Nasopharyngeal carcinoma or nasopharyngeal cancer (NPC) is a tumor arising from the epithelial cells that cover the surface and line the nasopharynx. It was first described as a separate entity by Regaud and Schmincke in 1921.1,2
NPC is a relatively uncommon malignant disease with an incidence of less than 1:100,000.3 Genetic, ethnic, and environmental factors play roles in the etiology of this disease. It was noticed that Chinese immigrants to Southeast Asia or North America had a higher incidence than North American-born Chinese populations.
Consumption of salted fish is one of the causative factors of NPC, which might be related to carcinogenic nitrosamine detected in the fish. Epstein–Barr virus (EBV) infection also plays a role in the etiology of NPC and has been demonstrated in situ carcinomas of the nasopharynx, which are presumed precursor lesions of NPC.4,5
This study used medical records from the ENT and Head and Neck departments, Al Nahdha Hospital, for all Omani patients with NPC who presented to the hospital from January 2003 until August 2011. We sought to identify the most common clinical presentation of the disease, its association with certain tribes in Oman, and any region specificity.
Methods
A retrospective chart analysis was performed of all NPC cases that presented to Al Nahdha Hospital between January 2003 and August 2011. Data was collected from the hospital patient data system (Al-Shifa) using the search code “Malignant Neoplasm of Nasopharyx, Unspecified” with a diagnosis of nasopharyngeal mass. Cases were then categorized into cancer and non-cancer according to the final diagnosis. Only those cases with a confirmed diagnosis of cancer were analyzed, according to age, sex, tribe, region distribution, clinical presentation, histopathology diagnosis, treatment modality, recurrence, and metastasis. Analysis was performed using SPSS, version 16 (SPSS Inc., Chicago, USA). A p-value of <0.050 was considered significant.
All Omani patients with a diagnosis of NPC proven by histopathology were included in the study. Non-Omani patients and those with benign nasopharyngeal mass or inconclusive histopathology were excluded.
A total of 32 cases were found in the initial data collection. Two cases were excluded as they were non-Omanis and four cases were excluded as the final histopathology report determined that the mass was not malignant. The follow-up period ranged from six months to seven years according to the available patient records.
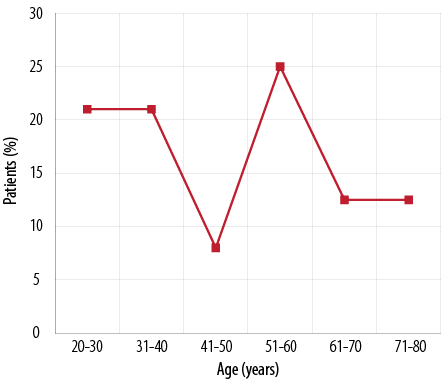
Figure 1: Patient distribution by age.
Results
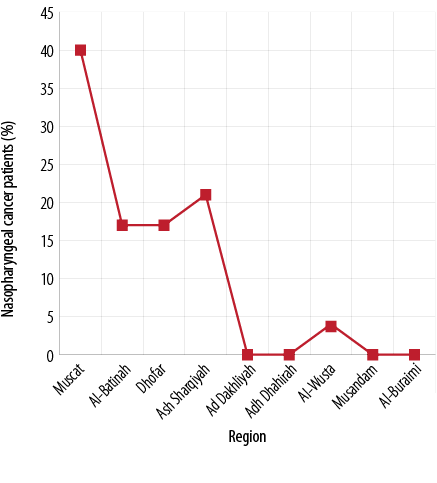
Figure 2: Distribution of nasopharyngeal cancer cases by region.
