|
Abstract
Pregnancy luteoma is a non-neoplastic lesion of the ovary occurring during pregnancy and is usually discovered incidentally at the time of a cesarean section or during postpartum tubal ligation. An accurate diagnosis is important for the mother and the fetus as it can be confused with ovarian malignancy leading to unnecessary surgery. We report a case of a pregnant female who was discovered to have bilateral enlarged ovaries at the time of emergency cesarean section.
Keywords: Pregnancy; Luteoma; Postpartum.
Introduction
Pregnancy luteoma is a rare non-neoplastic hormone dependant tumor-like lesion of the ovary that was first described by Sternberg in 1963.1 It is usually discovered incidentally at the time of a cesarean section or during postpartum tubal ligation. Most cases resolve completely in about three months postpartum.2 It may be a diagnostic and management challenge as it can mimic the presentation of malignant ovarian tumors.3 An accurate diagnosis is important for both mother and fetus since it can be confused with ovarian malignancy leading to unnecessary surgery.4
The etiology is unclear and it has been postulated that the pregnancy luteoma arises from pre-existing luteinised stromal cells, which respond in an exaggerated manner to the elevated levels of gonadotropin during pregnancy.5 A case is reported of a pregnant female who was discovered to be having bilateral enlarged ovaries at the time of emergency caesarean section.
Case Report
A 21-year-old primigravida underwent emergency cesarean section for fetal distress. A female baby was delivered uneventfully. Per-operatively, both ovaries were found to be enlarged with a maximum dimension of 8 cm each and a smooth outer surface. Bilateral partial oophorectomy was performed. On gross examination, the cut sections were gray brown, edematous and firm. Microscopically, sections from both right and left ovarian masses showed similar findings and revealed a lesion composed of diffusely masses of cells arranged in nests, cords and follicular pattern containing colloid like material (Fig 1). Irregular spaces were seen in between the masses of cells containing RBCs. Intervening stroma showed edema. The cells were polygonal in shape and had abundant amount of finely granular eosinophilic cytoplasm showing vacuolations at places (Fig 2). Nuclei were small, round, vesicular and had prominent nucleoli. Occasional mitotic figures, areas of necrosis and focal areas of hemorrhage were noted. Based on the clinical and histopathological findings a diagnosis of bilateral pregnancy luteoma was made. The patient was observed closely in postpartum period.
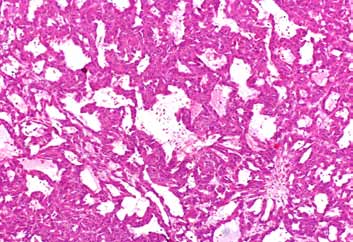
Figure 1: Microphotograph showing masses of cells arranged in follicular pattern (H&E X 100).
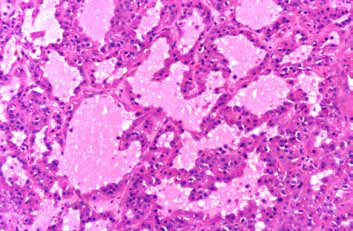
Figure 2: High power view showing colloid like material filling the follicles that are lined by polygonal cells containing small, round nuclei and abundant eosinophilic cytoplasm (H&E X 400).
Discussion
Pregnancy luteoma is a non-neoplastic lesion of the ovary occurring during pregnancy and is known to spontaneously regress, which begins within days after the delivery. The serum androgen levels decrease rapidly after delivery usually reaching normal concentration within 2 weeks postpartum.3 To date, fewer than 200 cases have been reported in literature.5,6 The patients are usually in their third or fourth decade of life.2,3,7 Bilateral lesions are reported in one third of the cases; as seen in our patient.3,7 Most patients with luteoma of pregnancy are asymptomatic with an enlarged ovary, discovered incidentally during cesarean section or at the time of postpartum tubal ligation.3,8 In 25% of the cases, luteomas are hormonally active leading to secretion of androgens causing masculinization in mothers and female infants (60-70% cases).5,9 The index case did not show any signs of virilisation in either the mother or the baby; therefore, the plasma testosterone levels were not done in our case.
The ovarian masses differs in size ranging from microscopic to more than 20 cm in diameter.7 In the current case, bilateral ovaries measured 8 cm in dimension. On sectioning, the lesions were well circumscribed and consist of multiple yellowish brown nodules with presence of dark hemorrhagic foci within the masses.2,7 Microscopically, the nodules are made up of cells that are arranged in trabecular or follicular pattern with stromal cell proliferation.
