The world is experiencing a demographic shift towards an era of population aging, which is one of the five global ‘megatrends’.1 The global aging population is a result of increased life expectancy and declining fertility and mortality rates.2,3 Malaysia is no exception and has become an aging society,4 with a forecast to be an aged nation by 2030. Older persons are susceptible to disease and disability,5 leading to an increased disease burden and greater demand for health services.6,7 The care for the aged population also produces a great and critical challenge to the family and society at large.8,9 Consequently, promoting the health and well-being of older persons is of utmost importance to improve their quality of life in their later years.
The prevalence and definitions of successful or healthy aging vary between studies.10 The concept of healthy aging has evolved from a classic biomedical definition to encompass multidimensional models. The classical model identifies success aging based on three indicators: being free of illness or disability (and having no risk factors), having high physical and cognitive functioning, and active engagement in social and productive activities.11,12 However, it has been emphasized that being free of diseases was not the most important component in the concept of healthy aging,13,14 as age-related chronic diseases can coexist with healthy aging.15–17 Many older individuals have well-controlled health conditions that do not impair their ability to function, highlighting that healthy aging does not mean ‘without disease’.18,19 Several domains have been considered to define healthy aging, including major diseases,20–23 physical, cognitive, and emotional functions and social or productive engagement.21,24,25
Numerous variables have been studied as predictors of successful or healthy aging, including demographic factors such as age, gender, educational level, and marital status,26–28 behavioral factors like physical activity,28,29 smoking status,30 and dietary habits,31 economic factors such as income,21,32 and social factors including social connectedness, community activity, religious activity,33 strong religious belief,34 independence,35 positive self-perception of health,36 and life satisfaction.37 As healthy aging may be influenced by cultural background, age, and gender, it is essential to examine factors specific to the local cultural and social context.38
This study aimed to fill the gap in the literature by determining the prevalence and determinants of healthy aging using a multidimensional construct among older persons who may not be completely free of disease. A consensus on concise indicators for a universal healthy aging concept and its factors is crucial for non-western countries like Malaysia.
Methods
A cross-sectional survey was conducted among 765 Malaysian community-dwelling older persons aged ≥ 60 years, both with and without comorbidities. However, those who were dependent, such as severely frail older persons, those with severe cognitive impairment, mental disabilities, severe sensory impairment, and bedridden individuals, were excluded. Older persons living in institutions were also excluded. A two-stage cluster random sampling method was used, where all eight districts in the state were initially chosen, and then a sub-district was randomly selected from each district. Finally, all individuals who met the inclusion and exclusion criteria in each selected sub-district and were available during the data collection period were included in the study.
The sample size was calculated using the single proportion formula,39 considering the nearest estimation proportion of healthy older persons in Malaysia24 and two proportion formulas using the Power and Sample Size Calculation 3.1 software, taking into account variables that were documented as significant determinants with available reference parameters in the literature, such as physical activity.40 The final calculated sample size was 765 based on the latter objective, considering the cluster effect.
Health programs involving community-dwelling older persons were conducted in the selected sub-districts between October 2019 and February 2020 to gather data. Participants who consented to participate in this study underwent screening for mood and cognitive status, followed by an interview, anthropometric measurements, and physical assessment. The interviewer-guided session was conducted using a standardized questionnaire by trained enumerators. Participants’ comorbidities and chronic illnesses were self-reported and verified with either their relatives and/or medical cards.
The tools used in this study included questionnaires, anthropometric measurements, and physical assessments. The first section of the questionnaire covered explanatory variables, including sociodemographic characteristics, economic characteristics, physical and social living support, and behavioral status. The nutritional status was assessed by Mini Nutritional Assessment®,41,42 religious status was obtained using the Duke University Religion Index,43 and social status was obtained by nine items on social and community involvement.
The second section of the questionnaire assessed the dependent variable, healthy aging status. Healthy aging was operationalized based on the multidimensional criteria set by previous scholars.11,14 Participants were classified as healthy agers (HAs) and usual agers. HAs were those who fulfilled all five criteria: 1) presence of optimal health of common comorbidities such as controlled and stable hypertension, diabetes, heart disease, stroke, cancer, and chronic lung disease; 2) satisfactory physical functioning; 3) satisfactory cognitive functioning; 4) no depression; and 5) satisfactory social functioning. Usual agers refer to participants who met less than five criteria. They represented older persons with common or ordinary status or having typical physical, emotional, cognitive, and social functioning. Table 1 describes the tools and criteria of healthy aging.
