|
Abstract
Objective: The aim of this study is to compare the neonatal outcomes of monochorionic and dichorionic twin pregnancies.
Methods: A retrospective cohort study involving 51 twin pregnancies followed and delivered at Sultan Qaboos University Hospital was conducted between January 2006 and December 2011.
Result: Thirty six (71%) pregnancies were dichorionic diamniotic (DCDA), 14 (27%) were monochorionic diamniotic (MCDA), and one (2%) was monochorionic monoamniotic (MCMA). The antepartum complications noted in the 15 monochorionic twins were discordant fetal growth in 2 (14%) cases, low birth weight in 11 (73%) babies, pre-eclampsia in three mothers (21%) and twin to twin transfusion syndrome in four (29%) cases. Fetal respiratory distress affected eight (57%) of the pregnancies. Six (40%) twin sets were delivered before 30 weeks, 4 (27%) sets at 31 to 32 weeks, 2 (13%) sets at 34-35 weeks, 2 (13%) sets at 36-37 weeks, and 1 (7%) at 37-38 weeks. Fifteen mothers delivered 16 live infants, 9 (30%) stillbirths and 5 (17%) died after birth. Most neonatal deaths were due to neonatal sepsis and pulmonary hypoplasia. Dichorioinic twins, (DC) morbidity was seen in 11% and 40% for monochoroinic twins (MC). Mortality rate was 17% for DC and 47% for MC twins.
Conclusions: Perinatal morbidity and mortality remain high among monochorionic twins. This is likely due to frequent twin-to-twin transfusion syndrome, prematurity, fetal growth restriction and intrauterine fetal death. Improved fetal and neonatal management may result in improved outcomes.
Keywords: Twins; Monochorionic; Dichorionic, Outcome.
Introduction
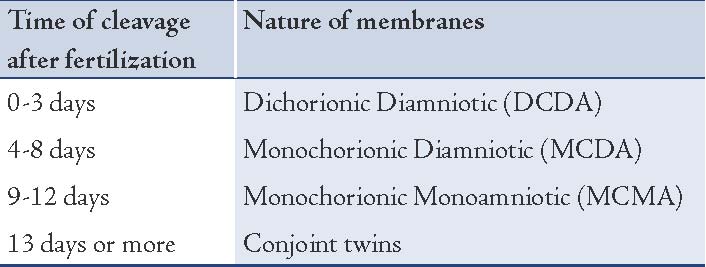
There are two types of twins: dizygotic and monozygotic twins. Approximately two thirds of twins are dizygotic and they result from fertilization of two or more eggs by different spermatozoa, with an incidence of 7 to 11 per 1000 births. The second type of twins is monozygotic, which results from the splitting of the zygote at various stages of development with an incidence of 3 to 4 per 1000 births.1 Different types of twins arise from monozygotic twins depending on the time of cleavage after fertilization as described in Table 1.2
Table 1: Different types of twins from monozygotic twins.
Advanced maternal age and use of reproductive techniques have increased the incidence of multiple pregnancies over the last decades. In the United States, the incidence of these pregnancies has increased by 59% between 1980 and 1999. Approximately 130,000 infants born in the United States are twins out of 4 million every year.3 Although monochorionic twins account for 3% of the entire group, they present 16% of the total perinatal mortality. Monochorionic twins have the highest risk of congenital malformations, perinatal mortality and morbidity.4 The incidence of monochorionic twins is very low, the outcomes for this kind of twins and the best gestational age for delivery have not been well studied. More studies are needed, and thus the aim of this study was to look into the neonatal outcomes of monochorionic twin pregnancies including the gestational age of delivery and to compare it with dichorionic twins. Although similar studies were reported in the literature, no study has yet been conducted in Oman. Different populations and different obstetric practices may modify rates of pregnancies with multiple gestations, as well as morbidity and mortality seen in this group.
Method
A retrospective cohort study of twin pregnancies was conducted at Sultan Qaboos University Hospital (SQUH) between January 2006 and December 2011. This is a tertiary care hospital with around 4,000 deliveries per year and a cesarean section rate of around 18%. The data of women with twin pregnancies and their infants were obtained from the medical records. This study was approved by Sultan Qaboos University-based ethical review committee. Two sets of twins were excluded because they were lost for follow-up.
