| |
Abstract
Objectives: The aim of this study was to test the association between quality of sleep and stress in individuals with TMD (temporomandibular joint dysfunction) in simulated Mars mission.
Methods: The 24 healthy crew members were recruited. The physiological measures of systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were recorded. The Symptom Checklist-90-revised was used which was based on nine dimensions of psychological functioning. The Multidimensional Pain Inventory was pain severity, social and physical activities, affective distress, social support, and feelings of life control. The Pittsburgh Sleep Quality Index was used to measure the number of hours spent in bed and during asleep, frequency and reasons for awakening, and difficulty returning to sleep after awakening. The orofacial pain questionnaire was applied to measure pain experience using descriptors from the McGill Pain Questionnaire. Salivary cortisol and melatonin were measured.
Results: The 15 crew members reported temporomandibular joint pain after 6 days of mission. On dental examination, 5 crew members reported simple muscle pain (SM) and other 10 crew members with TMD. The TMD group endorsed more affective descriptors of their pain experience. Compared to the TMD group, the SM group also reported significantly poorer sleep duration. The TMD group reported nonsignificantly more daytime dysfunction than the control. Higher levels of salivary cortisol and salivary melatonin were reported in the TMD group as compared to other group.
Conclusion: This study concludes that both quality of sleep and stress levels due to extreme condition (simulated Mars mission) were associated with TMD in simulated Mars mission.
Keywords: Temporomandibular joint dysfunction; Sleep; Stress; Mars mission; Simulated.
Introduction
Human physiological adaptation to the conditions of space is a challenge faced in the development of human spaceflight.1 A roundtrip to Mars with current technology is estimated to involve at least 18 months in transit alone.2 How the human body reacts to such time periods in space is a vital part of the preparation for such journeys. Astronauts will encounter both physiological and psychological extremes during the journey while on the Mars terrain, and the return to Earth. Exposure to microgravity and the space environment during short- and long-duration space missions has important medical and health implications in astronauts. These include neuro-vestibular problems involving space motion sickness, disorientation during flight, and impaired balance and neuromuscular coordination after landing; cardiovascular and fluid-related problems related to orthostatic hypotension, ventricular arrhythmias and reduced cardiac muscle mass and diminished cardiac function; muscle-related problems of atrophy involving loss of muscle mass, circadian rhythm-related problems involving sleep and performance; immune-related problems involving infections and immunodeficiency, and psychological factors.1-4 Very few studies were published on effect of microgravity and extreme condition on oral cavity.5 Temporomandibular joint dysfunction (TMD) consists of a series of clinical signs and symptoms involving the temporomandibular joint (TMJ) and/or masticatory muscles, with pain being the most frequent symptom. Several etiological factors including sleep disorders as well as physical, emotional, and occlusal stress may decrease the adaptive capacity of the stomatognathic system and lead to the occurrence of the disorder.6 To the best of our knowledge, no study was published on effect of extreme environment due to simulated Mars mission on tempromandibular joint. The aim of this study was to test the association between quality of sleep and stress in individuals with TMD (temporomandibular joint dysfunction) in simulated Mars mission.
Methods
The 24-crew members were recruited from Simulated Mars mission at MDRS (Mars Desert Research Station). The crew members were aged 20-26 (23.6 [2.4]) years. The average of calorie and calcium intake of the crew members during mission were 2400 kcal/day (range 2090-3200 kcal/day) and 1267 mg/day (1130-1400 mg/day), respectively. Dietary sodium and potassium intake were maintained at 98 (80-103) and 86 (75-120) mmol/day, respectively. Water intake was ad libitum 1236(68) mL/day). Temporomandibular joint examinations were done by clinical examination every day (8:00-9:00 am) during the 14 days of mission and next day after finished mission.
