|
Introduction
A 42-year-old male shopkeeper presented in the out-patient department (OPD), with intermittent cough for the last six months along with occasional compressive symptoms at the centre of chest and mild dyspnea on exertion. Detailed cardiological history was not contributory. Chest on auscultation showed diminished air entry in the left infra-scapular region with occasional crepitations; the right side of the chest and other systemic examinations were within normal limits. Chest X-ray postero-anterior (PA) view revealed a lobular opacity in the left cardio-phrenic angle. (Fig. 1)
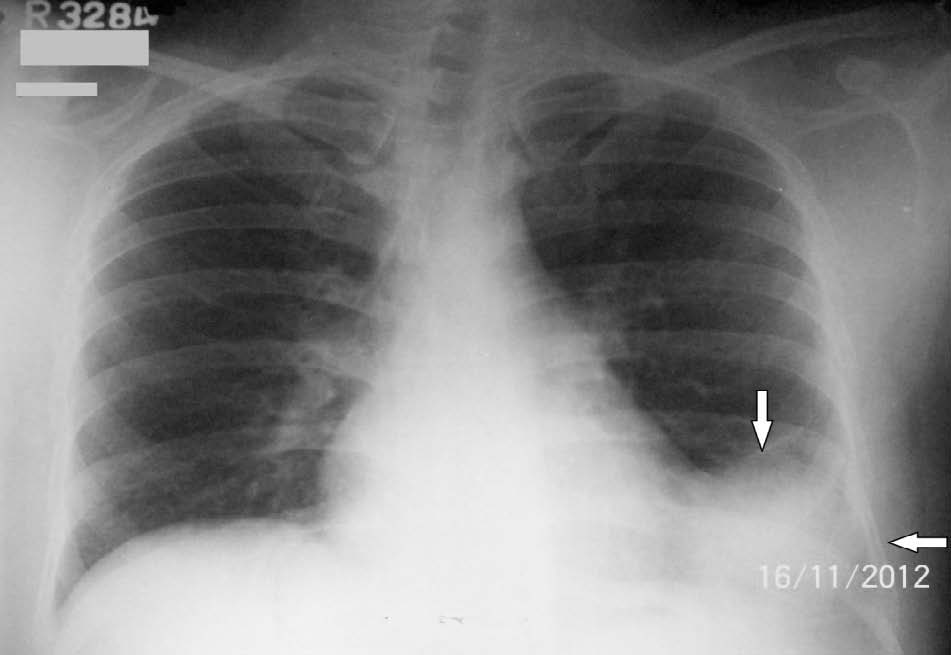
Figure 1: Chest X-ray PA view showing a lobular opacity at the left cardio-phrenic angle large enough to obscure the left costo-phrenic angle, shown by the arrow.
Routine blood investigations and 12-lead electrocardiography (ECG) revealed no abnormality. Two-dimensional echocardiography revealed a large well defined mass having echo-free space measuring 9.0 × 5.6 cm, resting on the postero-lateral side of the left ventricle (LV) without any connection to ventricular cavity (Fig. 2). But due to poor window, the exact morphological and anatomical nature of the mass could not be substantiated. Later contrast enhanced computed tomography (CECT) scan of the chest confirmed (Fig. 3), a large well circumscribed cystic lesion measuring 9.8 cm (antero-posterior) × 6.4 cm (supero-inferior) × 5.5 cm (transverse) in the left lower hemi-thorax, abutting the lateral aspect of the pericardial cavity, not separable from it and indenting the lateral wall of the LV. It had thin barely perceptible wall, homogeneous fluid attenuation content, without any foci of calcification, contrast enhancement, or internal septa.
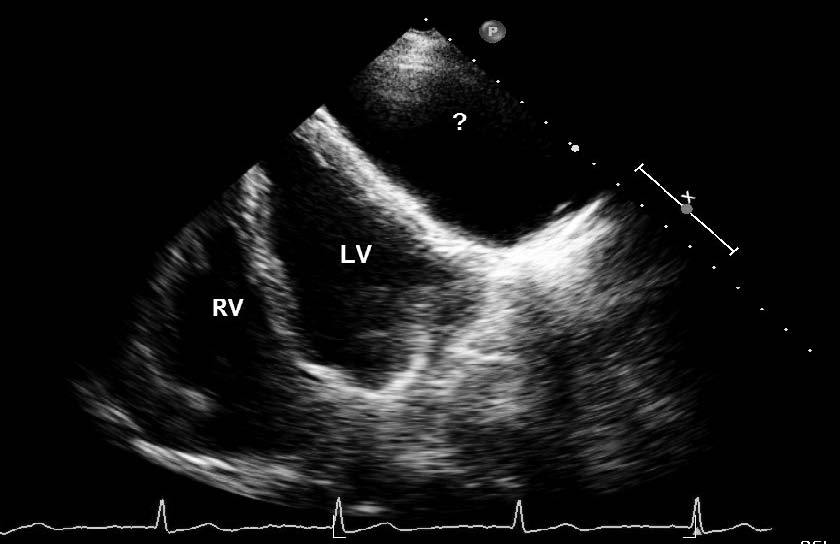
Figure 2: 2-D echocardiography showed a large well defined mass having echo-free space near the postero-lateral side of left ventricle (shown by interrogation mark).