Table 1: Description of healthy aging criteria.
|
Tool and indicator
|
a. Mean systolic blood pressure < 140 mmHg and mean diastolic blood pressure < 90 mmHg.
b. Fasting capillary glucose level of ≤ 7.0 mmol/L or postprandial ≤ 8.5 mmol/L.
c. No self-reported compromised functions due to underlying chronic diseases* and its complications.
|
Malay Katz ADL with score of 5–6,44 and Lawton Instrumental ADL with a score of 5 in men or 8 in women.45
|
Malay Geriatric Depression Scale of < 5.46
|
Malay Elderly Cognitive Assessment Questionnaire score of ≥ 44.47,48
|
Medical Outcome Study Social Support Survey score of ≥ 62.49
|
*Six major diseases include hypertension, diabetes, heart disease, stroke, cancer, and chronic lung disease. **Healthy agers: fulfil five criteria; usual agers: fulfil one, two, three, or four criteria only
ADL: Activities of Daily Living..
All these tools in the Malay version were pre-tested and validated by previous researchers. Additionally, nine items on social function and community involvement, which consists of membership, activity involvement, and social interaction, were newly developed and validated. The nutritional and physical status of the participants, including waist circumference, calf circumference, gait speed, and handgrip strength, were also obtained. Anthropometric measurements and physical assessments were carried out by trained researchers and personnel using standardized protocols.
All analyses were carried out using SPSS (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Descriptive statistics were used to describe the sociodemographics of the participants. Percentage and 95% CIs were used to estimate the prevalence of HAs. Determinants for healthy aging status were initially screened using simple logistic regression with a significance value set at p < 0.25 and later multivariable logistic regression with a significance set at p < 0.05.
A total of 41 independent variables under eight factors, including demographic (age, gender, educational level, marital status, employment status, etc.), economic (income, number of children, savings, property ownership, etc.), behavioral (diet consumption of protein, fruits and vegetable consumption, daily water intake, smoking habit, sleep duration, indoor activity and leisure activity, etc.), nutritional (body mass index (BMI), calf circumference, waist circumference, etc.) and physical status (handgrip strength and walking speed), social (living arrangement, pet ownership, status of caregiver during ill, own bedroom, etc.) and physical living support (use of cell phone, use of computer, use of information and communication technology application, and safety living environment), and religiosity (organizational religious activity, nonorganizational religious activity, and intrinsic religiosity) were tested as candidate predictors of healthy aging.
Approval to conduct this study was obtained from the Terengganu State Government i.e., Institut Modal Insan Terengganu Sejahtera (i-MiTS.TR.450/10/2-99) and the Human Ethics Committee of UniSZA.C/2/UHREC/628-2 Jld 2.11.
Results
A total of 765 respondents were included in the final data analysis, resulting in a 100% response rate. Among the overall sample, there were significantly more female respondents (64.1%) than males. The participants’ ages ranged from 60 to 88 years, with a mean age of 67.7±5.8 years. The largest proportion of respondents (41.7%) belonged to the young-old age group (60–64 years), while only 0.3% were in the oldest-old group (≥ 85 years).
Based on the adopted criteria and measures, 14.1% (95% CI: 11.64–16.59) of the respondents were classified as HAs. About 39.0%, 36.9%, and 9.0% met four, three, and two out of five healthy aging criteria, respectively [Figure 1]. Only 1.0% of the participants met one criterion of healthy aging. The prevalence of healthy aging status and corresponding percentages based on the criteria of healthy aging are presented in Table 2.
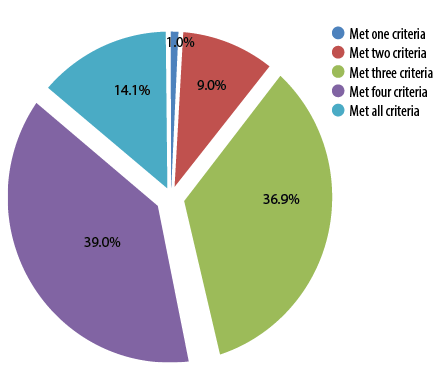 Figure 1: Distribution of participants who meet the criteria of healthy aging.
Figure 1: Distribution of participants who meet the criteria of healthy aging.