Gestational age (GA) was determined by the last menstrual period or by ultrasound before 20 weeks of gestation. Chorionicity was determined by ultrasound examination in the antenatal period and confirmed by histological examination of the placenta in the postnatal period. Chorionicity was classified as: dichorionic diamniotic (DCDA), monochorionic diamniotic (MCDA) and monochorionic monoamniotic (MCMA). Twin to twin transfusion syndrome (TTTS) was diagnosed by the recognition of a single placenta, twin’s weight discordance, same gender, intrauterine growth restriction in the donor, normal or large size of the recipient, bladder sizes and abnormal Doppler’s at later stages. Growth discordant was diagnosed if the inter-pair difference in estimated fetal weights (EFW) was ≥20% (EFW large- EFW small/EFW large x 100).5
Preterm birth was defined as delivery before 37 weeks of gestation. Newborns weighing less than 2500 g was classified as low birth weight. Intrauterine fetal death (IUFD) was defined as death of the fetus inutero after 20 weeks gestation. Fetal hydrops was diagnosed with the presence of fluid in two or more fetal cavities. Respiratory distress syndrome (RDS) was diagnosed based on clinical and radiographic parameters. Congenital malformations were diagnosed by ultrasound examination during the antenatal period or by clinical examination of the neonate. The following data were recorded for each case: maternal demographics including age, gravidity, parity, past obstetrical history, previous surgeries, past medical history, last menstrual period, obstetrical complications during current pregnancy and neonatal outcome including: birth weight (BW), neonatal intensive care unit (NICU) admission, and complications of prematurity (Intraventricular hemorrhage, retinopathy of prematurity, respiratory distress syndrome, necrotizing enterocolitis, sepsis, death).
Continuous variables are reported as means with standard deviation (SD) and ranges. Catergorical variables are reported as frequencies and proportions. Chi-square test was used to compare between categorical variables and student t-test was used to compare between means. And p values of <0.05 is used for statistical significance.
Results
There were 51 sets of twin pregnancies in the study. Forty-six (90%) of the mothers were Omanis. The mean maternal age was 27.1 years (SD 4.1) and 15 (29%) of the mothers were primigravida. Pre-eclampsia was noted in 9 (18%) mothers. The most frequent route of delivery was cesarean section (94%) followed by normal vaginal delivery (6%), (Table 2). With respect to chorionicity, 36 (71%) pregnancies were DCDA, 14 (27%) were MCDA, and one (2%) was MCMA.
The Antepartum complications noted in the 15 monochronoic twins included: discordant fetal growth in 2 (13%) cases, low birth weight in 11 (73%) babies, pre-eclampsia in 3.
(20%) mothers, and TTTS in 4 (26.7%) sets. Fetal respiratory distress affected 8 (53%) pregnancies. Antepartum steroid for fetal lung maturity was given in 13 mothers (87%). Six (40%) twin sets were delivered before 30 weeks, 4 (27%) sets at 31-32 weeks, 2 sets (13%) at 35-36 weeks, 2 sets (13%) at 36-37 weeks and 1 set (7%) at 37-38 weeks. Fifteen mothers delivered 16 live infants (53%), 9 were stillbirths (30%) and 5 babies (17%) died after birth. Most neonatal mortality was the result of neonatal sepsis and pulmonary hypoplasia. (Tables 3 and 4)
Table 2: Maternal demographics.
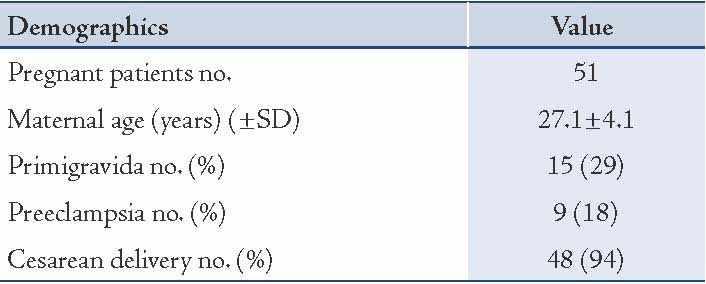
Table 3: Monochorionic pregnancy complications (15).
