| |
Introduction
In the prevailing view that "There is no health without mental health",1 it becomes imperative to establish the best evidence-based practice psychiatric care. Numerous literatures have indicated the importance of establishing psychiatric services within general, tertiary or teaching hospitals.2-4 The first reason being that specialized psychiatric services have not been forthcoming to cater to the required needs on the ground in many developing countries,5 or emerging economies like Iraq.6 Instead, the priority has been geared towards the control and eradication of communicable diseases.1 What amounts to be such myopic approach persists despite the fact that emotional, cognitive and behavioral disorders which are often framed as non-communicable diseases are outstripping communicable diseases in terms of their negative repercussions to the society, nation and global health.7
The second impetus that comes to the forefront for establishing psychiatric services in general hospitals is derived from the fact that general hospitals are spread in many quarters in developing countries. In Iraq for instance, despite its turbulence, there is an acceptable veneer of general hospitals in all parts of the country with an estimated physician density of 0.7 physicians/1,000 population.8 On the other hand, specialized psychiatric services are few and most are located in areas not accessible for the majority of the population. In the developing countries in general, most of the available psychiatric services are, to say the least, rudimental. Due to the lack of trained professionals, psychiatric hospitals are often perceived as proxy prisons due to their custodial nature.
The third reason is due to specific socio-cultural teachings related to the conception of mental illness, psychiatric services are harboring negative stigma in the eyes of the community.2,9 Many people with mental illness are likely to stay underground or seek traditional healing until their condition becomes advanced and sometimes develop irreversible pathology,7 further adding to the dire situation of mental health in many developing countries.
The fourth reason is that there is evidence suggesting that general hospitals may be more conducive for a situation where psychiatric complaints may co-exist with other medical conditions. Due to logistical reasons, economic or healthcare system, it may sometimes be difficult to refer a client with co-morbidity to a relevant hospital. With stigmatized psychiatric centers in developing countries, finding non-psychiatric physicians to work in available psychiatric centers is an untenable inspiration. Within such background, there is a strong rationale for establishing psychiatric services within a general hospital. Such quest appears to provide the middle ground for those who call for ‘deinstitutionalization’ of psychiatric hospitals on one hand, and those who call for moving mental health services back into the community, on the other hand.5
Despite decades of political unrest, Iraq has made a concerted effort to integrate mental health into primary healthcare.10 Along with such quest, some of the general tertiary care (Baghdad University - College of Medicine), for example, have developed a walk-in psychiatric clinic. The advantage of such clinic being that psychiatric services serve within the convenience of a general hospital. Studies from elsewhere have indicated that such clinics are perceived favorably by the mental health users which enable them to have access and receive prompt consultations at a tertiary level clinic without going through protracted referral formalities.2,11
Most published studies in the Arab parts of the world have focused on liaison facilities, psychiatric patient referrals and psychiatric patients in primary healthcare.12 There is a dearth of information on socio-demographic and clinical characteristics of a walk-in psychiatric clinic in a general hospital. Thus, the present study aims to examine (i) demographic, and (ii) clinical characteristics of the clients seeking consultation at a walk-in psychiatric clinic in a general hospital during the year 2010, as classified by the Diagnostic and Statistical Manual of Mental Disorders Classification Criteria (DSM-IV).13
Methods
For this retrospective study, a detailed structured form was designed to uniformly extract required information from the medical records of patients who registered at the walk-in clinic during the period of 1st January to 31st December 2010. The inclusion criteria consisted of all consecutive attendees seeking psychiatric consultation regardless of whether it was their first visit or they were coming for follow-up. Exclusion criteria included attendees referred for medico-legal purposes or known medical cases referred to the psychiatric unit as part of palliative care. For patients deemed to have fulfilled the inclusion criteria, information was elicited from the medical records of socio-demographic profiles and diagnostic break-up of the patients attending the walk-in psychiatric clinic, Baghdad, during the year 2010. The recorded signs and symptoms were classified according to the DSM-IV.
The study protocol was approved by the local Institutional Review Board (IRB), Research and Ethical Committee, at Medical City Teaching Hospital. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) software (Version 16.0, IBM, Chicago, Illinois, USA). Chi-square analysis was used to evaluate categorical data. The non-parametric Fisher’s exact test (two-tailed) replaced the Chi-square test in case of small sample size where the expected frequency was less than 5 in any of the cells in 2 × 2 tables. A cut off p-value of <0.05 was used for statistical significance.
