While it is common to diagnose fallopian tube torsion along with ovarian torsion, isolated tubal torsion without ovarian involvement is a rare entity, with an overall incidence of one in 1.5 million women since the first reported case in 1890.1–3 Female patients presenting to the emergency department with acute lower abdominal pain have a broad differential diagnosis. Ultrasonography is the initial imaging modality of choice in such cases, with ovarian torsion being the most common provisional diagnosis. However, ovarian torsion has specific ultrasonographic features, such as enlarged ovaries and impaired Doppler flow. In contrast, in isolated tubal torsion, these findings do not apply, and ultrasound (US) imaging may be less effective.4 Clinicians may opt for computed tomography (CT) imaging, especially if the presentation suggests gastrointestinal or urological issues, adding to the diagnostic complexity due to the lack of specific features on CT. Radiologists and gynecologists need to be aware of this entity for a prompt clinical diagnosis and improved clinical outcomes.
Case report
A 38-year-old female patient presented in the evening with severe lower abdominal pain since that morning. The patient had been treated with analgesics in an outside hospital, but the pain persisted. The patient had a history of two lower-segment cesarean sections and had undergone sterilization. Her last menstrual period was 15 days prior. On examination, the abdomen was normal except for tenderness in the left iliac fossa. Per speculum and per vaginal examination revealed tenderness in the left vaginal fornix with no other abnormalities. Serum beta-hCG < 0.100 mIU/mL, and the total count was 11 500 cells/mm3, with 85% neutrophils. The provisional clinical diagnosis was ovarian torsion or tubo-ovarian mass. Emergency US (USG) of the abdomen and pelvis showed a normal uterus with a normal endometrium and bilateral polycystic ovaries. An anechoic tubular structure (3.2 × 2.2 cm) with incomplete septation, suggestive of hydrosalpinx, was seen in the left adnexa, surrounded by a hyperechoic area with significant internal vascularity [Figure 1]. Arterial and venous flow were observed within the left pedicle. The diagnosis on USG was left hydrosalpinx with salpingitis or early phlegmon. A plain CT of the abdomen was advised to rule out any bowel pathology, but it did not provide additional insights into the diagnosis, except for a bulky left adnexa.
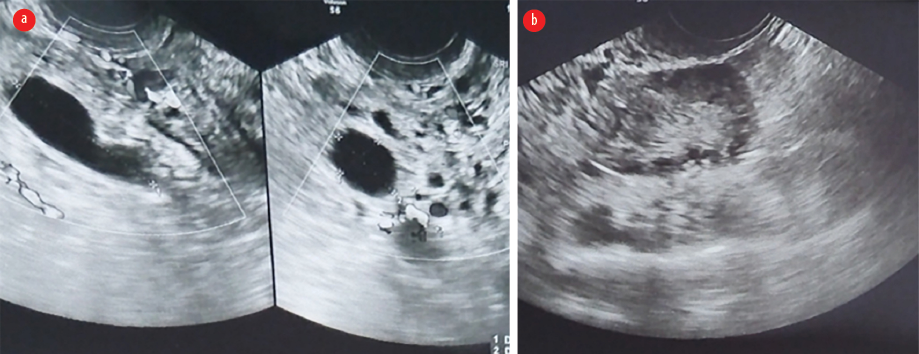 Figure 1: (a) Emergency ultrasound image showing tubular, anechoic, hydrosalpinx with surrounding increased echogenicity, heightened vascularity, and (b) polycystic right ovary with no features of torsion.
Figure 1: (a) Emergency ultrasound image showing tubular, anechoic, hydrosalpinx with surrounding increased echogenicity, heightened vascularity, and (b) polycystic right ovary with no features of torsion.
Given the persistent and severe pain refractory to analgesics, the patient underwent emergency diagnostic laparoscopy. Intraoperatively, the left fallopian tube was found to be dilated, congested, and twisted at its cornual end, while the left ovary was normal. Hence, a left salpingectomy was performed after detorsion [Figure 2]. As there was a right hydrosalpinx, a right salpingectomy was also performed. The right ovary and uterus were normal, and adequate hemostasis was achieved; the ports were sutured. Postoperative, the patient was comfortable and was discharged with antibiotics. The patient experienced complete relief from pain. Informed written consent was obtained from the patient for the publication of this case report.
