.5%) of the patients, other services were scarcely accessible. The reasons for inaccessibility of these services were sought. Table 3 presents the details.
Table 1: Discharged patients and the types of treatments they received for minor ailments.
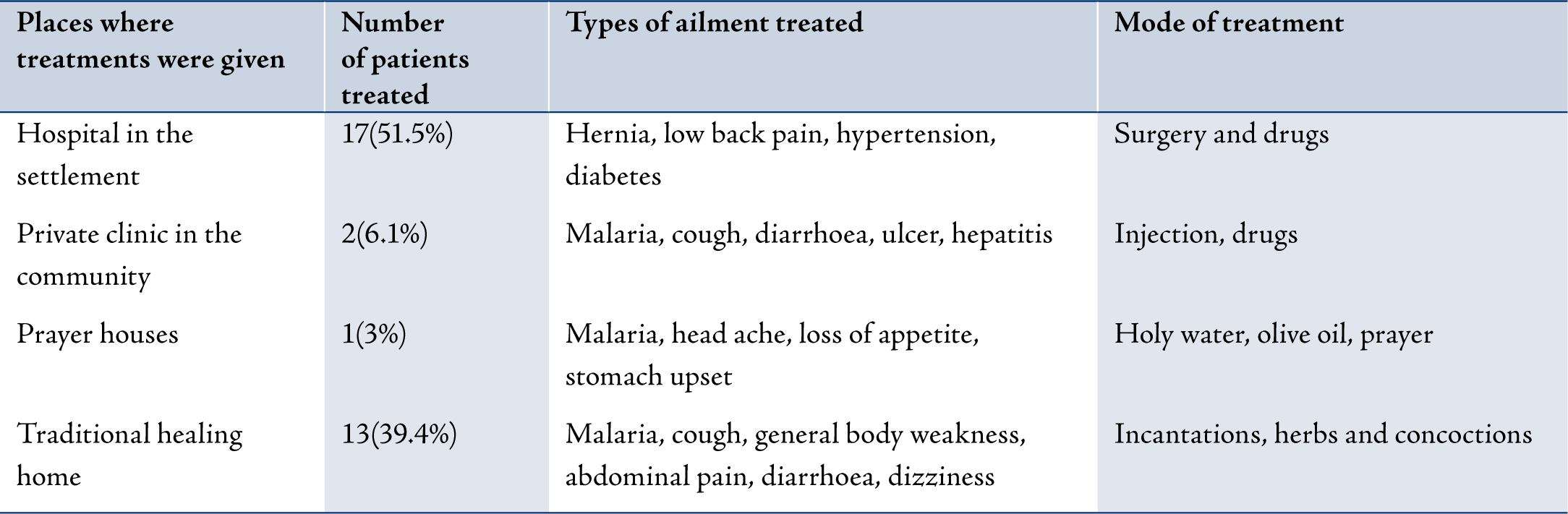
Table 2: Discharged patients and types of national prevention programs ever received.
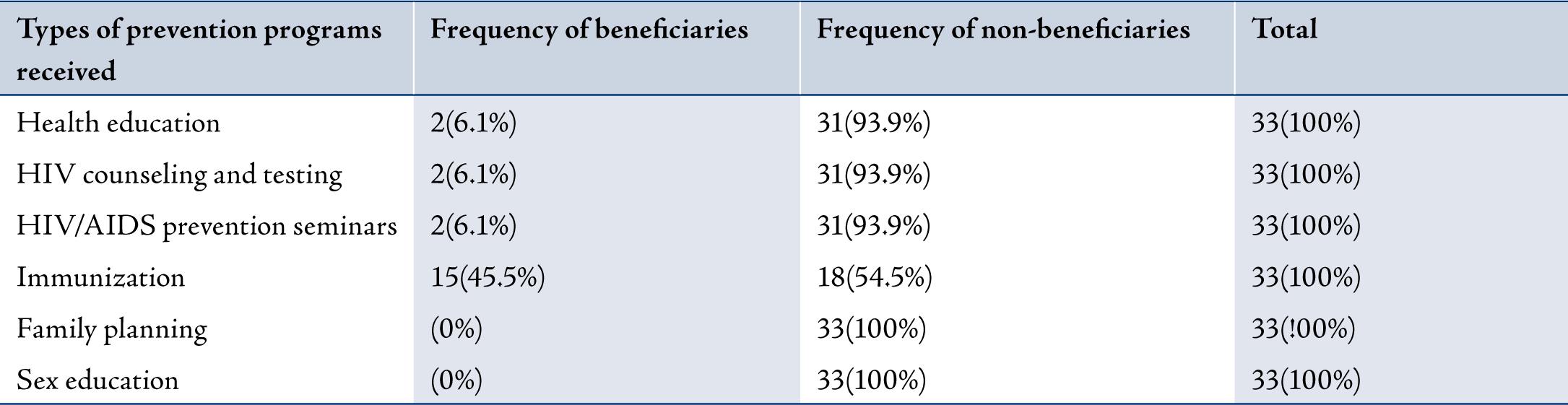
Table 3: Discharge patients and reasons for not accessing prevention services.