Clinical criteria of temporomandibular joint dysfunction as follows:
1. Biting or chewing difficulty or discomfort.
2. Clicking sound while chewing or opening the mouth.
3. Mild to moderate aching pain in the face.
4. Discordant sensation while chewing.
5. Headache.
6. Jaw pain or tenderness of the jaw.
7. Reduced mouth opening.
The orofacial pain examination began with a detailed history of the subject’s chief complaint(s), associated symptoms, TMJ noise, mandibular dysfunction, parafunctional habits, past facial trauma, past medical history, family medical history, previous treatments/consultations for their chief complaint(s), previous and present medications for their chief complaint(s), as well as their psychosocial history. The subsequent physical examination included measurements of vital signs, cranial nerve examination, cervical and mandibular range of movements with notation of associated pain, TMJ palpation and auscultation, cervical and masticatory muscle palpation with notation of associated pain and/or presence of myofascial trigger points, and intraoral examination. The examinations were conducted by dentists with advanced training in the diagnosis of orofacial pain conditions. For those subjects with some degree of TMD, the following questionnaires were further applied. The physiological measures of systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were recorded using a Paramed 9200 automated blood pressure cuff. The cuff was placed on the patient’s left arm. The Symptom Checklist-90-Revised (SCL-90-R) was used based on nine dimensions of psychological functioning, including somatization (SOM), obsessive-compulsive behavior (OC), interpersonal sensitivity (IS), depression (DEP), anxiety (ANX), hostility (HOS), phobic anxiety (PHOB), paranoid ideation (PAR), and psychoticism (PSY). Test-retest reliabilities ranged from r=0.78 to 0.90 for normal samples, and internal consistencies ranged from 0.77 to 0.90. The Multidimensional Pain Inventory (MPI) was pain severity, social and physical activities, affective distress, social support, and feelings of life control.7 The Pittsburg Sleep Quality Index (PSQI) was used to measure the number of hours spent in bed and asleep, frequency and reasons for awakening, and difficulty returning to sleep after awakening.8 The orofacial pain questionnaire was applied to measure pain experience using descriptors from the McGill Pain Questionnaire.9 Saliva samples were collected immediately before and after sleep every day. The samples were immediately frozen at -4C, centrifuged and analyzed for biomarkers. Salivary cortisol (by means of Salimetrics Inc., PA, USA) and melatonin (by means of Alpco Diagnostics, NH, USA) were measured. Data were analyzed using SPSS, version 11 (SPSS, Chicago, IL, USA).
Results
The 15 crew members reported TMJ pain after 6 days of mission. On dental examination, 5 crew member reported simple muscle pain (SM) and other 10 crew members reported TMD. We divided the subjects into three groups such as TMD (10), SM (5) and control (9). The sums of the number of affective descriptors and sensory descriptors endorsed by each crew members were calculated and a comparison was made between the groups. The TMD group endorsed more affective descriptors of their pain experience (M [Mean]=0.87, SD=1.2) than the SM group (M=0.45, SD=0.56), p<0.05. When subjects’ psychological symptoms were compared, there were statistically nonsignificant differences between the three groups on four of the nine dimensions of the SCL-90-R (somatization, obsessive-compulsive, depression, and anxiety) (Table 1).
Table 1: SCL-90-R symptom dimension means and standard deviations.
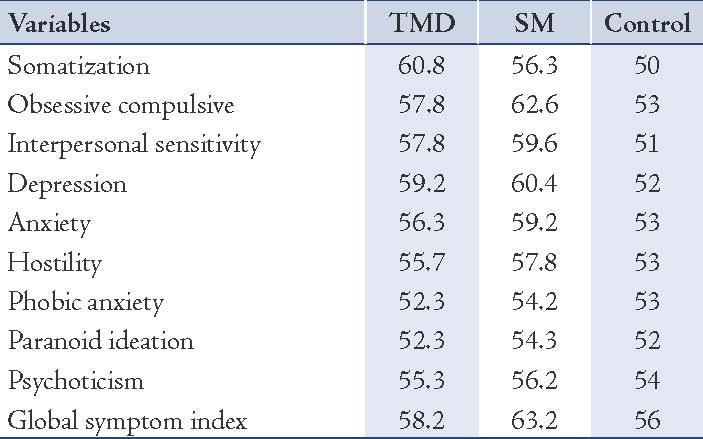
Table 2: PSQI in three groups.