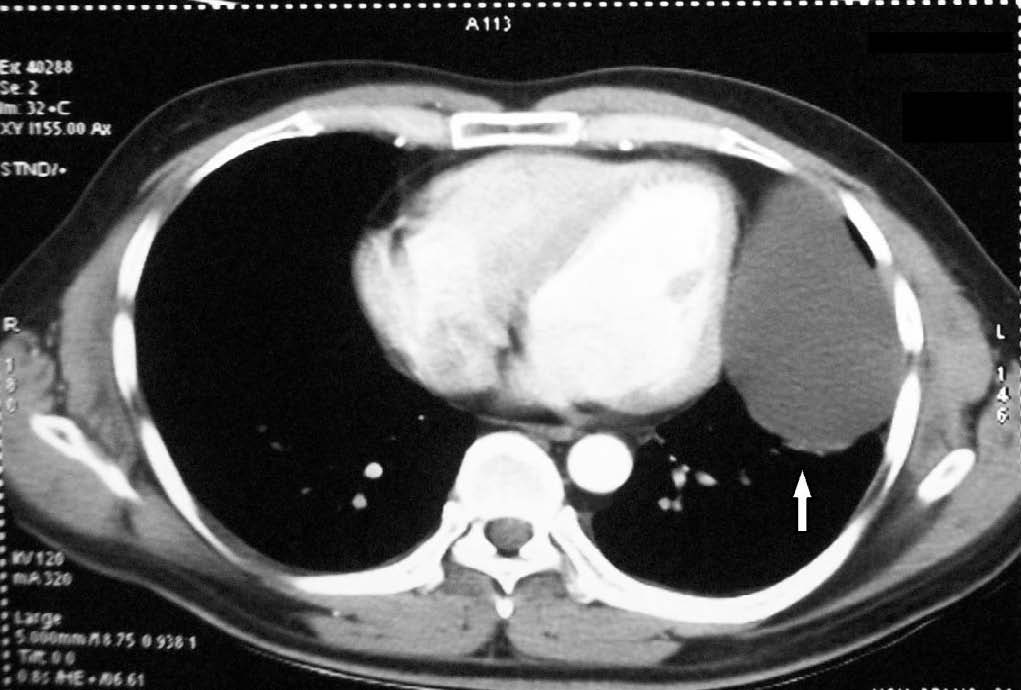
Figure 3: CECT chest showing a large well circumscribed cystic lesion in left lower hemi-thorax, abutting lateral aspect of pericardial cavity.
Question
What is the diagnosis?
Answer
All imaging studies suggested a large congenital benign pericardial cyst arising from the left cardiac border.
In view of this large pericardial cyst causing local compressive symptoms, cardio-vascular surgical opinion was taken and they suggested for surgical excision of the cyst. Surgical procedure was uneventful with postero-lateral thoracotomy in the 6th intercostal space and complete excision of the cyst measuring 9 cm × 7 cm × 5 cm, containing clear straw-coloured fluid inside. Biochemical analysis of the fluid favoured transudative nature according to Light’s criteria (cystic fluid protein was 2.8 g/dL, Lactate dehydrogenase (LDH) was 110 U/L; whereas serum protein was 6.4 g/dL and serum LDH was 190 U/L). Cell count of the fluid was 180/cu.mm with 90% lymphocyte and 10% neutrophil. Histopathological evaluation of the cyst showed the wall formed by only a single layer of cuboidal epithelial cells over a basement membrane formed by loose stroma and collagen fibers. The patient recovered favorably in post-operative period without any resurgence of compressive symptoms or cough.