Table 2: Prevalence of healthy aging according to its multidimensional criteria (N = 765).
|
Presence of optimal health of common comorbidities
|
240 (31.4)
|
28.08–34.67
|
|
Satisfactory physical functioning
|
548 (71.6)
|
68.43–74.84
|
|
Good mood status
|
684 (89.4)
|
87.23–91.60
|
|
Satisfactory cognitive functioning
|
765 (100)
|
100.00–100.00
|
|
Well social functioning
|
500 (65.4)
|
61.98–68.74
|
|
Healthy aging status using all criteria
|
|
Healthy agers
(fulfil all five criteria)
|
108 (14.1)
|
11.64–16.59
|
Around a quarter (31.4%; 95% CI: 28.08–34.67) of the respondents reported optimal health for six common major diseases. Among the six major diseases, 31.4% of the respondents had one disease, 31.0% had two to three diseases, and 0.5% had more than three diseases. The most prevalent major chronic diseases were uncontrolled high blood pressure (55.4%) and uncontrolled diabetes mellitus (31.6%), whilst 0.3% were suffering from cancer. A high percentage of respondents (89.4%; 95% CI: 87.23–91.60) met the criteria for good mood status and satisfactory physical functioning (71.6%; 95% CI: 68.43–74.84). All respondents reported satisfactory cognitive functioning (100%). Nearly two-thirds (65.4%; 95% CI: 61.98–68.74) of them met the criteria for social functioning.
Variables were screened using simple logistic regression to identify potential predictors, and 20 out of 41 variables were statistically significant and identified in the univariable analysis, with a p-value < 0.25.50 The significant variables included sociodemographic characteristics (gender and marital status), socioeconomic factors (number of children and savings), physical living support characteristics (use of cell phone and information and communication technology application), religiosity (organizational religious activity, non-organization/private religious activities, and intrinsic religiosity), membership and social interaction, behavioral characteristic (daily water intake, protein intake, daily indoor activity, recreational leisure activity, and sleep duration), nutritional status (BMI, waist circumference, and calf circumference), and physical status (gait speed). These significant variables were then analyzed using multivariable logistic regression analysis.
Initially, the forward logistic regression yielded eight significant potential predictive variables. However, in the backward elimination model, a total of seven out of eight predictor variables were found to be statistically significant, excluding BMI. The significant variables for predicting healthy aging status were savings, water intake, calf circumference, waist circumference, gait speed, social interaction, and intrinsic religiosity [Table 3].
Table 3: Associated factors for healthy aging status using multiple logistic regression (N = 765).
|
Savings
|
|
No
|
1.69 (1.10–2.58)
|
1.71 (1.10–2.66)
|
5.561 (1)
|
0.018
|
|
Yes
|
|
Water intake, cups/day
|
|
< 5
|
1.78 (1.11–2.86)
|
2.01 (1.23–3.30)
|
7.671 (1)
|
0.006
|
|
≥ 5
|
|
Calf circumference
|
|
At risk
|
1.80 (1.16–2.79)
|
2.05 (1.24–3.38)
|
7.875 (1)
|
0.005
|
|
Not at risk
|
|
Waist circumference, cm
|
|
At risk
|
1.77 (1.17–2.68)
|
1.63 (1.04–2.55)
|
4.599 (1)
|
0.032
|
|
Not at risk
|
|
Gait speed
|
|
At risk
|
1.66 (1.04–2.64)
|
1.71 (1.04–2.80)
|
4.531 (1)
|
0.033
|
|
Not at risk
|
|
Social interaction
|
|
Unsatisfactory
|
3.00 (1.42–6.31)
|
2.82 (1.32–6.04)
|
7.107 (1)
|
0.008
|
|
Satisfactory
|
|
Intrinsic religiosity
|
|
Unsatisfactory
|
*Simple logistic regression; **multiple logistic regression.
Odds ratio; df: degree of freedom.
The model fit was reasonable, and model assumptions were met. There were no significant interactions, multicollinearity problems, or outliers detected.
Discussion
As the world’s population ages, the importance of healthy aging research is growing, and healthy aging has become a prominent theme globally. The term ‘healthy aging’ is often used interchangeably with concepts such as ‘active’, ‘successful’, and ‘productive’ aging. Unlike ‘successful aging’ or ‘anti-aging’ discourses, which focus on the prevention of disease or slowing the aging process, healthy aging emphasizes preserving physical and cognitive function despite the presence of health problems.51,52 It has been highlighted that applying multidimensional criteria to identify the older aging population in a better condition could be more informative than focusing on unidimensional health outcomes.53 To the best of our knowledge, this study is pioneering in considering the presence of major diseases with optimal health to be qualified as healthy aging, while others excluded them54–57 or included them based on the number of major diseases they have suffered.21,58 The current strategy tried to move away from highlighting multimorbidity but focused on how elders function in their surroundings while managing their illnesses.