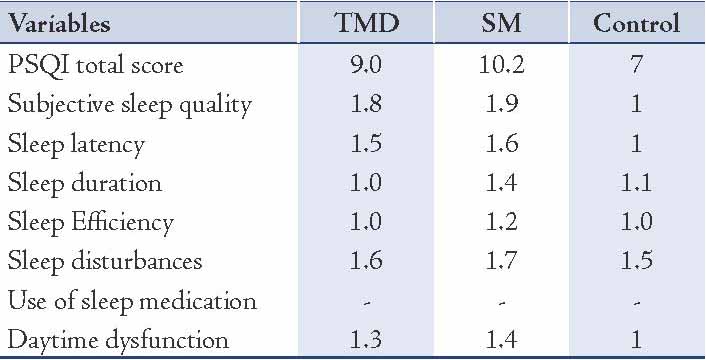
There were nonsignificant differences between the three groups on the life interference and life control subscales of the MPI. The TMD and the SM groups reported significantly more daytime dysfunction than control group. Compared to the TMD group, the SM group also reported significantly poorer sleep duration. The TMD group reported nonsignificantly more daytime dysfunction than the control. There were no other significant differences between the groups on the PSQI scores (Table 2). There were nonsignificant difference found between the three diagnostic groups for SBP (TMD group: 132; SM group: M=130; control group: M=128), DBP (TMD group: M=74; SM group: M=72; control group: M=70), or HR (TMD group: M=79.6; SM group: M=74; control group: M=72). There were nonsignificant difference found between the three diagnostic groups for salivary cortisol (TMD group: before and after sleep 3.9 and 4.4 ng/mL; SM group: before and after sleep 3.2 and 4.2 ng/mL; control group: before and after sleep 3 and 4 ng/mL), or salivary melatonin (TMD group: before and after sleep 4.8 and 7.2 ng/mL; SM group: before and after sleep 4.2 and 6.4 ng/mL; control group: before and after sleep 2.8 and 5.2 ng/mL).
Discussion
It has been reported that high workload, international environment (different cultures, different languages, and different habits), isolated, limited internet access, constrict food diet and limited resources lead to stress in simulated Mars mission.10 The risks associated with a Mars mission may be defined as the provisional probability of an adverse event occurring from exposure to the space environment. Particularly, they are the elements that will affect human performances and well-being during a mission. These include the physical environments in which the crew is required to perform operations, and as described above, it is known that the human physiological status will change in response to microgravity, radiations, isolated, international and limited resources in particular known as extreme conditions.1-4
The present study revealed higher levels of psychological distress among TMD and SM groups than among the control on most psychological domains. Our findings are generally consistent with the results of previous study reporting, the lowered levels of psychological distress in TMJ pain as compared to muscle pain in crew members.11 In our study, samples of subjects, quality of sleep, and stress levels were associated with TMD, and a relationship was found between the stress scores, salivary cortisol and melatonin levels and the presence or absence of sleep disorders. Sleep disorders measured by PSQI score indicates that subject is with sleep problems. Temporomandibular disorder (TMD) is a common stress-related condition which is associated with dysregulation of cortical and melatonin secretion. Increased activation of the stress hormone axis by conscious pain perception is a likely explanation, but the magnitude of the increase could indicate that pain in the facial region acts as a greater stimulus than pain elsewhere in the body.11 TMDs have multifactorial etiologies with observed associations with sleep disorders and stress due to extreme condition during simulated Mars mission.12 Previous studies have reported a strong association between sleep disorders and certain types of stress.11,12 Sleep disorders cause an increase in levels of traditional markers of stress and other markers, such as salivary cortisol and melatonin, heart rate and exacerbate the effects of stress as reported in previous studies.11-13 Early morning responses in salivary cortisol excretion profiles have been used in the determination of stress-related adaptation. An enhanced cortisol awakening response is associated with an increased level of stress.12,13 Salivary melatonin and cortisol may serve as an indicator of a biomarker of circadian dysregulation and stress.12
The present study has some limitations. As it was conducted for a small sample size, it does not confirm the absence or presence and degree of TMD, and also, the type of TMD was not diagnosed. In addition, no imaging was used to confirm the diagnosis of TMD or simple pain. Within the limitations of this study, quality of sleep and stress levels due to extreme conditions were associated with TMD in this sample. These data raise the possibility that target factors thought to drive primary insomnia, such as psychophysiology arousal, in addition to improve sleep continuity and administration of melatonin may enhance the efficacy of treatments for TMD and other idiopathic pain disorders and possibly have prophylactic benefits. Melatonin therapy might help in mitigation of sleep, stress and TMD problem in earth, space as well as extreme conditions.