Results
The present retrospective survey was based on 2,979 attendees to a walk-in psychiatric clinic who fulfilled the inclusion criteria. The attendees included 1,864 (63%) males and 1,115 (37%) females. Table 1 depicts the age group of the attendees, gender, source of referral, place of abode, and occupation. In terms of the source of referral, the majority (n=2600; 87%) were referred themselves to the walk-in clinic or were referred by family. Other sources of referral included other medical subspecialties, emergency department, and civil or military administration. On the whole, the participants who came via means other than themselves or were referred by family constituted less than 6% of the referrals.
In terms of the place of residence, the majority of participants were residents of Baghdad City rather than from the coterminous Baghdad provinces. While in terms of occupation, housewives constituted 24%, and approximately 32% of the studied group was comprised of subjects who were employed (military/police, government employees and private work). The rest were either minors, students or retired, as shown in Table 1.
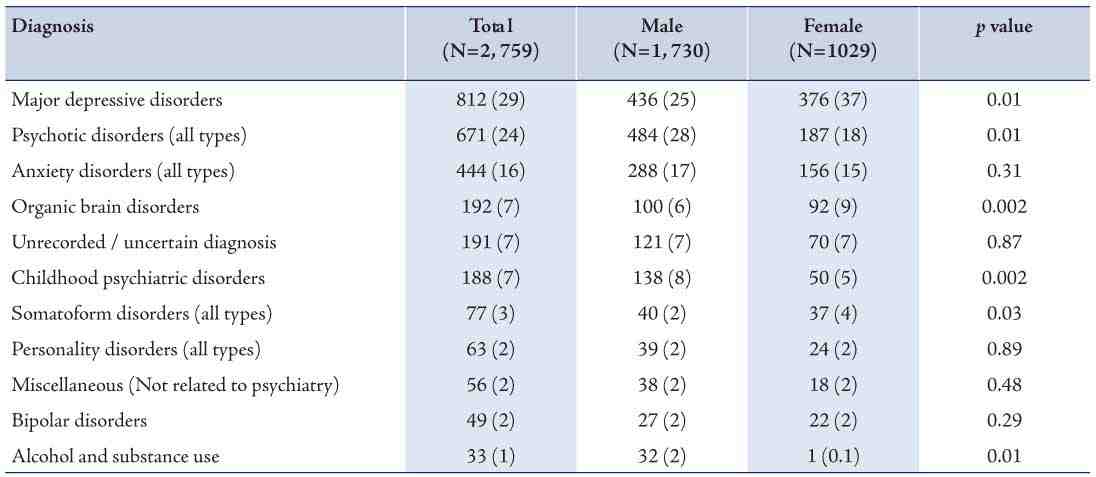
Table 2 shows the DSM-IV diagnoses of the cohort. The most common diagnosis being major depressive disorders (30%), while psychotic disorders (25%) and anxiety disorders (18%) were also strongly expressed. In terms of gender, the predominance for males was significant for both depression and psychotic diagnoses. However, there was no gender difference in terms of diagnosis of anxiety disorders. On the whole, a male gender factor was significant in organic brain disorders, childhood disorders, somatoform disorders, as well as alcohol and substance abuse.
Approximately 7% of the cohort presented with conditions falling under the realm of child and adolescent psychiatric disorders. Organic brain disorders comprised 7% of the studied sample. Less common diagnoses included somatoforms (3%), personality disorders (2%), and the lowest rate was observed for Bipolar disorder (2%). Alcohol and substance use disorders comprised 3% of the total sample, and the rest of the sample (4%) did not qualify to fulfill DSM-IV diagnoses.
Table 1: Socio-demographic profile of patients who attended the walk-in psychiatric clinic in Baghdad (year 2010).