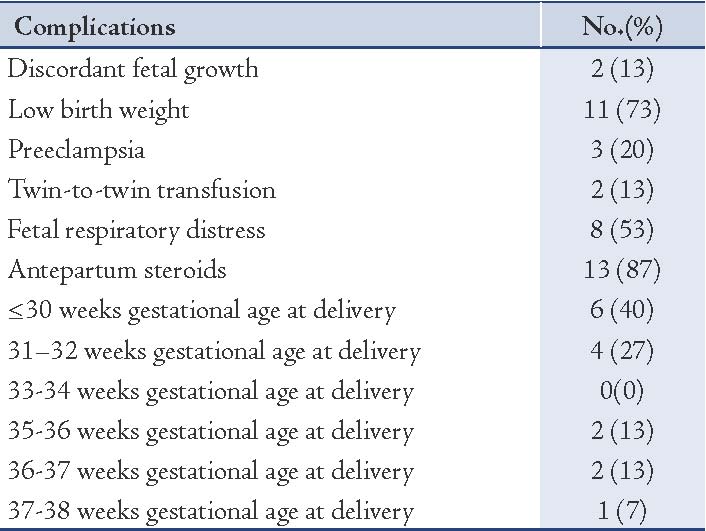
Table 4: Perinatal outcome in monochoroinic twin pregnancies
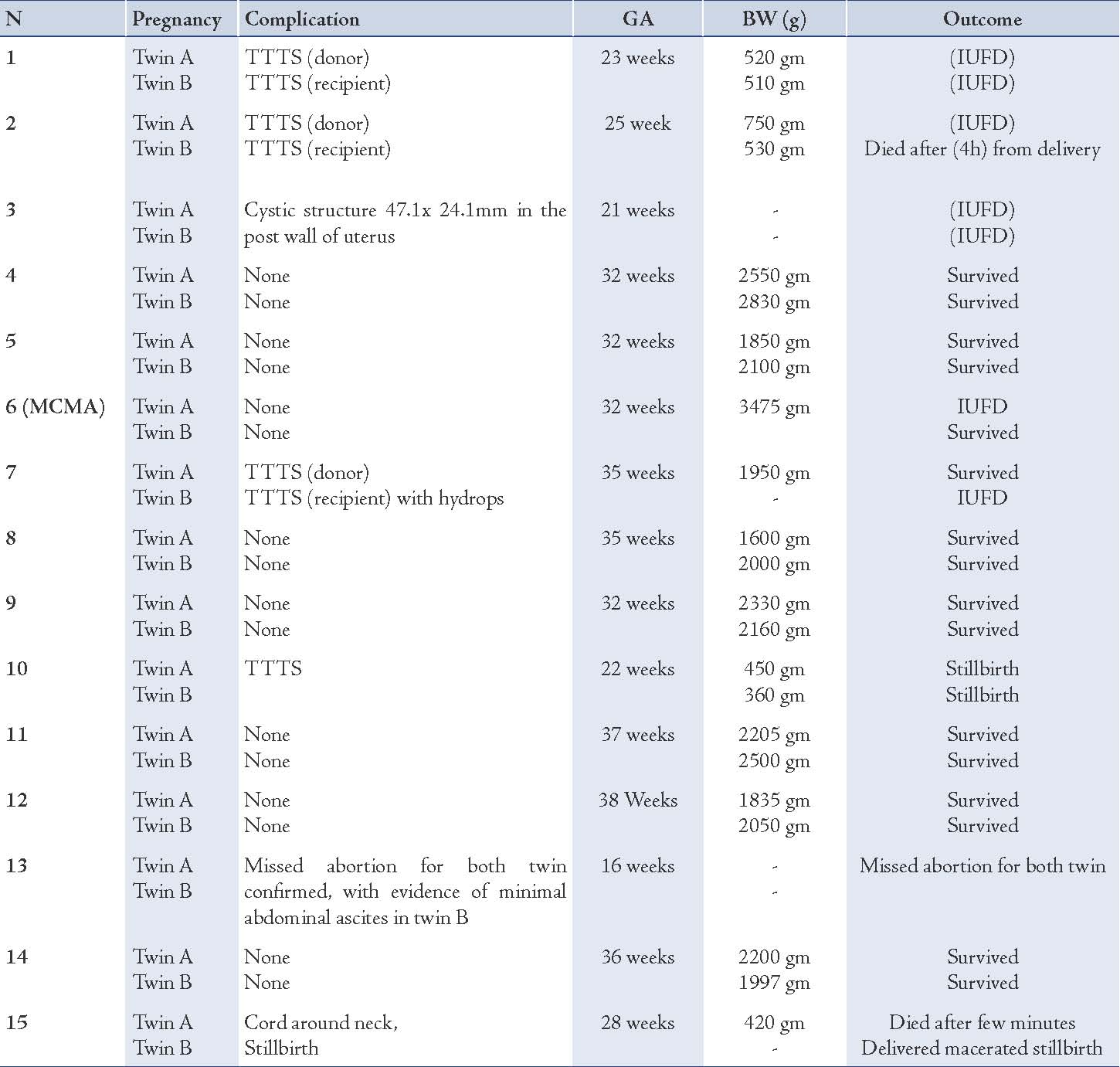
The outcomes for monochorionic twins were as follows:
1. Prematurity - which was seen in 13/15 (87%) prenancies delivered preterm
2. Twin-to-twin transfusion syndrome - There were four cases (27%) of TTTS. Two of the complicated cases are detailed below.
