|
Abstract
Electric injury can cause a variety of cardiac arrhythmias. Atrial fibrillation as a result of such injury is very rare. We present a case of a young asymptomatic patient who developed acute atrial fibrillation with antegrade conduction over the atrioventricular bypass tract and very high ventricular rate after accidental low voltage electric injury, which was reverted successfully by DC shock.
Keywords: Atrial fibrillation; Pre-excitation; Electric injury.
Introduction
Electrical injuries can cause various cardiac arrhythmias. Low tension electrical injury seldom causes arrhythmia. Our case is unique as the patient had underlying asymptomatic Wolff–Parkinson-White syndrome, (WPW) syndrome which manifested as atrial fibrillation with fast antegrade conduction over accessory pathway after low voltage electric current.
Case Report
A 35-year-old male having no associated co-morbidities and cardiac risk factors experienced a low voltage (<350) electric shock at home. Immediately after the electric shock he developed palpitation and loss of consciousness, and he was referred to the emergency department at our hospital. On examination, he was drowsy, with cold clammy skin, pulse was feeble and irregular with a blood pressure of 90/60. He had a small entrance wound of about 5 mm at the tip of his middle finger on his right hand. Intravenous access was established and urgent 12 lead EKG was done. EKG revealed broad QRS tachycardia which was irregular with ventricular rate of 220 to 240 (Fig. 1). Tachycardia was reverted with 100 Joules biphasic synchronous DC shock. Base line ECG after cardioversion was showing short PR interval with delta waves in leads V1-V6 and in leads II, III and AVF (Fig. 2). These findings were diagnostic of WPW syndrome with left lateral accessory pathway. Amiodarone infusion was given for 24 hours. He had no recurrence of atrial fibrillation and cardiac monitoring was done for 48 hours. All baseline investigations viz complete blood count, kidney function, serum electrolytes, thyroid functions, and echocardiography were normal.
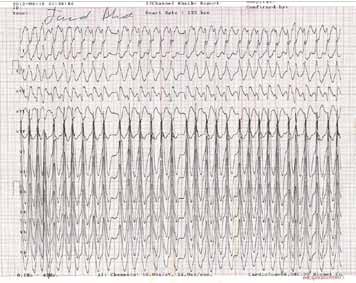
Figure 1: Irregular Wide QRS tachycardia due to antegrade conduction through accessory pathway).
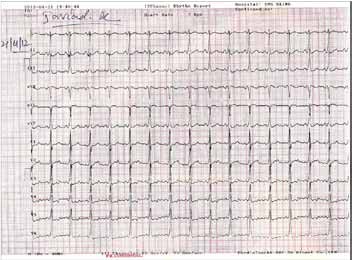
Figure 2: Post Cardioversion ECG revealing short PR interval with a slur in ascending limb of R wave (delta wave).
Discussion
Atrial fibrillation can occur in both cardiac and noncardiac disease or it can appear in the absence of any overt condition. Common causes include hypertension, valvular disease, coronary heart disease, cardiac surgery, thyrotoxicosis, excessive consumption of alcohol, and cardiomyopathy.1 The heart is one of the organs most vulnerable to electrical injury. Electrical injury may cause direct necrosis of the myocardium or cardiac dysrhythmia. Asystole and ventricular fibrillation are the most serious of the cardiac complications of electrical injury.1 Other possible rhythm disturbances include sinus tachycardia, bradycardia and nonspecific ST-T wave changes. There are also conduction defects such as various degrees of heart block, prolongation of the QT interval, and bundle brunch block.2 Supraventricular tachycardia and sick sinus syndrome have also been reported.3 The association of atrial fibrillation with electrical injury is rare,4-7and has usually occurred in instances of high tension (>1,000 V) electrical shock.
Cardiac dysrhythmias are more frequent in patients who lose consciousness at the time of injury and in patients who experience a high-tension electrical injury.1 Exposure to high-tension current will most likely cause ventricular asystole. The pathogenesis of the other cardiac dysrhythmias is not clear and is most likely multifactorial. Likely mechanisms include arrhythmogenic foci due to myocardial necrosis, alterations in the Na+- K+-adenosine triphosphatase concentration and changes in the permeability of myocytes membranes.1 Cardiac injury and rhythm disturbances can also be caused by anoxic injury in cases in which respiratory arrest precedes the injury to the heart.8-10 The need for cardiac monitoring after electrical injury is less well defined. The criteria for cardiac monitoring after an electrical injury are: loss of consciousness, abnormal electrocardiogram on admission, exposure to high voltage, and a history of cardiac disease.11 Our patient had syncope, was having hypotension and had manifested atrial fibrillation at admission which needed DC cardioversion. We did 48-hour cardiac monitoring with continuous telemetry and serial electrocardiograms, and we detected no rhythm disturbances.