The prevalence of healthy aging among community-dwelling elderly in Terengganu (14.1%) is comparable to successful aging rates among elderly individuals in Norway (14.5%)54 but slightly higher than rates reported among older Koreans (13.3%)21 and Americans (11.9%).22 However, it is lower than the rates reported among older Singaporeans (25.4–28.6%).23,59 Other local studies that also applied multidimensional criteria for successful aging reported healthy aging prevalence at 11% and 13.8%, respectively.24,57 Likewise, the results of this study seemed to be higher than older Nigerian (7.5%),60 Taiwanese (10.4%),61 Iranian (11.2%),62 and Dutch older persons (10.0%)63 that employed criteria that were more subjective and focused on psychosocial aspects.
It was discovered that substantial variability in successful and healthy aging prevalence has been reported mostly depending on the criteria/indicator used to define healthy aging. Most studies using restrictive criteria excluding major diseases as indicators for identifying healthy aging status have shown a lower prevalence.21,24,54,57 The result seems possible due to the multidimensional criteria applied to describe the healthy aging status.64,65 Another possible explanation for the low prevalence of healthy aging findings is that it seems commensurate with the fact that the prevalence of disease and disability is higher among older persons, as the majority (62.9%) of the participants suffered from at least one chronic disease. Additionally, there may be a discrepancy due to the different responses of the study population based on their cultures and value systems of what constitutes healthy aging.17
In the absence of a single gold standard for the measurement of healthy aging, this study has constructed a solid assessment comprising multidimensional criteria, namely physical, including health diseases and activities of daily living, mood status, and cognitive and social components as evidenced by the previous researchers11,14,24 for defining an accurate healthy aging status in this study. A multidimensional concept applied to define healthy aging in the present study is consistent with the World Health Organization's definition of healthy aging as “the process of promoting and maintaining functional capacity that allows well-being in old age”.19 Functional ability refers to having the mental and physical capacities that allow older persons to function (i.e., meet basic needs, make a decision, build and maintain relationships, and make contributions).19,66
Intrinsic religiosity was found to be the most significant factor associated with healthy aging status. The positive impact of spirituality and religiosity on well-being and coping with chronic diseases has been supported by previous studies.67,68 The strong religiosity observed among the Muslim participants in this study may contribute to their positive thinking and resilience in dealing with illnesses.69,70 The Muslim respondents considered illness, suffering, pain, and death as tests from God and regarded illness as a means of expunging one's sins.71
Furthermore, the participants in this study with satisfactory social contact were found to be healthier as compared to their counterparts. Older persons who have continuous interaction with others will have more positive health indices associated with healthy aging72 as well as enhanced level of health-related quality of life.73,74 In addition, our study revealed that savings were significantly associated with healthy aging status. It was found that financial issues can affect older persons' mental health and become a significant source of stress for many older persons.75,76 Furthermore, financial constraints have a significant impact on psychological health and well-being and may contribute to poor nutrition, mobility, functional status, and cognitive status.77,78 The importance of financial security in later life is underscored by the fact that older persons are more susceptible to morbidities, with some having neither a pension nor passive income. Older persons with more financial resources can access better preventive and tertiary healthcare.79,80
Besides, a positive and significant relationship between gait speed and healthy aging status signified that older persons who are physically competent have a better chance of being healthy than their at-risk counterparts. Older persons with delayed gait speed are at risk for physical frailty. Walking and physical activity are highly promoted among older persons as they are positively associated with good physical and functional well-being, as well as enhanced mood, better mental health, and proprioception preservation.81–84 In addition, gait speed has been proven reliable and sensitive in detecting frailty status and sarcopenia.85,86
Calf circumference was highly associated with nutrition status, diagnoses of sarcopenia, and frailty.87–89 The present results found that older persons who are not at risk for malnutrition have a better chance of being healthy than their at-risk counterparts. It reinforced research findings that a smaller calf circumference is linked to poor physical function, while a larger calf circumference was associated with better skeletal muscle mass, physical performance, and strength.90–93 Muscle mass plays a big role in musculoskeletal strength and mobility in maintaining independence in older age.94,95
Consistent with other studies, our study found a positive relationship between normal waist circumference and healthy aging status.96,97 The result supported other studies that discovered waist circumference was an accurate method for predicting general health, and those with abdominal obesity are more likely to score lower healthy aging score.97,98 The elderly with high waist circumference or obesity were more likely to suffer multimorbidity, cardiovascular diseases, chronic diseases such as diabetes, osteoporosis, arthritis, and mortality.99–103 Hence, it can be concluded that both nutritional indicators (normal calf and waist circumference) were positively associated with healthy aging status.