Case 1. This MCDA twin pregnancy was diagnosed with TTTS at 23 weeks gestation. The diagnosis was based on the presence of polyhydramnios/oligohydramnios sequence, fetal growth discordance and abnormal Doppler studies in the intrauterine growth-restricted twin. The larger twin progressed to fetal hydrops and the smaller infant was complicated by IUFD.
Case 2: This MCDA twin pregnancy was diagnosed at 22 weeks with TTTS. The larger twin developed fetal hydrops at 25 weeks gestation and was stillborn and the smaller twin was born alive and died after 4 hours. The twin had mildly dilated lateral ventricles.
There were two sets of MCDA twins which resulted in IUFD at 21 and 28 weeks gestation respectively, but the cause was unknown.
3. MCMA
In this study, there was only one set of MCMA twins. The mother was a primigravida who conceived spontaneously and had close follow-up during the pregnancy. She was admitted from 28 weeks gestation for fetal monitoring. No maternal or fetal complications were identified and after extensive counseling, the decision was made for cesarean delivery at 34 weeks. Unfortunately, sudden IUFD of one twin occurred at 32 weeks and an emergency cesarean section was performed. The death was attributed to cord entanglement. The surviving twin did well and MRI at first week of life and at 6 months did not show any hypoxic insult.
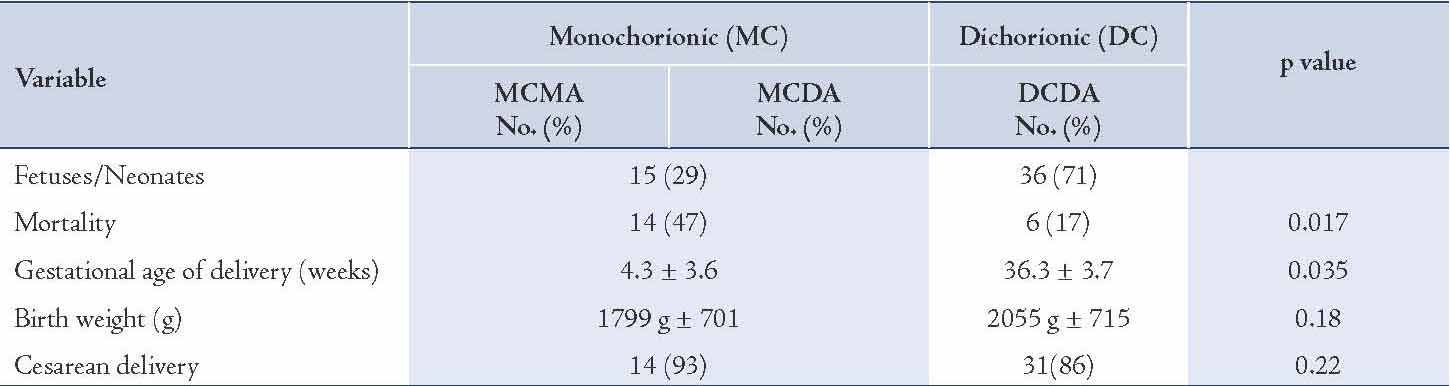
For the dichorioinic twins (DC), the mortality rate was significantly lower in DC (17%) when compared to MC (47%) twins (p=0.017). The mean gestational age at delivery was 36.3 weeks (±3.7) for DC twins and 34.3 weeks (±3.6) for MC twins (p=0.035). The mean birth weight of DC twins was 1799 g (SD: 701) and 2055 g (±715) for MC twins (p=0.18). The frequency of cesarean deliveries among DC twins was 14 (93%) compared with 31 (86%) for MC twins (p=0.22). The comparison between dichorioinic and monochorionic twins is illustrated in Table 5.