Table 1: Nasopharyngeal cancer stage at time of diagnosis.
|
Stage I |
4 |
15.4 |
23.5 |
|
Stage II |
1 |
3.8 |
5.9 |
|
Stage III |
2 |
7.7 |
11.8 |
|
Stage IV |
10 |
38.5 |
58.8 |
|
Unknown, but not metastatic |
4 |
15.4 |
- |
|
Unknown, metastatic |
3 |
11.5 |
- |
|
Unknown |
2 |
7.7 |
- |
Twenty-six patients were included in the final study population. The male to female ratio was 1.4:1. When considering age, patients were noted to exhibit a bimodal distribution: 21% of patients were in the 20–30 year old group and 25% in the 50–60 year old age group [Figure 1].
Most cases of NPC were from the capital city, Muscat, representing 40% of the total number, followed by 21% in the Ash Sharqiyah region. In addition, both Dhofar and Al-Batinah (now divided into North Batinah and South Batinah) had a similar significant number of cases both representing 17% of the total figure. There were no cases recorded from the Adh Dhahirah, Ad Dhakhliyah, Musandam, and Al-Buraimi regions [Figure 2].
Considering the tribe names (the Family name), it was noted that most of the cases were from the Al-Balushi tribe (23%) and all were from Muscat (p= 0.031) [Figure 3].
Most cases presented with either presence of a neck mass or with nasal symptoms (bleeding or block) and represented 35.7% of cases each. The second most common symptom was ear pain or ear block, which accounted for 25% of cases, and only 3.6% of cases complained of tinnitus. No cases presented with cranial nerve involvement [Figure 4].
Histopathological examination showed that 69.2% of cases were undifferentiated squamous cell carcinoma (WHO Type 3) and 23% were well-differentiated squamous cell carcinomas (WHO Type 1). There was only one case of nasopharyngeal lymphoma and one case of lymphoepithelioma found, representing 3.8% each of the total number of cases [Figure 5].
Most cases were treated by concurrent chemoradiotherapy (66%) followed by adjuvant chemotherapy. Almost a quarter of cases (23%) were treated by radiotherapy alone, but 3.3% of cases were treated by chemotherapy alone. In addition, 6.6% of cases had persistent neck nodes post-chemoradiotherapy and were treated with neck dissection [Figure 6].
The stage of the disease at the time of diagnosis was only found in 17 cases out of 26, in the remaining eight cases the stage was not mentioned. Adjusted percentage was calculated to find any association. Most cases first presented to the clinic at stage IV followed by stage I [Table 1].
Looking at the association between the region and the stage at presentation, no significant association was found (p=0.297) [Table 2].6
The majority of patients (76%) had no recurrence and only 12% had locoregional recurrence. The follow-up data showed that 88% of patients were on regular follow-up (median=4.5 years/53 months). However, 12% of the cases were lost to follow-up. Distant metastasis to either lungs, liver, or bone (with equal percentages) was found in 12.5% of patients. Unfortunately, there was insufficient data from the medical records regarding the risk factors related to NPC, especially any history of smoking.
Table 2: Association between region and stage at diagnosis.
|
Muscat
Al-Batinah
Dhofar
Ash Sharqiyah
Al-Wusta
Ad Dhakhliyah
Adh Dhahirah
Al-Buraimi
Musandam |
3
0
0
0
1
0
0
0
0 |
0
0
0
1
0
0
0
0
0 |
1
0
0
1
0
0
0
0
0 |
4
3
2
1
0
0
0
0
0 |
8
3
2
3
1
0
0
0
0 |
47.0
17.6
11.8
17.6
6
0
0
0
0 |
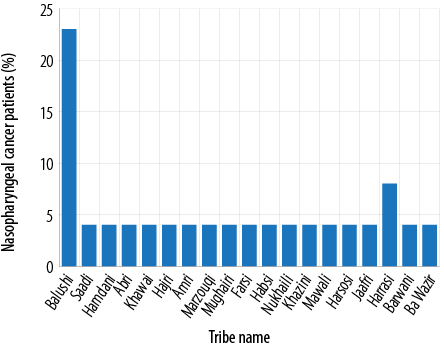
Figure 3: Distribution of nasopharyngeal cancer cases by tribe name.