Fluid intake is rarely considered in the evaluation of dietary intake, even though it is a critical component of optimal metabolic function and nutritional status.104 There has been minimal research addressed fluid intake among older persons, and most studies are focused on adolescents or children and adults.105,106 To our knowledge, no other studies have included measures on water intake towards healthy aging, thus, limiting comparisons across populations. This study acknowledges the importance of daily fluid consumption for the elderly. Adequate hydration ensures the appropriate function of the kidneys, brain, and mood.107–109
The main strength of this study is the multidimensional criteria used to define healthy aging, which offers a holistic approach to healthy aging. Furthermore, the predictors associated with healthy aging revealed include components such as water intake, savings, and intrinsic religiosity, which have not previously been addressed. The existing local studies have included retrospective data from a national survey and a longitudinal study,23,56 while our study used a community-based cross-sectional study to determine the prevalence and associated factors of healthy aging. This study adds valuable data on participants in Terengganu, mainly for community settings. Additionally, the large study sample and the recruitment of participants from eight districts within one locality contribute to a better representation of the population and perhaps provide more accurate results.
However, this study has some limitations. It excluded fragility from the concept of healthy aging assessment, focusing on optimizing health and independence among older persons, and almost all successful or healthy aging studies exclude frailty status in their criteria. Frailty is a condition that impairs older persons' functioning, where they presented with low grip strength, low walking speed, low level of physical activity, self-reported exhaustion, and unintentional weight loss.110–114 It is characterized by loss of muscle mass, reduced functional capacities, and increased vulnerability to stressors.112,115
In addition to health aspects, the major aspects of social, religious, economic, behavioral, physical, and nutritional status were found to be the most significant in determining the health status of older persons. The healthy aging policy should consider a wider multidimensional health outcome approach to optimize opportunities for older people's health, social participation, and security.
Strengthening existing prevention initiatives for older persons is vital to support successful, healthy, and active aging. Health promotions on active lifestyles are highly recommended, especially during the International Day of Older Persons celebration on the first of October each year to honor the nation's elders.
It is suggested that policies and rules for retirement, continued paid work, pensions, and other income to support older age be considered. Malaysian policymakers and authorities should consider active aging policies that employ older persons into the workforce because this group has significant experience and expertise and can contribute ideas and guidance for future generations.116 Policy to support older adults to remain in the workforce, specifically with reduced working hours, part-time work, job-sharing, and working from home, can benefit from flexible working practices.
Conclusion
Our study emphasizes the importance of a multidimensional approach to healthy aging. Older persons with strong intrinsic religiosity, active social lives, good nutritional status, adequate water intake, physical competence, financial security, and healthy weight were more likely to age healthily. The findings can guide healthcare providers in supporting Malaysian older persons to adapt positively to the challenges of old age. Policymakers should consider active aging policies that involve older persons in the workforce to utilize their experience and expertise for the benefit of future generations. Future studies should replicate and expand on this research to develop a more comprehensive understanding of healthy aging and design effective intervention programs in health and social services.
Disclosure
The authors declared no conflict of interest. This study was supported by the Ministry of Higher Education, Malaysia (FRGS/1/2015/SS05/UNISZA/02/5–RR 149).
Acknowledgments
The authors would like to thank the participants in this study, the Healthy Aging Research Team, Faculty of Medicine UniSZA, and Terengganu State Health Department for their valuable support during the data collection period. The authors also appreciate the Terengganu State Government, Institut Modal Insan Terengganu Sejahtera, and Majlis Pengurusan Komuniti Kampung for their cooperation and support.
references
- 1. United Nations. World population ageing 2019: highlights. New York. Report No.: ST/ESA/SER.A/430. 2019 [cited 2023 December 20]. Available from: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf.
- 2. Fuster V. Changing demographics: a new approach to global health care due to the aging population. J Am Coll Cardiol 2017 Jun;69(24):3002-3005.