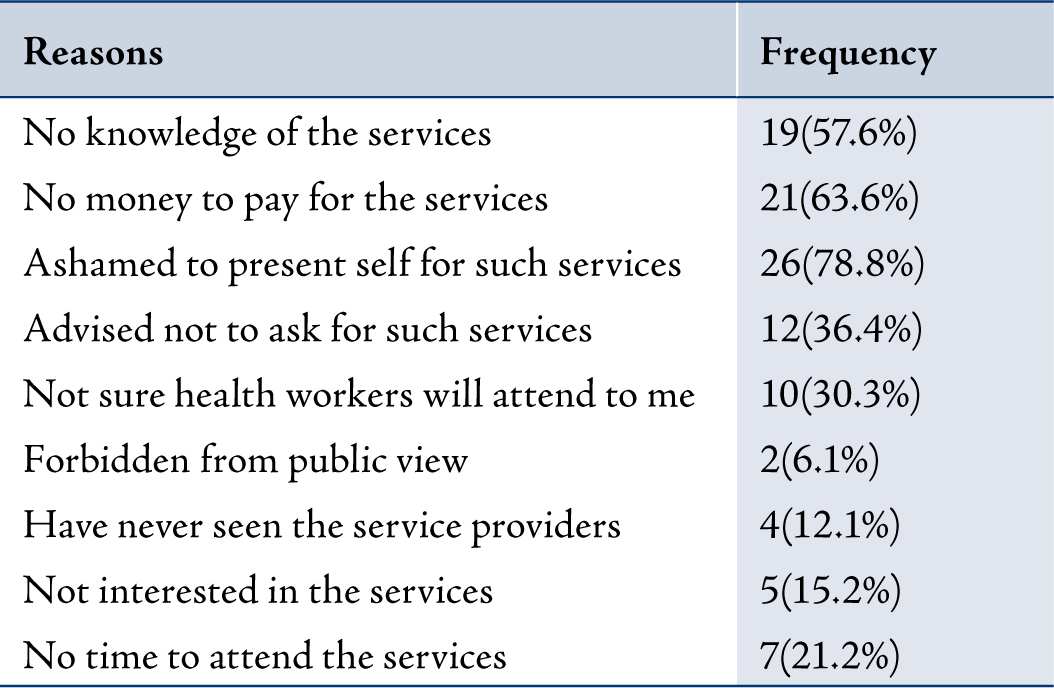
Table 3 shows that the commonest reason given by 26 (78.8%) of the patients for not receiving the services was that they were ashamed to present themselves for the services in the midst of others.
The findings on whether some of the contact persons of the discharged patients were given prophylaxis against leprosy infection showed that relatives of 20 (60.6%) of the patients were given dapsone as prophylaxis. Further findings on whether the prophylaxis given to the contact persons was prescribed by health workers showed that the health workers did not prescribe the dapsone. Rather, the patients themselves, on their own volition gave the dapsone to their relatives. However, during the study, 3 (9.1%) of the discharged patients reported that their children were already infected with leprosy and that the children were also under treatment.
Assessment of the physical conditions of the patients showed that in all, 9 (27.3%) used accessories for mobility. About 4 (12.1%) others were amputees, 3 (9.1%) had deformities that necessitated the use of prostheses, while 2 (6.1%) used crutches. On the whole, 15 (45.5%) of the discharged patients had leaking ulcers.
In assessing the discharged patients’ work capacity, 27 (81.8%) patients signified that they carried out their daily activities unaided, 4 (21.1%) said they only carried out their daily activities if aided, while 2 (6.1%) were incapacitated and incapable of performing their daily activities. These two patients indicated that their children assisted them with all daily activities including washing.