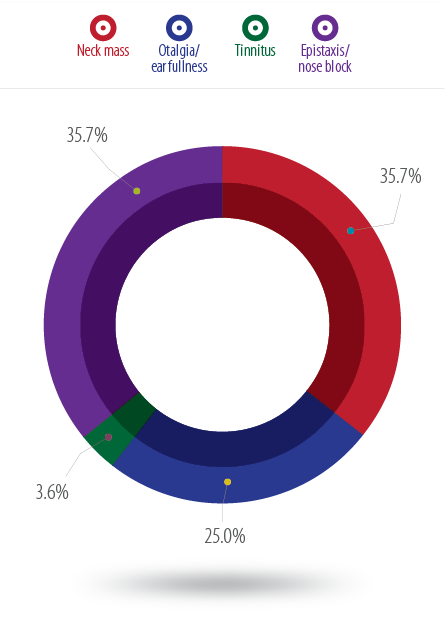
Figure 4: Presentation mode in patients with nasopharyngeal cancer.
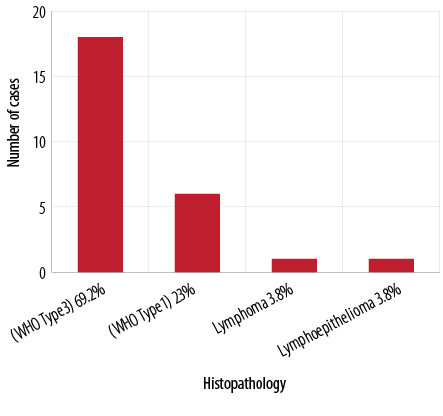
Figure 5: Histopathology of nasopharyngeal cancer cases.
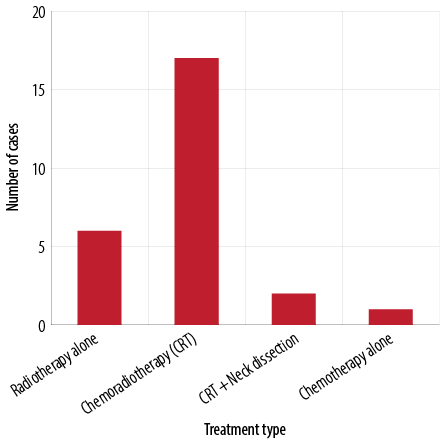
Figure 6: Treatment modality in NPC cases.
Discussion
NPC originates in the lateral wall of the nasopharynx, which includes the fossa of Rosenmuller. It can then extend within or out of the nasopharynx to the other lateral wall and/or posterosuperiorly to the base of the skull, inferiorly to the palate, anteriorly to the nasal cavity or posteroinferiorly to the oropharynx. It then typically metastasizes to the cervical lymph nodes. Distant metastases may occur in the bone, lung, mediastinum and, rarely, the liver.7,8
In our study, the male to female ratio was 1.4:1, which is similar to the ratio internationally. Neck mass is the most common presentation mode of NPC, followed by aural then nasal symptoms.9
Our study showed that the most common presentation of NPC is neck mass and nasal symptoms of obstruction and epistaxis. Ear symptoms were less common. The incidence rate of NPC in Oman (2.3:100,000) is slightly higher than the worldwide incidence of 1:100,000.10 Most cases were from Muscat with an incidence rate of 1.2:100,000,10 which could be due to the larger population size compared to other regions. There may also be an element of bias since a lot of people work in the capital city and sometimes give a local address in Muscat rather than their original place of residence.
It was found that most NPC cases were within the Al-Balushi tribe. The Baloshi, Balochi, or Baluchi tribe originates from East Balochistan, a western province of Pakistan (approximately 50% of their population still lives there). Forty-percent of Balochi are settled in Sindh, Pakistan, and a significant number of the Baloch people live in South Punjab, Pakistan. The rest live in Iran, Afghanistan, Turkmenistan, Oman, the United Arab Emirates, Bahrain, Kuwait, India, and in some parts of Africa. Small communities of Baloch people also live in Europe particularly Sweden, Norway, Denmark, England, and Perth, Australia, where they arrived in the 19th century.11-13 We are not sure when exactly this tribe moved to Oman and there is no sufficient information regarding their unique lifestyle habits (i.e. smoking or chewing tabacco) or genetic predisposition.