Table 5: Perinatal outcome in 51 fetuses of twin pregnancies according to chorionicity.
Discussion
Our study has shown a 47% mortality rate of monochorionic pregnancies mainly attributed to TTTS. This high rate could be explained by late presentation to our hospital and end stages of TTTS that had a poor prognosis. Monchrorionic pregnancies have high perinatal mortality of about 68%.6,7 This high rate could be explained by prematurity, TTTS, umbilical cord entanglements and congenital malformations.6,7 Before 1990, antenatal chorionicity determination was difficult; therefore, antenatal diagnosis of monchrorionic pregnancies was made in less than half of the patients and the majority were delivered vaginally.8 Over the last decades significant reduction in perinatal mortality has been reported, 40 to 60% in 1961 to 1962, reduced to 28% in 1961 to 1982, to 20% in 1997 to 1999 and 12% in 2001 to 2004.8-10 These changes in perinatal mortality can be explained by advanced fetal and neonatal management including antenatal diagnosis of twin type, close fetal surveillance, recognition of complications and early antenatal interventions.
The incidence of premature birth of twin pregnancies is higher than singletons and the monchrorionic twins are even at much greater risk. In our study, the mean gestational age of monochorionic twins at delivery was 34.3 weeks with 87% of deliveries occurring before 37 weeks. The mean age at delivery of twin pregnancies reported in previous studies was 35.6 weeks; this difference can be explained by the high frequency of pregnancies with complications referred to our Hospital. According to chorionicity, the mean gestational age at delivery was lower in monochorionic pregnancies compared to dichorionic pregnancies. Our study showed the mean gestational age of 36.3 week for dichorionic pregnancies and of 34.3 week for monochorionic pregnancies. In comparison with another study conducted at the Sao Paulo University School of Medicine, the mean gestational age at delivery was 36.7 weeks for dichorionic pregnancies and 35.6 weeks for monochorionic pregnancies.11
Low birth weight (LBW) was mostly seen in twin newborns than among singleton newborns. Birth weight below 2500 g is 8.3 times more common in twins in comparison to singleton and birth weights less than 1500 g is 10 times more common in twins.12 Classification regarding to chorionicity in our study showed a mean BW of 2055 g for dichorionic pregnancies and 1799 g for monochorionic pregnancies. Previous studies showed mean BW of 2165 g for dichorionic pregnancies and of 1827 g for monochorionic pregnancies almost similar to our study results.11
Twin-to-twin transfusion syndrome (TTTS) is more common in MCDA than MCMA pregnancies because MCDA placentas have less superficial arterio-arterial and more deep arteriovenous anastomoses than MCMA placentas.13,14 We report of TTTS in 4 of the 15 monochorionic pregnancies (27%), whereas TTTS was reported in previous studies as 8%.15 This difference could be explained by the small sample size of monochorionic twin gestations in our study and due to the large number of high risk pregnancies referred to our center.
The optimal time for delivery of monochorionic twins to reduce the risks from cord entanglement, growth discrepancies and intrauterine fetal death is still controversial. However, most literatures, reported that the optimal time for delivery of MCMA twins is no later than 32 to 34 weeks of gestation.7,10 Premature infants, especially those born before 32 weeks of gestation, have a high risks of perinatal depression, respiratory distress, patent ductus arteriosus, early-and late-onset sepsis, intracranial hemorrhage, necrotizing enterocolitis,, hospitalization and neurological complications.16 Our study had only one set of MCMA (2%) who were planned for delivery at 34 weeks but delivered at 32 weeks gestation due to sudden IUFD of one twin. Fortunately, the other twin was born alive and was discharged from hospital with no evidence of hypoxic insult.
