|
Introduction
Breast cancer is the most common malignancy in women throughout the world. It accounts for 18% of all female cancers and approximately 600,000 annual deaths worldwide.1 Among Omani women, breast cancer is the most common cancer accounting for one in every five new cases of cancer detected among females, with an age standardization incidence rate (ASR) of 11 per 100,000.2 Even though the incidence is increasing in Oman, it remains low compared to Western countries, but is consistent with other Asian countries.
The patient in our study presented with breast cancer and was discovered to have humeral head metastasis during initial workup. The dilemma was encountered in investigating the modality of confirming humeral head metastasis, since there are many common differential diagnoses that can present with the same findings for example: cervical radiculopathy, brachial plexopathy, neuropathy, rotator cuff tendonitis, adhesive capsulitis, and epicondylitis.
Case Report
A 46-year-old female presented at the One Stop outpatient Breast Clinic at Sultan Qaboos University Hospital (SQUH), with a history of right breast lump for the past 6 months which was painless and not associated with nipple discharge. She had no previous history of breast disease. She experienced menarche at the age of 12 years and has had regular cyclical periods. She had her first child at the age of 21 years, and has 5 children in total who were all breastfed. There was no history of oral contraceptive use and she had no family history of breast cancer but her mother was diagnosed with uterine cancer. She also complained of right shoulder pain for the last 2 months.
On examination, the left breast and axilla were grossly normal. However, in the right breast, there was an obvious palpable lump in the upper outer quadrant (UOQ) measuring approximately 5 × 4 cm, which was ill-defined and mobile. There were also multiple enlarged and mobile axillary lymph nodes. Neck examination was grossly normal. Examination of the right shoulder showed intact distal neurovascular state with limitation of abduction to 110 degrees and external rotation to 40 degrees. The left shoulder was normal. Breast imaging, including mammogram and ultrasound were reported as BIRADS V (Fig. 1), consistent with multifocal multicentric malignant masses with pathological axillary lymph nodes.
FNA of the largest mass in the right breast was performed which showed atypical cells dispersed singly and in clusters with a mucinous background. Tru-cut biopsy showed a grade 1 infiltrating ductal carcinoma with mucinous features. The tumor was formed of cohesive sheets as well as cluster and cords of mild to moderately pleomorphic cells in mucin pools and also infiltrating desmoplastic stroma. An associated solid low-grade ductal carcinoma in situ (DCIS) was present. Lymph vascular invasion was also seen. The tumor cells were positive for estrogen receptor (ER) and progesterone receptor (PR), and negative for HER-2/neu.
Her staging workup which included CT chest, abdomen and pelvis were all normal except for a lytic lesion seen in the right humeral head (Fig. 4). However, the Bone Scan static (Dose of HMDP: 700 MBq), showed very high uptake in the right shoulder with no other abnormal uptake noted in the rest of the body. (Fig. 5)
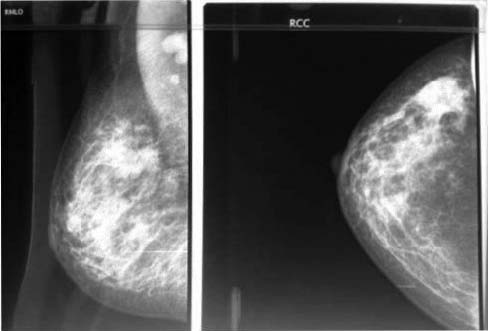
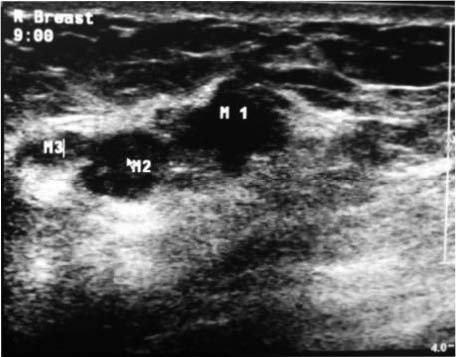
Figure 1: Mammogram and Ultra sound Breast.
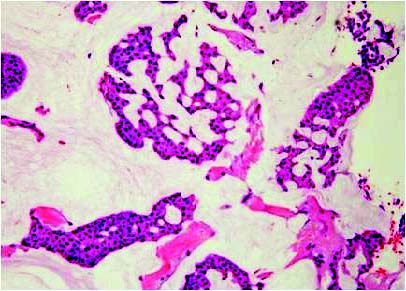
Figure 2: Mucinous areas within the tumor showing nests of tumor cells suspended in pools of extracellular mucin.