In general, 7% of Omanis (13.4% males and 0.5% females)14 smoke (including pipes, shisha, and cigarettes). Anecdotal evidence suggests that most smokers live in Dhofar and Muscat. However, there is no study that provides information on the distribution of smokers by region.
Dhofar is situated in the south of Oman, which is known for the production and use of frankincense. The resin is obtained by slashing the bark of the Boswellia sacra tree and allowing the sap to bleed out and harden. Some chemicals found in frankincense are acid resin, 3-acetyl-beta-boswellic acid, alpha-boswellic acid, phellandrene, 4-O-methyl-glucuronic acid, incensole acetate, and gum. Frankincense can be used in perfumery and aromatherapy, skin care, and traditional medicine.15 Frankincense has also been shown to have cancer-killing properties, and has the potential to destroy ovarian cancer cells when used in the oil form.16 However, the long-term use of frankincense (in smoke form) is associated with an increased risk of squamous cell carcinoma of the respiratory tract.17
A Chinese study looking at region distribution of NPC suggested that the differences over time of NPC in different areas may be related to changes in risk factor exposure in the corresponding populations.18 Although there is no strong supportive evidence, it may be attributable to the changing lifestyle among local residents from traditional Chinese to Western diets, followed by rapid economic growth and development in these corresponding areas. Changes in smoking habits, pickled food intake, and immigration may also have great influences on incidence.18-20
Our observation that Muscat and Dhofar followed by Ash Sharqiyah and Al-Batinah have the most number of cases could be attributed to the fact that all of them are located in coastal regions. In these regions, the process of preserving and canning of highly salted fish is famous (known locally as Al-Maleh) adds another risk factor.
No cases were recorded in Adh Dhahirah, Musandam and Al-Buraimi, which could be explained due to the locations of these areas close to the borders of the United Arab Emirates (UAE). Most people in these areas seek medical treatment in the UAE as it is closer than Muscat.
There are three subtypes of NPC recognized by the WHO classification:21
- Type 1: keratinizing squamous cell carcinoma.
- Type 2: non-keratinizing carcinoma.
- Type 3: undifferentiated carcinoma.
All three types express cytokeratin, and types 2 and 3 have incorporation of EBV into their genome, and circulating IgA antibodies to EBV in the peripheral blood.
Our study showed that most of the Omani patients had type 3 NPC, which is related to EBV. However, there was no data concerning EBV markers as tests for these are not done in our hospital. The Cologne modification of the WHO scheme by Krueger and Wustrow21 includes the degree of lymphoid infiltration. Types 2 and 3 may be accompanied by an inflammatory infiltrate of lymphocytes, plasma cells, and eosinophils, which are abundant, giving rise to the term lymphoepithelioma and which we had only one case.
The mainstay of treatment of NPC is external beam radiotherapy, followed by adjuvant chemotherapy. Surgery has little role in the management of NPC other than for the purpose of diagnostic biopsy.22 Most of our patients were treated by combined chemoradiotherapy followed by adjuvant chemotherapy.
Three patients had recurrence, out of which two had local recurrence and one was treated by radiotherapy. The third patient had regional recurrence that was treated by radical neck dissection.
Conclusion
NPC is considered a rare entity in Oman and it usually presents at a late stage. Neck mass and nasal symptoms are the most common presentation in most cases of NPC in Oman. It is most common in Muscat followed by the Ash Sharqiyah region and among the Al-Balushi tribe. A study of lifestyle habits among this tribe, including dietary habits, and a look at EBV serology is recommended to further support our findings. To consolidate our results, we recommend conducting a prospective study with a larger sample size.