The incedence of maternal and fetal complications increase significantly in twin pregnancies. As a result of the increase of twin pregnancies over the last decades, obstetricians must be the aware of the adverse neonatal outcomes in this type of pregnancy. It is very important to determine the chorionicity at the beginning of pregnancy as each type carries different prognosis and expected morbidity. This will also help towards counseling the parents. Chorionicity can be determined in the first trimester by ultrasound examination. Moreover, regular ultrasound follow-up can help in predicting of pregnancies that are at a higher risk of fetal growth restriction and discordant growth.17
The current study limitations include small sample size, retrospective study at one tertiary center and the low incidence of MCMA twins. Further studies involving more hospitals are needed to verify the current findings.
Conclusion
Monochorionic twins remain a group that carry high perinatal morbidity and mortality rates because they are more likely to involve twin-to-twin transfusion syndrome (TTTS), prematurity, fetal growth restriction and IUFD. However, improved fetal and neonatal management may result in better outcomes.
Acknowledgements
There was no conflict of interest between the authors in conducting this study and no funding was received for this work.
References
1. Sadler T.W. Longman Medical Embryology,10th edition .2006:104-108
2. Gambon HM. Essential of obstetrics and gynecology, 4th edition 2006: 183-185
3. Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep 2003 Dec;52(10):1-113.
4. Powers WF, Kiely JL. The risks confronting twins: a national perspective. Am J Obstet Gynecol 1994 Feb;170(2):456-461.
5. Victoria A, Mora G, Arias F. Perinatal outcome, placental pathology, and severity of discordance in monochorionic and dichorionic twins. Obstet Gynecol 2001 Feb;97(2):310-315.
6. Rodis JF, McIlveen PF, Egan JF, Borgida AF, Turner GW, Campbell WA. Monoamniotic twins: improved perinatal survival with accurate prenatal diagnosis and antenatal fetal surveillance. Am J Obstet Gynecol 1997 Nov;177(5):1046-1049.
7. Allen VM, Windrim R, Barrett J, Ohlsson A. Management of monoamniotic twin pregnancies: a case series and systematic review of the literature. BJOG 2001 Sep;108(9):931-936.
8. Carr SR, Aronson MP, Coustan DR. Survival rates of monoamniotic twins do not decrease after 30 weeks’ gestation. Am J Obstet Gynecol 1990 Sep;163(3):719-722.
9. Tessen JA, Zlatnik FJ. Monoamniotic twins: a retrospective controlled study. Obstet Gynecol 1991 Jun;77(6):832-834.
10. Ezra Y, Shveiky D, Ophir E, Nadjari M, Eisenberg VH, Samueloff A, et al. Intensive management and early delivery reduce antenatal mortality in monoamniotic twin pregnancies. Acta Obstet Gynecol Scand 2005 May;84(5):432-435.
11. De Assunção RA, Liao AW, De Lourdes Brizot M, Krebs VJ, Zugaib M. Perinatal outcome of twin pregnancies delivered in a teaching hospital. Obstet Gynecol 2010;56(4):447-451.
12. Brizot M, Fujita M, Reis N, Banduki J, Schultz R, Miyadahira S, et al. Malformações fetais em gestacao multipla. Rev Bras Ginecol Obstet 2000;22(8):511-517 .
13. Umur A, van Gemert MJ, Nikkels PG. Monoamniotic-versus diamniotic-monochorionic twin placentas: anastomoses and twin-twin transfusion syndrome. Am J Obstet Gynecol 2003 Nov;189(5):1325-1329.
14. Bajoria R. Vascular anatomy of monochorionic placenta in relation to discordant growth and amniotic fluid volume. Hum Reprod 1998 Oct;13(1O):2933-2940.
15. Suzuki S, Kaneko K, Shin S, Araki T. Incidence of intrauterine complications in monoamniotic twin gestation. Arch Gynecol Obstet 2001 May;265(2):57-59.
16. McIntire DD, Bloom SL, Casey BM, Leveno KJ. Birth weight in relation to morbidity and mortality among newborn infants. N Engl J Med 1999 Apr;340(16):1234-1238.
17. Machado RC, Brizot ML, Liao AW, Cabar FR, Zugaib M. Prenatal sonographic prediction of twin growth discordance. Twin Res Hum Genet 2007 Feb;10(1):198-201.
|