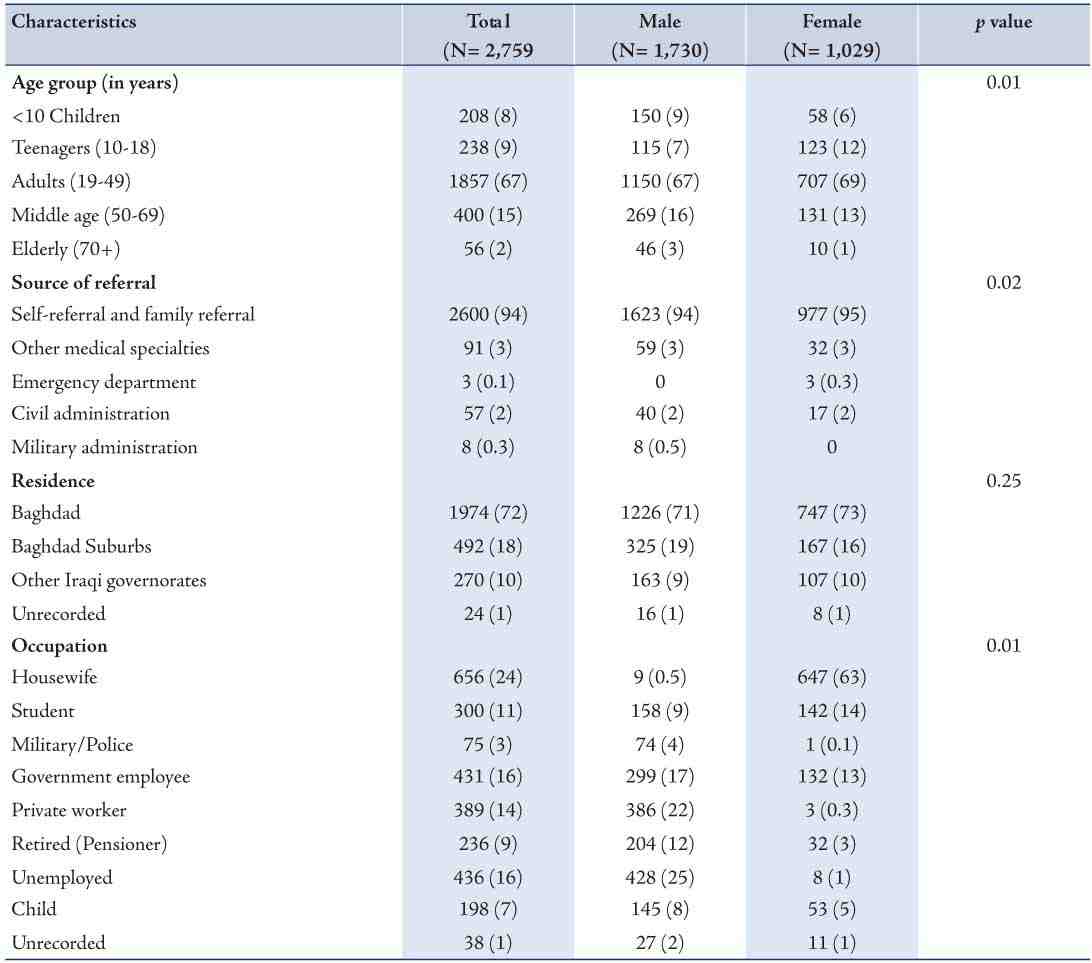
Table 2: Diagnoses of patients who attended the walk-in psychiatric clinic in Baghdad (year 2010).
Discussion
Mental disorders are an important cause of long term disability and dependency.14 Epidemiological surveys and services in Asia have indicated that there are 680 million people who are likely to succumb to vagaries of psychiatric disorder and yet in terms of services, there is one mental health professional per million population.1 The question remains whether people with mental illness seek help and what is the underlying psycho-cultural background that shapes such care seeking.
As it has already been observed, people with mental illnesses, in the Arab world for example, tend to seek help from traditional healers.15 With recent mushrooming of psychiatric hospitals, some people with mental illnesses also seek help from such specialized psychiatric hospitals. In addition to specialized psychiatric services, and complementary and alternative medicine, some walk-in psychiatric clinics have mushroomed in different parts of the Arab world including Iraq. This retrospective study has embarked to depict and point out the observed trends through a socio-cultural perspective to determine the demographic and clinical characteristics of clients seeking consultation from a walk-in psychiatric clinic in the urban region of Iraq, during the year 2010.