Conclusion
As this study has limitations, quality of sleep and stress levels due to extreme conditions might be associated with TMD in this sample. Furthermore, improve sleep continuity and proper rest might enhance the efficacy of treatments and management for TMD.
Acknowledgements
We would like to express gratitude towards the Mars Society, ILEWG Euro Moon Mars field research programme, ESA/ESTEC, L’Ecole de L’Air, Dr. Guy Pignolet from the SALM institute, Dr. Carol Stoker (NASA Ames), the Mission Support, Mr. Don Lusko, Prof. Bernard H. Foing, and all other related people for their daily assistance and our remote supporters from America, Europe, Canada, and JBR research group India. We are especially thankful to JBR group for providing us funding.
References
1. Paloski WH, Black FO, Reschke MF, Calkins DS, Shupert C. Vestibular ataxia following shuttle flights: effects of microgravity on otolith-mediated sensorimotor control of posture. Am J Otol 1993 Jan;14(1):9-17.
2. Buckey JC Jr, Lane LD, Levine BD, Watenpaugh DE, Wright SJ, Moore WE, et al. Orthostatic intolerance after spaceflight. J Appl Physiol 1996 Jul;81(1):7-18.
3. Baldwin KM, White TP, Arnaud SB, Edgerton VR, Kraemer WJ, Kram R, et al. Musculoskeletal adaptations to weightlessness and development of effective countermeasures. Med Sci Sports Exerc 1996 Oct;28(10):1247-1253.
4. White RJ, Averner M. Humans in space. Nature 2001 Feb;409(6823):1115-1118.
5. Rai B, Kaur J. The history and importance of aeronautic dentistry. J Oral Sci 2011 Jun;53(2):143-146.
6. Ahlberg K, Ahlberg J, Könönen M, Alakuijala A, Partinen M, Savolainen A. Perceived orofacial pain and its associations with reported bruxism and insomnia symptoms in media personnel with or without irregular shift work. Acta Odontol Scand 2005 Aug;63(4):213-217.
7. Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985 Dec;23(4):345-356.
8. Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 1998 Jul;45(1):5-13.
9. Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain 1975 Sep;1(3):277-299.
10. Rai B, Foing BH, Kaur J. Working hours, sleep, salivary cortisol, fatigue and neuro-behavior during Mars analog mission: five crews study. Neurosci Lett 2012 May;516(2):177-181.
11. Korszun A, Young EA, Singer K, Carlson NE, Brown MB, Crofford L. Basal circadian cortisol secretion in women with temporomandibular disorders. J Dent Res 2002 Apr;81(4):279-283.
12. Rai B, Kaur J. Grieofa MO, Foing BH. JBR study of human factors in Mars Analogue: MDRS crew 100 ILEWG EuroMoonMars Crew.62nd International Astronautical Congress, Cape Town, South Africa 3-7 october 2011; IAC-11.A1.4.16.
13. Mongini F, Ciccone G, Ibertis F, Negro C. Personality characteristics and accompanying symptoms in temporomandibular joint dysfunction, headache, and facial pain. J Orofac Pain 2000;14(1):52-58.
|
|