The proportion of patients who attended after-care services and/or received follow-up visits from the health workers were explored and the findings showed that only 19 (57.6%) of the patients attended after-care services, while 10 (30.3%) received follow-up visits from the health workers, but such visits were said to be very sporadic. Patients who neither attended after-care services nor received follow-up visits gave reasons why they did not attend. Using the words of the patients, "we did not receive after-care services because we had no need for such. We have been cured and issued with certificate of fitness; therefore, attending after-care services was unnecessary. It would amount to exposing ourselves further in the communities." Others said, "We did not seek for after-care services because of lack of transport fare and money to pay for the cost of services. We are not doing anything for a living and therefore, do not have money for such services."
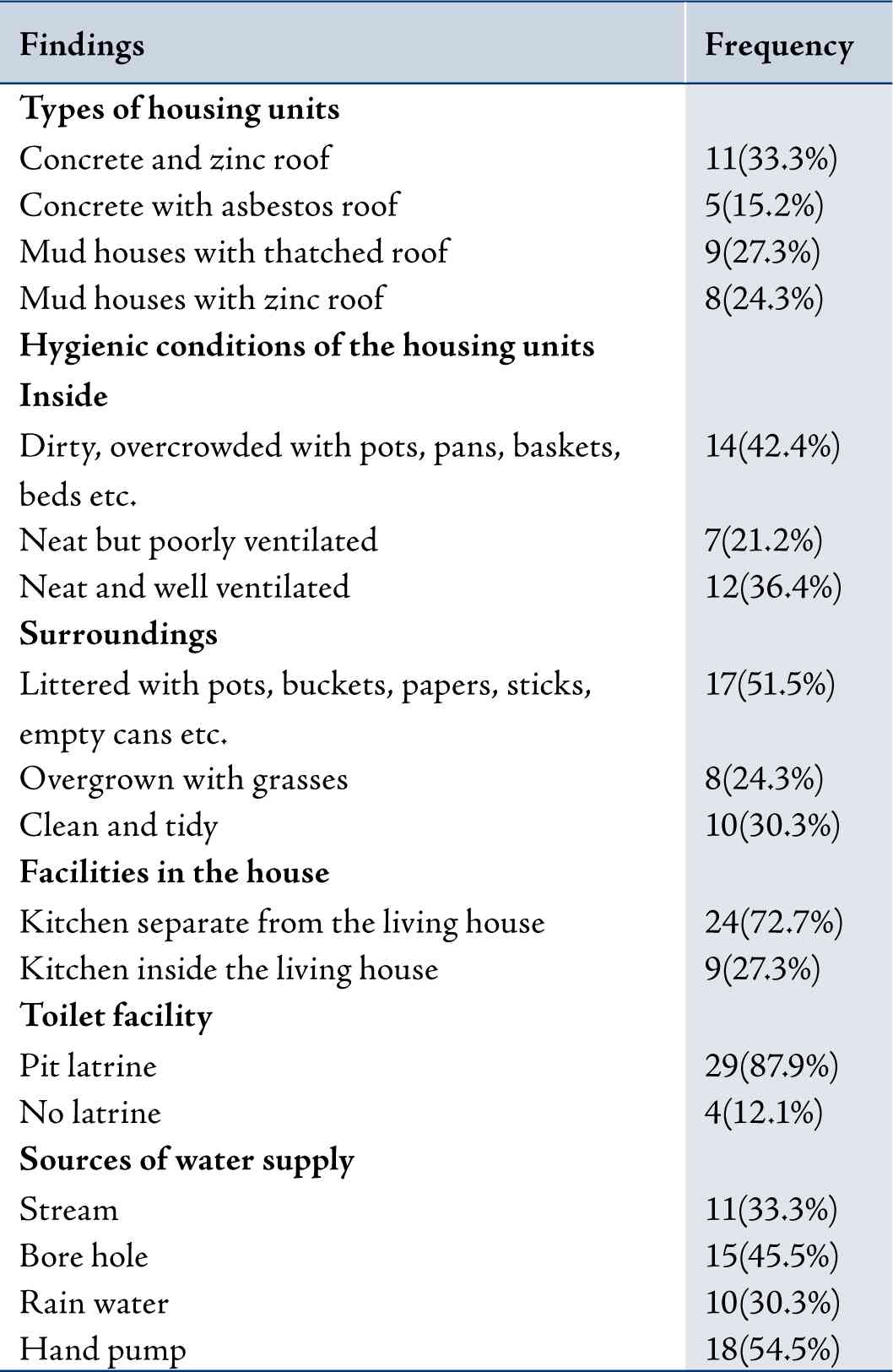
Results from the checklist of the discharged patients’ residential areas showed that 14 (42.4%) patients lived in dirty and overcrowded houses, while 12 (36.4%) lived in neat and well ventilated houses. Table 4 contains the details of the hygienic conditions of the residential areas. The findings revealed that, the environmental conditions of a good number of the patients were not conducive.