- 3. Tang CF, Tey NP. Low fertility in Malaysia: can it be explained? J Popul Res (Canberra) 2017;34(2):101-118.
- 4. DOSM. Press release: current population estimates, Malaysia, 2021. Department of Statistics Malaysia. Putrajaya. 2023 [cited 2023 December 24. Available from: https://www.dosm.gov.my/site/downloadrelease?id=current-population-estimates-malaysia-2021&lang=English&admin_view=.
- 5. Fong JH. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr 2019 Nov;19(1):323.
- 6. McGrath RP, Snih SA, Markides KS, Faul JD, Vincent BM, Hall OT, et al. The burden of health conditions across race and ethnicity for aging Americans: disability-adjusted life years. Medicine (Baltimore) 2019 Nov;98(46):e17964.
- 7. Acharya S, Ghimire S, Jeffers EM, Shrestha N. Health care utilization and health care expenditure of Nepali older adults. Front Public Health 2019 Feb;7:24.
- 8. Teerawichitchainan B, Knodel J. Long-term care needs in the context of poverty and population aging: the case of older persons in Myanmar. J Cross Cult Gerontol 2018 Jun;33(2):143-162.
- 9. Harper S. Living longer within ageing societies. J Popul Ageing 2019;12(2):133-136.
- 10. Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry 2006 Jan;14(1):6-20.
- 11. Rowe JW, Kahn RL. Successful aging. Gerontologist 1997 Aug;37(4):433-440.
- 12. Rowe JW, Kahn RL. Human aging: usual and successful. Science 1987 Jul 10;237(4811):143-149.
- 13. Nosraty L, Jylhä M, Raittila T, Lumme-Sandt K. Perceptions by the oldest old of successful aging, vitality 90+ study. J Aging Stud 2015 Jan;32:50-58.
- 14. Young Y, Frick KD, Phelan EA. Can successful aging and chronic illness coexist in the same individual? A multidimensional concept of successful aging. J Am Med Dir Assoc 2009 Feb;10(2):87-92.
- 15. Calasanti T. Combating ageism: how successful is successful aging? Gerontologist 2016 Dec;56(6):1093-1101.
- 16. Carver LF, Beamish R, Phillips SP, Villeneuve M. A scoping review: social participation as a cornerstone of successful aging in place among rural older adults. Geriatrics (Basel) 2018 Oct;3(4):1-16.
- 17. Phelan EA, Anderson LA, LaCroix AZ, Larson EB. Older adults’ views of "successful aging"–how do they compare with researchers’ definitions? J Am Geriatr Soc 2004 Feb;52(2):211-216.
- 18. Lowsky DJ, Olshansky SJ, Bhattacharya J, Goldman DP. Heterogeneity in healthy aging. J Gerontol A Biol Sci Med Sci 2014 Jun;69(6):640-649.
- 19. World Health Organization. World report on ageing and health. Vol. 56, Luxembourg. Geneva. 2015 [cited 2023 January 12]. Available from: https://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf?sequence=1&isAllowed=y.
- 20. Feng Q, Son J, Zeng Y. Prevalence and correlates of successful ageing: a comparative study between China and South Korea. Eur J Ageing 2014 Dec;12(2):83-94.
- 21. Jang HY. Factors associated with successful aging among community-dwelling older adults based on ecological system model. Int J Environ Res Public Health 2020 May;17(9):1-12.
- 22. McLaughlin SJ, Connell CM, Heeringa SG, Li LW, Roberts JS. Successful aging in the United States: prevalence estimates from a national sample of older adults. J Gerontol B Psychol Sci Soc Sci 2010 Mar;65B(2):216-226.
- 23. Subramaniam M, Abdin E, Vaingankar JA, Sambasivam R, Seow E, Picco L, et al. Successful ageing in Singapore: prevalence and correlates from a national survey of older adults. Singapore Med J 2019 Jan;60(1):22-30.
- 24. Hamid TA, Momtaz YA, Ibrahim R, Aizan T, Momtaz A, Hamid TA, et al. Predictors and prevalence of successful aging among older Malaysians. Gerontology 2012;58(4):366-370.
- 25. Wu M, Yang Y, Zhang D, Sun Y, Xie H, Zhang J, et al. Prevalence and related factors of successful aging among Chinese rural elders living in nursing homes. Eur J Ageing 2017 Mar;14(4):419-428.