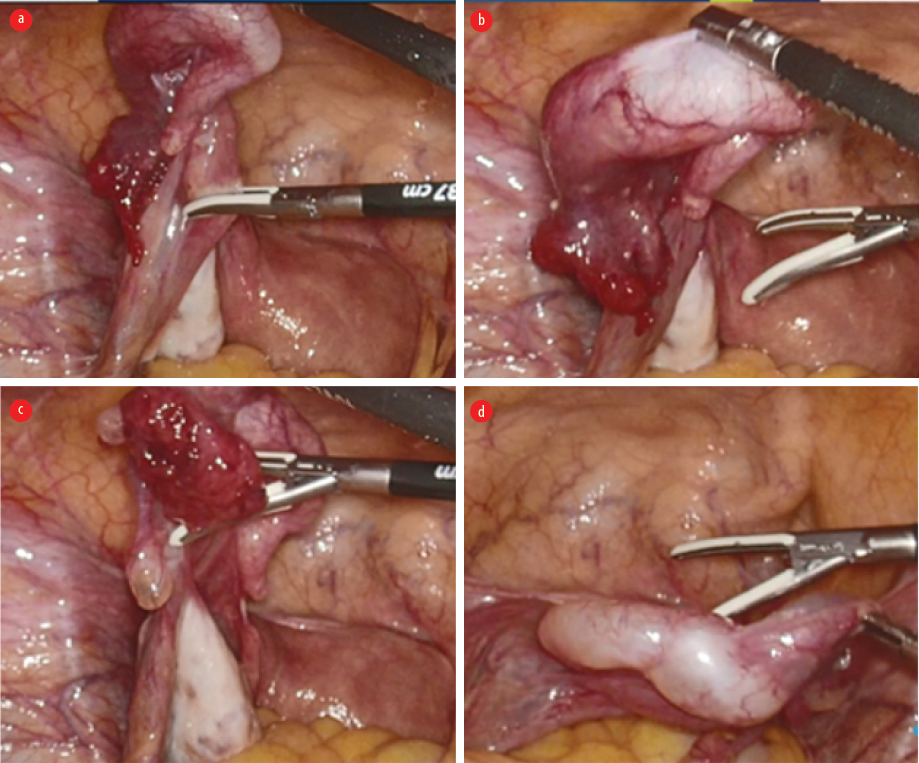 Figure 2: Laparoscopic intraoperative images showing (a) torsed fallopian tube and mesosalpinx, (b) partial detorsion of dilated fallopian tube, (c) partial detorsion of mesosalpinx, and (d) fully detorsed mesosalpinx with hydrosalpinx.
Figure 2: Laparoscopic intraoperative images showing (a) torsed fallopian tube and mesosalpinx, (b) partial detorsion of dilated fallopian tube, (c) partial detorsion of mesosalpinx, and (d) fully detorsed mesosalpinx with hydrosalpinx.
Discussion
Acute pelvic pain can manifest from various conditions such as ovarian torsion, mittelschmerz, adnexal ectopic pregnancy, pelvic inflammatory disease, appendicitis, diverticulitis, intestinal obstruction, ureteric/bladder calculus, or uncommon entity like tubal torsion.5 Risk factors for isolated tubal torsion include hydrosalpinx, pelvic inflammatory disease, tubal ligation, tubal adhesion, tubal neoplasm, adnexal venous congestion, adjacent ovarian or paraovarian neoplasm, uterine masses, gravid uterus, and trauma.6
In our case, tubal torsion was secondary to tubal ligation and was associated with hydrosalpinx. Post-tubal ligation, fallopian tube torsion has unique and interesting implications. Unlike other causes, abnormal mobility and an abnormal bulk of the tube are required before the fallopian tube undergoes torsion, as in our case. According to Cox,7 division of the tube deprives the lateral part of any stability it might obtain from continuity with the medial part, facilitating torsion. Other authors theorize that torsion results from cutting too deeply into the mesosalpinx, allowing excessive rotation and movement of the oviduct.8 According to Ottesen et al,9 increased mobility is caused by severing or at least constricting the attachment of the tube to the uterus. The increased bulk of the fallopian tube is produced when secretions from the tube can no longer travel into the uterus, resulting in a hydrosalpinx.