One of the main aims of the present study was to establish the demographic characteristics of attendees at the walk-in psychiatric clinic during the study period. First of all, in terms of age, patients aged between 19 and 49 years (adults) presented the majority of the study participants, this trend is similar to what has been noted elsewhere with minor variations due to the difference in the breakdown of age groups. In Fiji, Aghanwa reported that a majority of those seeking psychiatric consultation at the general hospital were in the 16-45 age group.11 However, there is no consensus as to which age group is the most prone to psychiatric disorders. The rates of psychiatric disorders fluctuate according to geographic, ethnic and socioeconomic status.16,17 In the American population, studies have suggested that the onset of mood disorders like depression tend to occur in the early 30s and tends to peak in the age group approaching 50 years.18 Despite such caveat, it is widely accepted that psychiatric disorders often affect young people who are on the midst of their most productive years of life.19
Many studies have highlighted a strong relationship between gender and mental illness, with the female gender being the most prominent of the risk factors in certain psychiatric disorders.18 But emerging situations appear to point to a more complex picture. In reference to the Arab world, Coker has noted that there are no gender gaps in the presentation of mental illness but women are more likely to admit having a mental illness.20 Such tendency is largely absent among males, however, such contention is challenged with clinical observations which show males surpassing their female counterparts in psychiatric consultations.21,22 Speculation indicates that there is a socio-cultural moderator mitigating some forms of mental illnesses among females. This is thought to explain why females tend to admit having a mental illness but are unlikely to seek help or to be seen at the psychiatric clinics. It is possible that perhaps gender segregation and other socio-cultural prescriptions inherent in such paternalistic society may hamper women from venturing outside to ‘spill the family secret’ to the outside world.23 As for the males, being the public front of the family or society are likely to ‘deny’ having mental illness, thus such ‘machismo’ is likely to be eroded once psychiatric distress becomes overwhelming. Being a public front of the family, males with overt, compromised cognitive or emotional functioning are likely to be exposed and therefore breed unwanted ‘shame’. It is not surprising that there is a male predominance in seeking psychiatric care in the Arab world, as the present study implies.
In many traditional communities, mental illnesses are often the prerogative of traditional healing systems. The fact that primary healthcare does not cater to the needs of people with mental illnesses; the first point of contact for them is tertiary care, and it is not surprising therefore, that the majority of Iraqi clients seeking consultation presented themselves at the general hospital or were referred by family. This is consistent with the low observed referrals from other medical specialties. Lower referrals may not only be as a result of a lack of awareness of non-psychiatric physicians, but also on the part of the patients. Many Arab clients are likely to be unsettled if they are referred to a ‘psychiatric doctor’. It is possible that patients may think that a referral to a mental health specialist means that they are "crazy". For these reasons, the majority of referrals (94%) were classified as ‘self and family referrals’.
In the available literature, referral to consultation liaison psychiatry appears to be low as noted in many countries.11,24 Many factors have been attributed to this including an insufficient knowledge of the scope of mental health services in the general hospital and the lack of respect towards the psychiatric field by other physicians.25 This situation is likely to be relevant in the case of the Iraqi population, where like their Arab counterparts, tend to present their psychiatric illness as somatic complaints. Somatic complains are likely to be perceived as medical or neurological conditions. A preponderance of somatic presentation has been vividly captured in a study by Okasha and Demerdash, who reported that sexual inadequacy was reported in the Arab population as backache due to the socio-cultural doctrine that the spine is the repository for sperm and virile.26
The most common diagnosis observed from the present survey was major depressive disorders followed by psychotic disorders and anxiety disorders. Because of recent seismic political stirrings and violence in Iraq, one would expect anxiety disorders such as post-traumatic stress disorder to be common but this was not the case for the present cohort. It is possible that this may be linked to Islamic teachings which have been postulated to "provide some protection against adverse psychological consequences. Muslims believe that God will avenge an injustice that befalls the faithful. Hence, the matter is left to God and the trauma is accepted as divine will" (p. 450).27
The population of Iraq has a predominant ‘youth bulge’ and one would therefore expect child and adolescent mental disorders to be relatively high.28 However, there is no evidence to substantiate such view from this retrospective study, a little speculation is therefore warranted. Globally, it has been estimated that 9-13% of the child and adolescent age group have serious cognitive, emotional and social disturbances.19 This means the society will have to care for such individuals for the rest of their lives. This obviously creates insidious economic and social burden onto the society. The demand for child and adolescent mental health services continue to exceed the supply worldwide.29,30 There is also a severe lack of distribution of such services across countries, particularly in many emerging economies and developing countries. Iraq is no exception, as there appears to be a deficient number of board certified child and adolescent psychiatrists or child clinical psychologists. The situation is also discouraging elsewhere, even in industrialized countries of Western Europe and North America. It has been projected that the world will continue to have a shortfall of child and adolescent mental health practitioners in the foreseeable future.31 It is not clear why there is an under-presentation of children and adolescents at Baghdad’s walk-in psychiatric clinic, but it is usually the caregivers or family and not the child or adolescent who are likely to consult mental health services. Therefore, whether or not children and adolescents seek help from walk-in psychiatric centers not only depends on the nature and severity of the distress, but also on the attitudes and tolerance of the parents. Although child and adolescent mental health services have yet to be developed in many emerging economies like Iraq, there is substantial evidence that mental health services are under-utilized among adolescents and youths.32
It may be worthwhile to highlight some of the obvious limitations of this study; one may stem from a well-known fact that retrospective studies are mediocre, for example, in comparison to prospective studies. The reason being that in retrospective studies, there are no mechanisms to manipulate exposure or outcome measures. Another obvious limitation of this study is the applicability of diagnosis employed being derived from Euro-American populations as concerns have been expressed on the accuracy of such diagnostic tools in capturing distress among non-western societies.33 Studies are therefore needed to explore whether the DSM is applicable to the Iraqi population for reasons which have been discussed elsewhere.34 Also, this study was limited to a walk-in psychiatric clinic as part of a teaching hospital and the fact is that a walk-in clinic might attract a particular group among the population, the generalization of this study should therefore be considered with caution.