Discussion
Primary cystic lesions comprise almost 20% of all mediastinal masses; cysts mostly originate from the local anatomical structures and causes symptoms mostly by compressive effects. Among them, pericardial cysts are the second most common mediastinal cysts following bronchial cyst; and they comprise 5-10% of all mediastinal masses.1 Embryologically, the pericardial sac is formed due to the fusion of mesenchymal lacunae and rarely pericardial cyst results due to the failure of fusion of these lacunae.2 Lillie suggested that pericardial cyst originates due to the non-fusion of an embryological ventral diverticlum.3 These cysts seem to be multi-locular externally due to multiple trabeculation but actually are uni-locular and contain clear watery or yellowish fluid of transudative nature. The cyst wall is formed by a single layer of mesothelial cells with a basement membrane formed by loose stroma consisting of collagen and elastic fibers. The cyst wall is sometimes infiltrated with lymphocytes, histiocytes, plasma cells, pigmented giant cells along with hyperplasia of mesothelial cell lining with foci of calcification, but malignant cells are never found. These cysts are asymptomatic in almost 75% of cases and incidentally observed in routine chest X-rays. The usual location is the right cardio-phrenic angle but can also rarely be found attached to the left cardio-phrenic angle (25% cases), or can even rarely protrude into the posterior, or superior mediastinum (8%).1,4,5
Though it follows a benign course throughout, it may in rare instances become symptomatic when it grows very large in size or when the wall is secondarily infected. Symptomatic patients generally present with progressive cough, chest pain (retro-sternal or at cardiac apex), dyspnea, palpitation, early satiety or dysphagia; but sometimes medical emergencies may arise for example: cyst rupture producing cardiac tamponade, cyst wall infection with erosion of large vessels and obstruction of larger airways causing sudden death.1,4 In the present case, local compression of the airways and other local mediastinal structures caused intermittent cough and occasional chest compressive symptoms.
Pankaj Kaul et al. reported a case of a large pericardial cyst producing local compressive effects, finally resulting in superior vena cava obstruction and right middle lobe atelectasis by obstructing the right main bronchus.6 Other rarer complications such as right ventricular outflow tract obstruction, atrial fibrillation, pulmonary stenosis and congestive heart failure have also been reported.1,4,5 As in our case, the cyst originated from the left cardio-phrenic angle which is not very common. The wall of the cyst showed only single layer of cuboidal epithelium in histopathological evaluation, ruling out possibilities of any recent infection or inflammation.
Routine chest X-ray and echocardiography are not very informative in this case. But literature suggests that radiologically cysts can be distinguished from cardiac shadow by delineating a minor gap between the actual cardiac muscle and the pericardium, as well as the independent free motion of the cyst.7 Roy et al. reported a case of superior vena cava syndrome caused by a similar anterior mediastinal mass found in echocardiography, associated with mild pericardial effusion, without involving myocardium or hampering cardiac motion, which was later proved by CT scan and histopathological examination as a large mediastinal germ cell tumor with malignant transformation.8 CECT scan finally helped to delineate the exact origin of the cyst in the current case. Magnetic resonance imaging (MRI) is useful but was not done in this case due to non-availability of resources. Surgical removal of the cyst was planned due to its large size and persistent symptoms. The indications for surgery in such benign pericardial cyst are large size, the patient’s request, persistent symptoms, and to rule out malignancy or to prevent complications.1,4,9
In conclusion, congenital pericardial cyst is a rare entity to produce mediastinal compressive symptoms. MRI or at least conventional CT scan is a better modality to demonstrate the origin of such cysts.
Acknowledgements
We express our sincere thanks to Senior Consultant Cardio-vascular surgeon Dr. Om Parkash Yadava for his contributions in final work up of the case.
References
1. Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, et al; Task Force on the Diagnosis and Management of Pricardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J 2004 Apr;25(7):587-610.
2. Lambert AV. Etiology of thin walled thoracic cysts. J Thorac Surg 1940;10:1-7.
3. Lillie WI, McDONALD JR, Clagett OT. Pericardial celomic cysts and pericardial diverticula; a concept of etiology and report of cases. J Thorac Surg 1950 Sep;20(3):494-504.
4. Patel J, Park C, Michaels J, Rosen S, Kort S. Pericardial cyst: case reports and a literature review. Echocardiography 2004 Apr;21(3):269-272.
5. McAllister HA Jr, Buja LM, Ferrans VJ. Pericardial disease. Anatomic abnormalities. In: Willerson JT, Cohn JN, Wellens HJJ, Holmes DR eds. Cardiovascular Medicine. 3rd Ed. Springer-Verlag, London 2007; 1479-82.
6. Kaul P, Javangula K, Farook SA. Massive benign pericardial cyst presenting with simultaneous superior vena cava and middle lobe syndromes. J Cardiothorac Surg 2008;3:32.
7. De Roover P, Maisin J, Lacquet A. Congenital pleuropericardial cysts. Thorax 1963 Jun;18:146-150.
8. Roy M, Bandyopadhyay R, Pandit N, Sengupta S. Superior Vena Cava Syndrome: A Presenting Feature of Mediastinal Germ Cell Tumor. Oman Med J 2010;25:131-133 .
9. Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005 Oct;128(4):2893-2909.
|