She was further investigated with shoulder MRI and PET scan which confirmed the findings of metastasis to the right humeral head. After discussion in a Multidisciplinary Team (MDT) meeting for breast cancer, it was decided to treat her with 6 cycles of neoadjuvant chemotherapy based on Adriamycin and docetaxel regimen. An orthopedic surgeon expert in shoulder joint advised not to intervene for the time being. The patient had a good response following neoadjuvant chemotherapy and showed a very good response with post chemo restaging CT scan showing lesion confined to breast and axilla only with well healed humeral lesion. (Fig. 6)
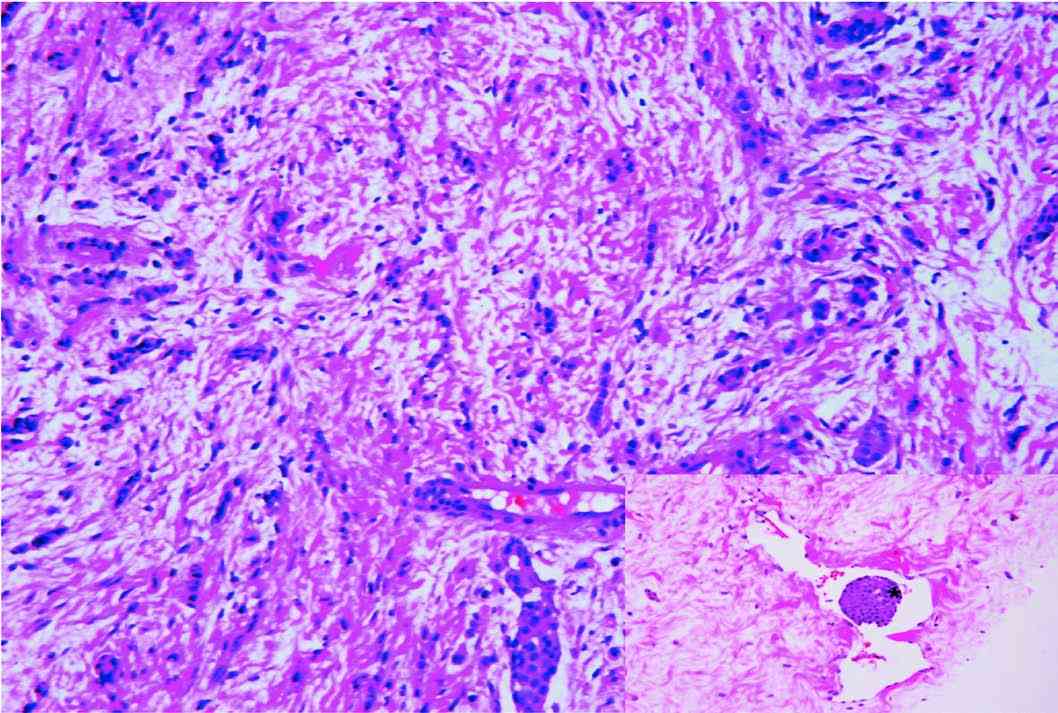
Figure 3: Areas of more conventional ductal carcinoma, no special type formed of infiltrating cords of tumor cells. Tumor embolus in a small lymphatic channel.
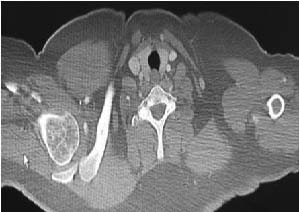
Figure 4: CT scan showing a lytic lesion in her right humeral head.
The patient later underwent right modified radical mastectomy with level I, II, and III axillary clearance. The subsequent histopathology revealed 6 × 4 × 2.5 cm mucinous carcinoma grade 1 with no evidence of regression post chemotherapy with low grade DCIS. There was no lymphovascular invasion or perineural invasion seen. There were tumor deposits seen in 7 out of 12 axillary nodes from levels I and II, while no tumor deposit was seen from a single level III axillary node. The immunohistochemistry was strongly positive for estrogen receptor while intermediate positive for progesterone receptor; however, HER2 status was negative as confirmed on fluorescence in situ hybridization (FISH). Ki67 index showed occasional proliferation. Deep and inferior margins showed tumor with 2 mm and 1 mm clearance, respectively. She was started on hormonal treatment and had completed 25 sessions of 45 Gy radiotherapy to her right shoulder, chest wall and supraclavicular fossa regions. She was recently seen at the Breast and Oncology Clinic with no active complaints and was doing well with improvement of right shoulder abduction. Informed consent was obtained from the patient for publication of this case report and all accompanying radiographic images.
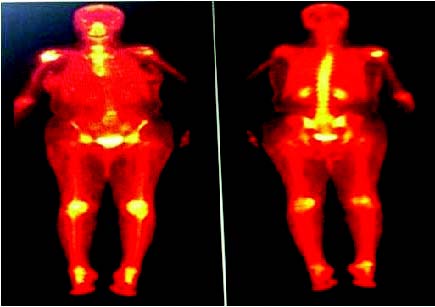
Figure 5: Static bone scan showing high uptake in right humeral head.