- 26. Naah FL, Njong AM, Kimengsi JN. Determinants of active and healthy ageing in Sub-Saharan Africa: evidence from Cameroon. Int J Environ Res Public Health 2020 Apr;17(9):1-24.
- 27. Choi HS, Kwon MH. Associated determinants of successful ageing among older Koreans: from the 7th KNHANES. Indian J Public Health Res Dev 2019;10(11):4442-4449.
- 28. Pengpid S, Peltzer K. Successful ageing among a national community-dwelling sample of older adults in India in 2017–2018. Scientific Reports 2021 Nov 12;11(1):2218.
- 29. Gopinath B, Kifley A, Flood VM, Mitchell P. Physical activity as a determinant of successful aging over ten years. Sci Rep 2018 Jul;8(1):10522.
- 30. Bosnes I, Nordahl HM, Stordal E, Bosnes O, Myklebust TÅ, Almkvist O. Lifestyle predictors of successful aging: a 20-year prospective HUNT study. PLoS One 2019 Jul;14(7):e0219200.
- 31. Goshen A, Goldbourt U, Benyamini Y, Shimony T, Keinan-Boker L, Gerber Y. Association of diet quality with longevity and successful aging in Israeli adults 65 years or older. JAMA Netw Open 2022 Jun;5(6):e2214916.
- 32. Ho M, Pullenayegum E, Burnes D, Fuller-Thomson E. Successful aging among immigrant and Canadian born older adults: findings from the Canadian longitudinal study on aging (CLSA). Int J Environ Res Public Health 2022 Oct;19(20):1-18.
- 33. Carver LF, Beamish R, Phillips SP. Successful aging: illness and social connections. Geriatrics (Basel) 2018 Jan;3(1):1-7.
- 34. Ayu Cahyaningtyas N, Sudiyanto A, Soemanto R. Socioeconomic determinants of healthy ageing and the contextual effect of peer group: a multilevel evidence from Blora, Central Java. Journal of Epidemiology and Public Health. 2019;4(1):30-36.
- 35. Lee WJ, Peng LN, Lin MH, Loh CH, Chen LK. Determinants and indicators of successful ageing associated with mortality: a 4-year population-based study. Aging (Albany NY) 2020 Feb;12(3):2670-2679.
- 36. Maia LC, Colares TF, Moraes EN, Costa SM, Caldeira AP. Robust older adults in primary care: factors associated with successful aging. Rev Saude Publica 2020 Apr;54:35.
- 37. Dorji L, Jullamate P, Subgranon R, Rosenberg E. Predicting factors of successful aging among community dwelling older adults in Thimphu, Bhutan. Bangk Med J 2019;15(1):38-43.
- 38. Löckenhoff CE, De Fruyt F, Terracciano A, McCrae RR, De Bolle M, Costa PT Jr, et al. Perceptions of aging across 26 cultures and their culture-level associates. Psychol Aging 2009 Dec;24(4):941-954.
- 39. Ariffin WN. Introduction to sample size calculation. Education in Medicine Journal 2019 [cited 2022 July 16]. Available from: http://wnarifin.github.io.
- 40. Cramm JM, Lee J. Smoking, physical activity and healthy aging in India. BMC Public Health 2014 May;14(1):526.
- 41. Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 2001 Jun;56(6):M366-M372.
- 42. Vellas B, Villars H, Abellan G, Soto ME, Rolland Y, Guigoz Y, et al. Overview of the MNA–Its history and challenges. J Nutr Health Aging 2006;10(6):456-463, discussion 463-465.
- 43. Ng CG, Nurasikin MS, Loh HS, HA AY, Zainal NZ. Factorial validation of the Malay version of multidimensional scale of perceived social support among a group of psychiatric patients. Malaysian Journal of Psychiatry 2012 Dec 1;21(2):17-26.
- 44. Ibrahim NI, Ahmad MS, Zulfarina MS, Zaris SN, Mohamed IN, Mohamed N, et al. Activities of daily living and determinant factors among older adult subjects with lower body fracture after discharge from hospital: a prospective study. Int J Environ Res Public Health 2018 May;15(5):1002.
- 45. Kadar M, Ibrahim S, Razaob NA, Chai SC, Harun D. Validity and reliability of a Malay version of the Lawton instrumental activities of daily living scale among the Malay speaking elderly in Malaysia. Aust Occup Ther J 2018 Feb;65(1):63-68.
