Thyroid malignancies are the most common of all endocrine tumors with the follicular variant representing the second most common tumor subtype.1,2 Treatment is usually surgery with adjuvant chemotherapy to achieve total remission. The prognosis is excellent with a 10-year survival rate greater than 90%.3 Dissemination of follicular thyroid carcinoma is primarily hematogenous, which in advanced disease results in pulmonary and bone deposits.4 Here we report a case of follicular thyroid cancer with extensive mediastinal, sternal, and ribs invasion that required tumor extirpation, sternectomy, and rib resection to relieve the patient’s symptoms.

Figure 1: Pre-operative image: anterior neck mass.
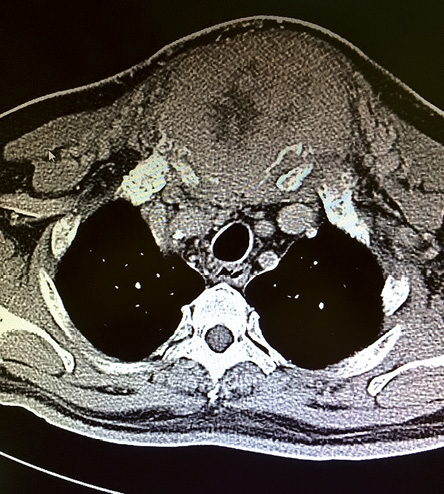
Figure 2: Computed tomography image of the tumor. The mass invaded the mediastinum with the involvement of sternum and ribs.

Figure 3: Computed tomography image of the tumor: coronal view of tumor and areas of invasion.
Case report
A 59-year-old man, with no prior medical illnesses, presented with a 10-year history of anterior chest mass [Figure 1]. The mass was initially pea sized but within the past two years it had progressively increased in size. He denied any airway or gut compressive symptoms but had lost weight in the past six months. He also complained of heat intolerance but no other thyroid hyperactivity symptoms. No voice change was noted.
Physical examination revealed a large 15 × 10 cm anterior chest wall mass fixed to the skin and underlying structures. The overlying skin was normal. The trachea remained central; however, the external jugular veins were dilated. There was also a neck swelling measuring 5 × 3 cm, which was not fixed to the skin and moved when the patient swallowed. The patient was biochemically and clinically euthyroid. His free thyroxine (T4) and thyrotropin (TSH) concentrations were 16.6 and 0.7, respectively. An initial computed tomography (CT) scan of the neck and thorax revealed an enlarged right thyroid lobe with no retrosternal extension [Figure 2 and 3]. However, there was an anterior mediastinal mass with local invasion to the sternum and ribs. Fine needle aspiration biopsy of the neck lesion was performed, which showed features suggestive of a follicular lesion.
A few days later, the patient underwent a total thyroidectomy, sternectomy, ribs resection, and a myocutaneous free flap reconstruction. Intraoperatively, it was found that the tumor had invaded the sternum both anteriorly and posteriorly with first to third rib involvement bilaterally [Figure 4]. It had also adhered to the superior vena cava and innominate vein posteriorly. The surgery was uncomplicated, and patient recovered fully [Figure 5]. He is scheduled for a whole body scan and radioiodine ablation in the future and is currently on regular follow-up.
Discussion
At the time of presentation, extracervical metastases are seen in 5–10% of patients with well-differentiated thyroid carcinoma.5 Patients frequently present with a chest mass and airway or esophagus compression symptoms. The most common cause of death in advanced thyroid carcinoma with extracervical metastases is asphyxia, which occurs in 26% of cases. Our focus, in this case, was the extensive sternal and ribs invasion as this creates a dilemma in treatment options and there are only a few isolated cases reported in the literature of extensive sternal deposits in thyroid carcinoma.6 Surgery is still the primary treatment of choice in these cases, followed by radioiodine ablation and close monitoring of disease progression post-operatively.
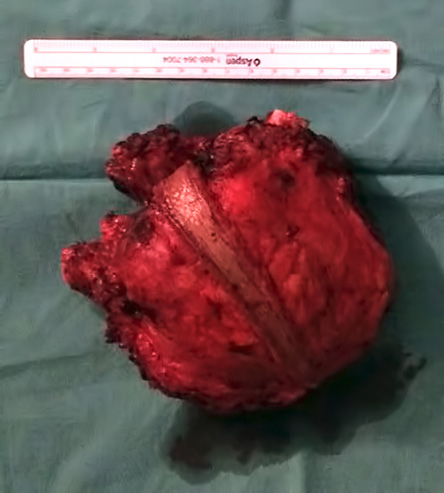
Figure 4: Specimen: en bloc resection of sternal metastases.