Table 4: Summary of findings on the patients living conditions.
Questions on medical coverage, utilization of healthcare services, after-care services, follow-up visits and hygienic conditions of the residential areas were used to assess medical rehabilitation. These questions had obtainable scores that ranged from 0-7 with the cut-off point as 5. Higher scores indicated better medical rehabilitation. The findings showed that 20 (60.6%) of the patients scored 3 to 7 with a mean score of 4.7±1.1. This overall range of scores indicated that the discharged patients were poorly medically rehabilitated.
Sex, age and marital status affected medical rehabilitation. Males with higher mean scores 5.0±1.1 were better medically rehabilitated than females with the mean score of 4.6±1.2, but this was not statistically significant (H=0.11, p=0.74). The mean score increased with age. Patients aged 59–69 years had the highest mean score (5.0±1.1) among all the ages, showing that they were better medically rehabilitated than others. While patients aged 20-29 years had the least mean score of 4.4±1.1, indicating that they were poorly medically rehabilitated; however, this was not statistically significant (F=0.53, p=0.72). In terms of marital status; divorced/ separated patients had a higher mean score (5.0±1.1) and were better medically rehabilitated than their married counterparts with a mean score of 3.5±0.71 (F=1.2, p=0.31).
Discussion
There were discrepancies in the inclusion of discharged leprosy patients in the national prevention and other healthcare programs. It was noted that access to quality healthcare service delivery to discharged leprosy patients was limited, unlike what is available to the general population. For instance, a good number of the discharged patients could not benefit from national healthcare programs like HIV/AIDS prevention, health education, family planning services, including after-care services. This lack of access to healthcare service delivery is a clear manifestation of stigmatization of discharged leprosy patients among health workers. With the recent WHO global health strategy for further reducing leprosy burden and sustaining leprosy control activities, it is critical that leprosy patients should be integrated in national disease prevention services to ensure that avoidable diseases are eliminated among leprosy patients at the same level as in the general population.
Not withstanding the fact that the discharged leprosy patients paid for the cost of all treatments and received limited follow-up visits from the health workers; medical rehabilitation among some groups was fair. The few number of patients who attended after-care services, and also benefited from the national prevention services confirmed this.
The fact that some discharged patients on their own volition, gave prophylaxis to family members indicates high knowledge of the prevention, control and causes of leprosy infection among them. This is in line with the WHO recommendations,3,4 that family members of leprosy patients should be given 1-4 mg dapsone per kilogram (kg/body weight per week) as well as one time intramuscularly injection of acedapsone per 10 weeks interval as prophylactic treatment to protect household contacts.
Age, sex and marital status affected medical rehabilitation of the discharged patients. Males were better medically rehabilitated than females. Also, the more middle aged the patients were (5969 years), the better medically rehabilitated they were. The fact that the divorced/separated in this study enjoyed better medical rehabilitation than others suggests that they were among the few discharged patients who benefited from national prevention programs like HIV counseling and testing, HIV/AIDS prevention seminars, health education and immunization. It could also be that they were among the group of patients that had after-care services; follow-up visits as well as those who lived in clean and non-overcrowded houses. It might be safe to assume that the divorced/separated patients enjoyed better medical rehabilitation probably because of their concern to prevent visible bodily disfigurements so as to increase their chances of remedying their broken marriage.
Conclusion
The problems associated with overcrowding, poor environmental conditions, lack of after-care services and follow-up visits are well recognized and therefore call for provision of health education. It is clear that stigmatization among leprosy patients in Nigeria has not been eliminated and this affects their access to national prevention services. By implementing health education services, it is hoped that inclusion of leprosy patients in the national healthcare prevention programs might help reduce the prevalence of diseases like HIV and other sexually transmitted diseases among them. It is critical to expect already impoverished leprosy patients to pay for their treatments. Asking them to pay for treatments could initiate situations where many of them would forgo health services because of the costs. This could delay seeking medical attention even for preventable health conditions. Discharged leprosy patients should therefore be allowed free treatments for all forms of diseases.
Realizing that amidst abject poverty, some patients were found pregnant notwithstanding the fact that their mean number of children was 3.8±2.5 suggests urgent need for family planning services to limit the number of children they would have.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work. |