Disclosure
The authors declared no conflict of interests. No funding was received for this study.
references
- Regaud C. Lympho-épitheliome de l’hypopharynx traité par la roentgenthérapie. Bull Soc Franc Otorhinolaryngol. 1921;34:209-214.
- Schmincke A. Über lymphoepitheliale Geschwülste. Beitr Pathol Anat 1921;68:161-170.
- Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas D. Cancer incidence in five continents. Volume VIII. IARC Scientific Publication No. 155. IARC Press; 2003.
- Pathmanathan R, Prasad U, Sadler R, Flynn K, Raab-Traub N. Clonal proliferations of cells infected with Epstein-Barr virus in preinvasive lesions related to nasopharyngeal carcinoma. N Engl J Med 1995 Sep;333(11):693-698.
- Niedobitek G, Agathanggelou A, Nicholls JM. Epstein-Barr virus infection and the pathogenesis of nasopharyngeal carcinoma: viral gene expression, tumour cell phenotype, and the role of the lymphoid stroma. Semin Cancer Biol 1996 Aug;7(4):165-174.
- Greene FL, Page DL. AJCC cancer staging manual. 6th Edition. Chapter 6.
- Som PM, Bergeron T, eds. Head and neck imaging. St Louis Mo.: Mosby-Year Book; 2003.
- Hayat MA, ed. Cancer imaging. Amsterdam: Elsevier, Academic Press; 2008.
- Imad K. Mahid Iqbal, Adnan Yar Muhammad. Presentation of Nasopharyngeal Carcinoma. Available at: www.jpmi.org.pk › Home › Vol 19, No 2 (2005). Accessed January 2011.
- The Oman Cancer National Registry. 2011. Available at: http://ghdx.healthdata.org/record/oman-cancer-incidence-oman-report-2011. Accessed August 18, 2014.
- Pakistan: A Country Study. Edited by Peter R. Blood. Washington: GPO for the Library of Congress; 1995.
- Bray D, Rai J. Ethnographic Survey of Baluchistan. Bombay, India: The Times Press; 1913.
- Janmahmad. The Baloch Cultural Heritage. Karachi, Pakistan: Royal Book Company; 1982.
- Al Riyami AA, Afifi M. Smoking in Oman: prevalence and characteristics of smokers. East Mediterr Health J 2004 Jul-Sep;10(4-5):600-609.
- Olibanum.—Frankincense. Available at: www.henriettesherbal.com. Accessed January 14, 2009.
- Adkins S. Frankincense Effective in Killing Ovarian Cancer Cells. University Herald: 2013.
- Friborg JT, Yuan JM, Wang R, Koh WP, Lee HP, Yu MC. Incense use and respiratory tract carcinomas: a prospective cohort study. Cancer 2008 Oct;113(7):1676-1684.
- Luo J, Chia KS, Chia SE, Reilly M, Tan CS, Ye W. Secular trends of nasopharyngeal carcinoma incidence in Singapore, Hong Kong and Los Angeles Chinese populations, 1973-1997. Eur J Epidemiol 2007;22(8):513-521.
- Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin 2005 Mar-Apr;55(2):74-108.
- Lee AW, Foo W, Mang O, Sze WM, Chappell R, Lau WH, et al. Changing epidemiology of nasopharyngeal carcinoma in Hong Kong over a 20-year period (1980-99): an encouraging reduction in both incidence and mortality. Int J Cancer 2003 Feb;103(5):680-685.
- Krueger GR, Wustrow J. Current classification of nasopharyngeal carcinoma at Cologne University. In: Grundmann E, Krueger GRF, Ablashi DV, editor. Nasopharyngeal carcinoma. Vol. 5. Stuttgart: Gustay Fisher; 1981. p. 11–15.
- King AD, Vlantis AC, Tsang RK, Gary TM, Au AK, Chan CY, et al. Magnetic resonance imaging for the detection of nasopharyngeal carcinoma. AJNR Am J Neuroradiol 2006 Jun-Jul;27(6):1288-1291. AJNR Am J Neuroradiol.