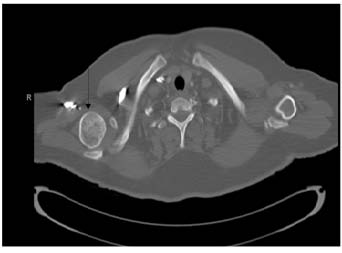
Figure 6: Post chemo CT with arrow pointing on well healed humoral head.
Discussion
Breast cancer is the most common site of origin of metastatic deposits in the skeleton as well as the most common site of recurrence of breast cancer. As much as half of all pathological fractures are due to breast cancer.3 Cervical radiculopathy, brachial plexopathy, neuropathy, rotator cuff tendonitis, adhesive capsulitis, epicondylitis, post-mastectomy syndrome, swelling, and bone metastases are among the common disorders responsible for upper-extremity pain in breast cancer patients.4 Metastasis to the bone arises in 20% to 60% of patients and in up to 70% to 85% at autopsy. More than 69% of these patients have a solitary recurrence confined to a single anatomic site, and 12% have multiple metastatic sites. However, only 3.5% of breast cancer patients develop long-bone metastases, and of those, 88% experience recurrence in the femur. When the humerus is involved, almost 90% of lesions arise in the proximal (42%) and diaphyseal (47%) regions. Metastases to the distal humerus are more infrequent, accounting for only 11% of cases.5
Tumors of the coracoids process are rare. We could only identify one report of a metastatic lesion to the coracoid using a PubMed search of the literature. The propensity of breast cancer to metastasize to bone is not clearly understood. Batson described the valveless venous plexus commonly thought to contribute to the spread of breast and prostate carcinoma to sites in the axial and appendicular skeleton. More recently, studies suggest some of the mechanisms for bone destruction once tumor cells have gained access to a distant site. These include osteoclast activating factors such as parathyroid hormone-related protein (PTH-rP), tumor necrosis factor (TNF) α and ß, epidermal growth factor (EGF), and prostaglandins. These changes to the bone architecture lead to structural weakness, and typically, the radiographic appearance of breast metastases to bone is one of mixed osteoblastic and osteolytic appearance.6
Although the prognosis for patients with breast cancer that has spread to the bone was poor in the past, nowadays these patients are living much longer and feeling much better due to dramatic improvements in medical and surgical treatments. Two of three patients with metastasis from breast cancer will need surgery, radiation, or medical therapy for complications due to bone metastasis.3 There are several effective ways to treat breast cancer that has metastasized to the bone. The treatment used is tailored to the needs of each patient. If the cancer has spread to bone in only one spot, radiation may be given to treat the bone. In general, this will relieve the pain and prevent fractures at this site. If breast cancer has spread to several places in the bones, radiation treatment to all of the sites may not be possible because of limitations in the total amount of radiation that can be given safely. In this case, the patient may be given anticancer therapy with hormonal treatment or chemotherapy. Patients whose breast cancer has spread to bone may be given bisphosphonate drugs such as Aredia and Zometa to help slow or stop the cancer from destroying bone tissue. Prophylactic surgical fixation of impending pathologic fractures is indicated if a patient remains symptomatic despite nonsurgical treatment or if the upper extremity is needed for weight bearing. Judicious bracing may reduce risk of fracture and allow for non-weight bearing functional activities in selected cases.4
Conclusion
Breast cancer can affect bone in two ways: it can metastasize to bone, while in addition, breast cancer treatment can cause rapid bone loss. Breast cancer metastasis most commonly affects the spine, ribs, pelvis, and proximal long bones. The humerus is the most common upper extremity site for bony metastasis, and pathologic fractures can result. It is important to have a high degree of clinical suspicion for metastasis when musculoskeletal pain occurs in breast cancer patients so that early investigations like MRI and PET can be ordered to make a definitive diagnosis.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Kumar S, Burney IA, Al-Ajmi A, Al-Moundhri MS. Changing trends of breast cancer survival in sultanate of oman. J Oncol. 2011;2011:316243. doi:10.1155/2011/316243. Accessed on 20th March 2013.
2. Ministry of Health Sultanate of Oman. Cancer incidence in Oman. Muscat: Ministry of Health Sultanate of Oman; 2010.
3. Cashman JL III. Metastatic Breast Cancer, American academy of orthopedic surgeons 2011. http://orthodoc.aaos.org/jlcashmanmd
4. Stubblefield MD, Custodio CM. Upper-extremity pain disorders in breast cancer. Arch Phys Med Rehabil 2006 Mar;87(3)(Suppl 1):S96-S99, quiz S100-S101.
5. Fan G, Sinclair E, Christakis M. Solitary bone metastasis beneath the shoulder shield: coincidence or cause? Current oncology Vol 13(4): 1-4. http://www.current-oncology.com/index.php/oncology/article/download/98/66.
6. Benson EC, Drosdowech DS. Metastatic breast carcinoma of the coracoid process: two case reports. J Orthop Surg Res 2010;5:22. . Accessed 20th Mar 2013.
|