Wolff-Parkinson-White syndrome is a disorder characterized by the presence of an accessory pathway which predisposes patients to tachyarrhythmias and sudden death. The prevalence of WPW syndrome is thought to be 0.1% to 0.3%, or 1 to 3 per 1000 people in the general population. Estimates of arrhythmia incidence in patients with pre-excitation vary widely, ranging from 12% to 80% in several surveys. Among patients with WPW syndrome, atrioventricular reentrant tachycardia (AVRT) is the most common arrhythmia, accounting for 95% of re-entrant tachycardias. It has been estimated that one-third of patients with WPW syndrome have atrial fibrillation (AF). AF is a potentially life-threatening arrhythmia.12 There is a small but significant risk of cardiac arrest due to the rapid conduction of atrial fibrillation over accessory pathway to ventricles leading to ventricular fibrillation.13 WPW syndrome presenting as atrial fibrillation with antegrade conduction over accessory AV pathway and having a very high ventricular rate leading to shock as a consequence of low-voltage electrical injury, however, has not been reported.10-12 We add to the literature this report of a 35-year-old man who developed atrial fibrillation with antegrade conduction over accessory atrioventricular bypass pathway complicated by very high ventricular rate leading to shock subsequent to low-voltage electrical injury with underlying WPW syndrome.
Conclusion
In conclusion, low-tension electrical injury can precipitate atrial fibrillation with very high ventricular rate as a result of antegrade conduction over accessory atrioventricular bypass tract leading to shock in an asymptomatic case of WPW syndrome. This type of arrhythmia with hemodynamic compromise has to be treated aggressively.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Varol E, Ozaydin M, Altinbas A, Dogan A. Low-tension electrical injury as a cause of atrial fibrillation: a case report. Tex Heart Inst J 2004;31(2):186-187.
2. Carleton SC. Cardiac problems associated with electrical injury. Cardiol Clin 1995 May;13(2):263-266.
3. Kose S, Iyisoy A, Kursaklioglu H, Demirtas E. Electrical injury as a possible cause of sick sinus syndrome. J Korean Med Sci 2003 Feb;18(1):114-115.
4. Shoenfeld P, Rupp J, Savage RW. Atrial fibrillation and electrical appliance injury. Mil Med 1991 May;156(5):254-255.
5. Wander GS, Bansal RK, Anand IS, Arora S, Khurana SB, Chawla LS. Atrial fibrillation following electrical injury. Jpn Heart J 1992 Jan;33(1):131-134.
6. Bøggild H, Freund L, Bagger JP. Persistent atrial fibrillation following electrical injury. Occup Med (Lond) 1995 Feb;45(1):49-50.
7. Arya KR, Taori GK, Khanna SS. Electrocardiographic manifestations following electric injury. Int J Cardiol 1996 Nov;57(1):100-101.
8. Santinelli V, Radinovic A, Manguso F, Vicedomini G, Gulletta S, Paglino G, et al. The natural history of asymptomatic ventricular pre-excitation a long-term prospective follow-up study of 184 asymptomatic children. J Am Coll Cardiol. 2009 20;53(3):275-80.
9. Jensen PJ, Thomsen PE, Bagger JP, Nørgaard A, Baandrup U. Electrical injury causing ventricular arrhythmias. Br Heart J 1987 Mar;57(3):279-283.
10. Robinson K, Rowland E, Krikler DM. Wolff-Parkinson-White syndrome: atrial fibrillation as the presenting arrhythmia. Br Heart J 1988 May;59(5):578-580.
11. Koumbourlis AC. Electrical injuries. Crit Care Med 2002 Nov;30(11)(Suppl):S424-S430.
12. Sethi KK, Dhall A, Chadha DS, Garg S, Malani SK, Mathew OP. WPW and preexcitation syndromes. J Assoc Physicians India 2007 Apr;55(Suppl):10-15.
13. Ashok TP, Sanjay Sharma, Mahesh Jain. Paroxysmal supraventricular tachycardia in the rural setting- Case reports and review. OMJ. 2008; Vol-23, No.2: 101-3.
|