Most documented cases were reported several years after tubal ligation.10 Therefore, it is unlikely that the surgery itself is a risk factor. Mechanical risk factors believed to predispose ovarian torsion, such as ovarian masses or cysts causing asymmetric weighting of the ovaries, also do not apply to patients with post-tubal ligation.
According to literature on ultrasonography, some patients with tubal torsion had free pelvic fluid, some had cystic adnexal masses, and others had no significant findings.3,8,9,10 This suggests that USG may be less helpful in assessing torsion in patients with post-bilateral tubal ligation, and such patients may go underdiagnosed if clinicians assume an US is sufficient to rule out torsion. The definitive diagnosis of isolated tubal torsion ultimately requires laparoscopy.4
In our case, there were nonspecific findings of hydrosalpinx with increased adnexal echogenicity and a normal ovary. The heightened echogenic area may represent the torsed, inflamed tubal tissue on retrospective analysis. The right hydrosalpinx was obscured by bowel gas.
If tubal torsion is not diagnosed promptly, it can lead to necrosis, gangrene, superinfection, peritonitis, and eventual ischemia or damage to the adjacent ovary.5,11 Treatment can range from detorsing the tube to salpingectomy or even salpingo-oophorectomy.1
Conclusion
In nonpregnant female patients with acute pelvic pain, especially post-tubal ligation, the differential diagnosis should include tubal torsion. Awareness of this specific entity enables clinicians to make a prompt diagnosis, given its challenging imaging presentation, and often necessitates surgical intervention. This proactive approach helps in preventing complications and mitigating the need for unnecessary investigations.
Disclosure
The authors declare no conflicts of interest.
Acknowledgments
We sincerely thank the members of the Department of Radiology, Department of Obstetrics and Gynaecology, Emergency Department, Nursing team, and operation theatre team of NMC Specialty Hospital for their contributions in treating and taking care of this patient.
references
- 1. Lo GC, Kadoch MA, Simpson Jr W. Isolated fallopian tube torsion: two case reports of a rare entity. Clinical Imaging 2016 Sep 1;40(5):1004-1008.
- 2. Bharathi A, Gowri M. Torsion of the fallopian tube and the haematosalpinx in perimenopausal women-a case report. J Clin Diagn Res 2013 Apr;7(4):731-733.
- 3. Raziel A, Mordechai E, Friedler S, Schachter M, Pansky M, Ron-El R. Isolated recurrent torsion of the fallopian tube: case report. Hum Reprod 1999 Dec;14(12):3000-3001.
- 4. Gurley AL, Choi S, Okour S. Isolated tubal torsion following bilateral tubal ligation: a case report and literature review. Case Rep Womens Health 2022 Jun;35:e00426.
- 5. Ferrera PC, Kass LE, Verdile VP. Torsion of the fallopian tube. Am J Emerg Med 1995 May;13(3):312-314.
- 6. Provost MW. Torsion of the normal fallopian tube. Obstet Gynecol 1972;39(1):80-82.
- 7. Cox BS. Unusual examples of adnexal torsion. British Medical Journal 1967 Jul 7;3(5560):308-309.
- 8. Shapiro HI, Hughes WF, Adler DH. Torsion of the oviduct following laparoscopic sterilization. Am J Obstet Gynecol 1976 Nov;126(6):733-734.
- 9. Ottesen B, Shokouh-Amiri MH, Hoffmann J. Torsion of the fallopian tube following tubal sterilization by electrocoagulation via a laparoscope. Eur J Obstet Gynecol Reprod Biol 1985 May 1;19(5):297-300.
- 10. Poma PA, Barber A. Fallopian tube necrosis after postpartum sterilization. J Natl Med Assoc 2001 Apr;93(4):149-150.
- 11. Ghossain MA, Buy J-N, Bazot M, Haddad S, Guinet C, Malbec L, et al. CT in adnexal torsion with emphasis on tubal findings: correlation with US. J Comput Assist Tomogr 1994;18(4):619-625.