Conclusion
This study attempted to examine the demographic, prescribed diagnosis and attendance rates of clients seeking psychiatric consultation at an open walk-in psychiatric clinic in Iraq’s capital, Baghdad. The results indicated the predominance of employed males, aged between 19 and 49 years who are residents of Baghdad City. The majority of the clinic’s attendees were most commonly diagnosed with depression and psychosis.
Acknowledgements
We wish to thank the authority of Medical City, Baghdad University College of Medicine for their support in carrying out this study. SA is a member of the World Health Organization Expert Consultation Group on Feeding and Eating Disorders, reporting to the International Advisory Group for the Revision of ICD-10 Mental and Behavioral Disorders. The views expressed in this article are those of the authors, and not the official policies or positions of the Consultation Group, the Advisory Group, or of the World Health Organization. As for the other authors, there are no conflicts of interest to declare. The study received no financial support for the research and/or authorship.
References
1. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet 2007 Sep;370(9590):859-877.
2. Chand P, Murthy P, Arunachalam V, Naveen Kumar C, Isaac M. Service utilization in a tertiary psychiatric care setting in South India. Asian J Psychiatr 2010 Dec;3(4):222-226.
3. Killaspy H, Banerjee S, King M, Lloyd M. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry 2000 Feb;176:160-165.
4. Al-Habeeb TA. A comparison of psychiatric referrals within the teaching hospital with those from primary care and general hospitals in saudi arabia. J Family Community Med 2002 Sep;9(3):57-65.
5. Patel V, Jenkins R, Lund C. the PLoS Medicine Editors. Putting Evidence into Practice: The PLoS Medicine Series on Global Mental Health Practice. PLoS Med 2012 May;9(5):e1001226 .
6. Sadik S, Al-Jadiry AM. Mental health services in Iraq, Past, Present and future. Integr Psychiatry 2006 Oct;3(4):11-13.
7. Bass JK, Bornemann TH, Burkey M, Chehil S, Chen L, Copeland JR, et al. A United Nations General Assembly Special Session for mental, neurological, and substance use disorders: the time has come. PLoS Med 2012 Jan;9(1):e1001159.
8. Central Intelligence Agency. Iraq. World Factbook. Accessed on June 24, 2013 https://www.cia.gov/library/publications/the-world-factbook/geos/iz.html
9. Skuse DH. Attitudes to the psychiatric outpatient clinic. Br Med J 1975 Aug;3(5981):469-471.
10. Sadik S, Abdulrahman S, Bradley M, Jenkins R. Integrating mental health into primary health care in Iraq. Ment Health Fam Med 2011 Mar;8(1):39-49.
11. Aghanwa H. Consultation-liason psychiatry in Fiji. Pac Health Dialog 2002 Mar;9(1):21-28.
12. Qureshi NA, van der Molen HT, Schmidt HG, Al-Habeeb TA, Magzoub ME. Criteria for a good referral system for psychiatric patients: the view from Saudi Arabia. East Mediterr Health J 2009 Nov-Dec;15(6):1580-1595.
13. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR; Washington DC, American Psychiatric Publishing, Inc, 2000.
14. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006 Nov;3(11):e442.
15. Al-Adawi S, Dorvlo AS, Al-Ismaily SS, Al-Ghafry DA, Al-Noobi BZ, Al-Salmi A, et al. Perception of and attitude towards mental illness in Oman. Int J Soc Psychiatry 2002 Dec;48(4):305-317.