Figure 5: Post-operative image: successful myocutaneous flap coverage of mediastinal defect.
In advanced metastatic thyroid carcinoma, surgery is often of palliative value. However, the basis for surgical debulking is trying to achieve an optimal hypothetical ablation in addition to the symptomatic benefits. In this case, tumor debulking could assist the patient in his further treatment and could give him a longer-than-expected life expectancy added on with a better cosmetic result. Ozaki et al,7 in the 1990’s, reported that reconstruction of the sternal region using acrylic resin and polypropylene mesh was feasible. However, it was not performed due to financial constraints. In our case, no reconstruction was attempted, and a free myocutaneous flap was used to provide tissue cover for the patient postoperatively. Usually, acrylic resin and polypropylene mesh reconstruction is not feasible in situations of hostile tissue conditions (e.g., infection or incomplete resection). In our case, the en bloc resection nature of the ribs and sternum was deemed unsuitable for reconstruction by the operating surgeon and, due to financial constraints, no further attempts were made for reconstruction.
As local tumor control was achieved postoperatively, it is hoped that subsequent radioiodine ablation will improve the patient’s survival as suggested in a 2003 study.8 The authors suggested that a metastasectomy would improve the effectiveness of radioiodine administration postoperatively thus providing a discrete improvement in the patient’s survival rate. This is especially true with adequate tumor resection in the presence of pulmonary deposits as observed by Luna-Ortiz et al,9 in 2012 whereby a reduction in the tumor load assisted in the treatment of pulmonary deposits, which was not amenable to surgery. Hypothetical potentiation of radioiodine ablation also contributes to prevention of the symptoms associated with these lesions such as pain, ulceration, and dyspnea. These symptoms all occur at a later stage and affect the patient’s quality of life.10
Conclusion
Follicular thyroid carcinoma with bulky mediastinum, sternum, and ribs invasion may require palliative surgical resection to relieve patients’ symptoms and minimize the residual disease.
Disclosure
The authors declared no conflicts of interest. Written informed consent was obtained from the patient for publication of this case report and its accompanying images.
references
- Patel KN. Molecular Advances in the Diagnosis and Treatment of Thyroid Cancer. In: Terris D, Gourin C, editor. Thyroid and Parathyroid Diseases: Medical and Surgical Management. New York: Thieme; 2008.
- Passler C, Prager G, Scheuba C, Niederle BE, Kaserer K, Zettinig G, et al. Follicular variant of papillary thyroid carcinoma: a long-term follow-up. Arch Surg 2003 Dec;138(12):1362–1366.
- Grubbs EG, Rich TA, Li G, Sturgis EM, Younes MN, Myers JN, et al. Recent advances in thyroid cancer. Curr Probl Surg 2008 Mar;45(3):156–250.
- Hundahl SA, Fleming ID, Fremgen AM, Menck HR. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985–1995. Cancer 1998 Dec;83(12):2638–2648.
- Harness JK, McLeod MK, Thompson NW, Noble WC, Burney RE. Deaths due to differentiated thyroid cancer: a 46-year perspective. World J Surg 1988 Oct;12(5):623–629.
- Moraitis S, Perelas A, Toufektzian L, Mazarakis N, Pechlivanides G. Giant sternal metastasis secondary to follicular carcinoma of the thyroid gland: report of a case. Surg Today 2012 Sep;42(9):895–898.
- Ozaki O, Kitagawa W, Koshiishi H, Sugino K, Mimura T, Ito K. Thyroid carcinoma metastasized to the sternum: resection of the sternum and reconstruction with acrylic resin. J Surg Oncol 1995 Dec;60(4):282–285.
- Pak H, Gourgiotis L, Chang WI, Guthrie LC, Skarulis MC, Reynolds JC, et al. Role of metastasectomy in the management of thyroid carcinoma: the NIH experience. J Surg Oncol 2003 Jan;82(1):10–18.
- Luna-Ortiz K, Salcedo-Hernández RA, Lino-Silva LS, Gómez-Pedraza A. Two cases of sternectomy for bone metastasis due to aggressive variants of thyroid papillary carcinoma. Int J Sur Case Rep 2013;4(2):156–159.
- Kitamura Y, Shimizu K, Nagahama M, Sugino K, Ozaki O, Mimura T, et al. Immediate causes of death in thyroid carcinoma: clinicopathological analysis of 161 fatal cases. J Clin Endocrinol Metab 1999 Nov;84(11):4043–4049.