The occurrence of an ovarian tumor presenting during pregnancy seems to be rare with the incidence ranging from 1:815 to 1:2200.10,11 Among these, the incidence of malignancy ranges from 2-8% with arrhenoblastomas, granulosa-theca tumor, Krukenberg tumor, papillary mucinous cystadenocarcinoma and mucinous cystadenocarcinoma were commonly seen during pregnancy.10,11,12 Careful radiological imaging of the ovaries of a pregnant female should be included in the initial examination. Young et al.13 recommended an ultrasound if an enlarged ovary is palpated during an initial pelvic examination. This will determine the size and identify the mass as solid or cystic. The ultrasonographic features of luteoma of pregnancy have been described as that of a solid mass which can be unilateral or bilateral with either single or multiple nodules.5 Because of the solid nature of mass, it is impossible to differentiate it from other solid ovarian neoplasms; for example, luteinized thecoma, granulosa cell tumor or leydig cell tumor based on imaging alone. Bilaterality and multi nodularity are more common in luteomas than in the other ovarian tumors.14
The etiology of pregnancy luteoma remains unclear. It is hypothesized that they arise from stromal cells, which were present before pregnancy and respond in an unusual manner to elevated levels of gonadotropins encountered during pregnancy.5 Luteoma of pregnancy must be differentiated in pregnant females with ovarian masses as recognition of this entity will obviate unnecessary oophorectomy.14 It should be considered in the differential diagnosis of ovarian masses in females who are pregnant or have been recently pregnant.15
In a retrospective study of six patients of pregnancy luteomas, Cronje9 reported that unilateral salpingo-oophorectomy was the most frequent treatment. However, he recommends that the correct treatment is biopsy with conservation of the enlarged ovary, in view of the natural course of the disease. When there is a high clinical suspicion for pregnancy luteoma, clinical monitoring and postpartum radiologic follow-up may be an appropriate management strategy to avoid unnecessary surgery.16
Conclusion
Pregnancy luteoma represents a physiological response during pregnancy and often regresses spontaneously in postpartum period. It must be considered as a part of differential diagnosis of ovarian masses in pregnant or recently pregnant females as recognition of this entity will avoid unnecessary radical surgery.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Sternberg WH. Nonfunctioning ovarian neoplasms. In Grady H G, ed. The ovary. Baltimore: Williams & Wilkins, 1963: 209
2. Garcia-Bunuel R, Berek JS, Woodruff JD. Luteomas of pregnancy. Obstet Gynecol 1975 Apr;45(4):407-414.
3. Lalwani N, Patel S, Ha KY, Shanbhogue AK, Nagar AM, Chintapalli KN, et al. Miscellaneous tumour-like lesions of the ovary: cross-sectional imaging review. Br J Radiol 2012 May;85(1013):477-486.
4. Phelan N, Conway GS. Management of ovarian disease in pregnancy. Best Pract Res Clin Endocrinol Metab 2011 Dec;25(6):985-992.
5. Choi JR, Levine D, Finberg H. Luteoma of pregnancy: sonographic findings in two cases. J Ultrasound Med 2000 Dec;19(12):877-881.
6. Spitzer RF, Wherrett D, Chitayat D, Colgan T, Dodge JE, Salle JL, et al. Maternal luteoma of pregnancy presenting with virilization of the female infant. J Obstet Gynaecol Can 2007 Oct;29(10):835-840.
7. Clement PB. Tumor-like lesions of the ovary associated with pregnancy. Int J Gynecol Pathol 1993 Apr;12(2):108-115.
8. Ugaki H, Enomoto T, Tokugawa Y, Kimura T. Luteoma-induced fetal virilization. J Obstet Gynaecol Res 2009 Oct;35(5):991-993.
9. Cronjé HS. Luteoma of pregnancy. S Afr Med J 1984 Jul;66(2):59-60.
10. Manganiello PD, Adams LV, Harris RD, Ornvold K. Virilization during pregnancy with spontaneous resolution postpartum: a case report and review of the English literature. Obstet Gynecol Surv 1995 May;50(5):404-410.
11. Stedman CM, Kline RC. Intraoperative complications and unexpected pathology at the time of cesarean section. Obstet Gynecol Clin North Am 1988 Dec;15(4):745-769.
12. Ozdegirmenci O, Kayikcioglu F, Haberal A, Ozfuttu A. Krukenberg tumor mimicking pregnancy luteoma. Gynecol Endocrinol 2007;23(8):482-485.
13. Young RH, Dudley AG, Scully RE. Granulosa cell, Sertoli-Leydig cell, and unclassified sex cord-stromal tumors associated with pregnancy: a clinicopathological analysis of thirty-six cases. Gynecol Oncol 1984 Jun;18(2):181-205.
14. Mazza V, Di Monte I, Ceccarelli PL, Rivasi F, Falcinelli C, Forabosco A, et al. Prenatal diagnosis of female pseudohermaphroditism associated with bilateral luteoma of pregnancy: case report. Hum Reprod 2002 Mar;17(3):821-824.
15. Rodriguez M, Harrison TA, Nowacki MR, Saltzman AK. Luteoma of pregnancy presenting with massive ascites and markedly elevated CA 125. Obstet Gynecol 1999 Nov;94(5 Pt 2):854.
16. Masarie K, Katz V, Balderston K. Pregnancy luteomas: clinical presentations and management strategies. Obstet Gynecol Surv 2010 Sep;65(9):575-582.
|