16. Al-Adawi S, Jaju SS, Al-Zakwani I, Dorvlo AS. Culture to Culture Fatphobia and somatization. In: V. R. Preedy, R. R. Watson, C. R. Martin (Eds.), International Handbook of Behavior, Diet, and Nutrition. New York: Springer, pp. 1457- 1473, 2011.
17. Ghaleiha A, Afzali S, Bazyar M, Khorsand F, Torabian S. Characteristics of hospitalized patients following suicide attempt in hamadan district, iran. Oman Med J 2012 Jul;27(4):304-309.
18. Rosenfield S. Gender and mental health: Do women have more psychopathology, men more, or both the same (and why)? In, Horwitz, Allan V. (Ed); Scheid, Teresa L. (Ed), A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York, NY, US: Cambridge University Press, pp.348-360. 1999.
19. Jaju S, Al-Adawi S, Al-Kharusi H, Morsi M, Al-Riyami A. Prevalence and age-of-onset distributions of DSM IV mental disorders and their severity among school going Omani adolescents and youths: WMH-CIDI findings. Child Adolesc Psychiatry Ment Health. 2009 Sept; 26: 3(1):29.
20. Coker EM. Selfhood and social distance: toward a cultural understanding of psychiatric stigma in Egypt. Soc Sci Med 2005 Sep;61(5):920-930.
21. Eloul L, Ambusaidi A, Al-Adawi S. Silent Epidemic of Depression in Women in the Middle East and North Africa Region: Emerging tribulation or fallacy? Sultan Qaboos Univ Med J 2009 Apr;9(1):5-15.
22. Katz G, Grunhaus L, Deeb S, Shufman E, Bar-Hamburger R, Durst R. A comparative study of Arab and Jewish patients admitted for psychiatric hospitalization in Jerusalem: the demographic, psychopathologic aspects, and the drug abuse comorbidity. Compr Psychiatry 2012 Aug;53(6):850-853.
23. Baker KA, Dwairy M. Cultural norms versus state law in treating incest: a suggested model for Arab families. Child Abuse Negl 2003 Jan;27(1):109-123.
24. Vythilingum B, Chiliza B. Consultation liaison psychiatry in Africa – essential service or unaffordable luxury? Afr J Psychiatry (Johannesbg) 2011 Sep;14(4):257.
25. Yamada K, Hosoda M, Nakashima S, Furuta K, Awata S: Psychiatric diagnosis in the elderly referred to a consultation-liaison psychiatry service in a general geriatric hospital in Japan. Geriatr Gerontol Int 2012 Apr; 12(2): 304-30 9.
26. Okasha A, Demerdash, A: An Arabic study of cases of functional sexual inadequacy. Br J Psychiatry 1975 May; 126: 126:446.
27. Shoeb M, Weinstein H, Mollica R. The Harvard trauma questionnaire: adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. Int J Soc Psychiatry 2007 Sep;53(5):447-463.
28. AlObaidi AK, Budosan B, Jeffrey L. Child and adolescent mental health in Iraq: current situation and scope for promotion of child and adolescent mental health policy. Intervention (Amstelveen) 2010 Mar;8:40-51 .
29. Thomas CR, Holzer CE III. The continuing shortage of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry 2006 Sep;45(9):1023-1031.
30. Al-Farsi YM, Waly MI, Al-Sharbati MM, Al-Shafaee M, Al-Farsi O, Al-Fahdi S, et al. Variation in socio-economic burden for caring of children with autism spectrum disorder in oman: caregiver perspectives. J Autism Dev Disord 2013 May;43(5):1214-1221.
31. Beresin EV, Balon R, Coverdale JH, Roberts LW. Challenges in child and adolescent psychiatric education. Acad Psychiatry 2012 Nov;36(6):429-432.
32. Al Riyami AA, Al Adawi SH, Al Kharusi HA, Morsi MM, Jaju SS. Health services utilization by school going Omani adolescents and youths with DSM IV mental disorders and barriers to service use. Int J Ment Health Syst 2009 Sept;25:3(1):22.
33. Al-Adawi S, Dorvlo AS, Viernes N, Alexander PC, Al-Zakwani I. Is the Diagnostic Prototype for Anorexia Nervosa Universal? Evidence from the Middle East and Implications for ICD-11. Arab J Psychiatry 2012 May;23(1):42-51.
34. Kleinman A. Suffering, ethics, and the politics of moral life. Cult Med Psychiatry 1996 Sep;20(3):287-290.
|
|