- 46. Ewe ET, Che Ismail H. Validation of Malay version of geriatric depression scale among elderly inpatients. Age 2004;17:65.
- 47. Kua EH, Ko SM. A questionnaire to screen for cognitive impairment among elderly people in developing countries. Acta Psychiatr Scand 1992 Feb;85(2):119-122.
- 48. Sherina MS, Rampal L, Mustaqim A. Cognitive impairment among the elderly in a rural community in Malaysia. Med J Malaysia 2004 Jun;59(2):252-257.
- 49. Norhayati MN, Aniza AA, Nik Hazlina NH, Azman MY. Psychometric properties of the revised Malay version medical outcome study social support survey using confirmatory factor analysis among postpartum mothers. Asia Pac Psychiatry 2015 Dec;7(4):398-405.
- 50. Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med 2008 Dec;3:17.
- 51. World Health Organization. Global strategy and action plan on ageing and health (2016 - 2020): a framework for coordinated global action by the World Health Organization, Member States, and Partners across the Sustainable Development Goals. 2016 [cited 2023 February 5]. Available from: https://www.partners-popdev.org/wp-content/uploads/2017/05/GSAP-Summary-EN.pdf.
- 52. World Health Organization. Healthy ageing and functional ability. 2020 [cited 2021 March 29]. Available from: https://www.who.int/news-room/questions-and-answers/item/healthy-ageing-and-functional-ability.
- 53. Cosco TD, Prina AM, Perales J, Stephan BC, Brayne C. Operational definitions of successful aging: a systematic review. Int Psychogeriatr 2014 Mar;26(3):373-381.
- 54. Bosnes I, Almkvist O, Bosnes O, Stordal E, Romild U, Nordahl HM. Prevalence and correlates of successful aging in a population-based sample of older adults: the HUNT study. Int Psychogeriatr 2017 Mar;29(3):431-440.
- 55. Abolfathi Momtaz Y, Hamid TA, Ibrahim R, Yahaya N, Abdullah SS. Moderating effect of Islamic religiosity on the relationship between chronic medical conditions and psychological well-being among elderly Malays. Psychogeriatrics 2012 Mar;12(1):43-53.
- 56. Tsou MT. Prevalence and risk factors for insomnia in community-dwelling elderly in northern Taiwan. Journal of Clinical Gerontology and Geriatrics 2013;4(3):75-79.
- 57. Vanoh D, Shahar S, Din NC, Omar A, Vyrn CA, Razali R, et al. Predictors of poor cognitive status among older Malaysian adults: baseline findings from the LRGS TUA cohort study. Aging Clin Exp Res 2017 Apr;29(2):173-182.
- 58. Hsu HC, Jones BL. Multiple trajectories of successful aging of older and younger cohorts. Gerontologist 2012 Dec;52(6):843-856.
- 59. Ng TP, Broekman BF, Niti M, Gwee X, Kua EH. Determinants of successful aging using a multidimensional definition among Chinese elderly in Singapore. Am J Geriatr Psychiatry 2009 May;17(5):407-416.
- 60. Gureje O, Oladeji BD, Abiona T, Chatterji S. Profile and determinants of successful aging in the Ibadan study of ageing. J Am Geriatr Soc 2014 May;62(5):836-842.
- 61. Li CI, Lin CH, Lin WY, Liu CS, Chang CK, Meng NH, et al. Successful aging defined by health-related quality of life and its determinants in community-dwelling elders. BMC Public Health 2014 Sep;14:1013.
- 62. Zanjari N, Momtaz YA. Successful aging among a sample of Iranian older adults. Open Psychol J 2020;13:67-73.
- 63. von Faber M, Bootsma–van der Wiel A, van Exel E, Gessekloo J, Lagaay AM, van Dongen E, Knook DL, et al. Successful Aging in the Oldest Old: Who Can Be Characterized as Successfully Aged? Arch Intern Med. 2001 Dec;161(22):2694–2700.
- Canêdo AC, Lopes CS, Lourenço RA. Prevalence of and factors associated with successful aging in Brazilian older adults: frailty in Brazilian older people Study (FIBRA RJ). Geriatr Gerontol Int 2018 Aug;18(8):1280-1285.
- 64. Garcia RF, Cassinello DZ, Bravo DL, Martinez AM, Nicolas JD, Lopez PM, et al. Successful ageing: criteria and predictors. Psychol Spain 2011;15(1):94-101.
- 65. Moreno-Agostino D, Prina M, Chua KC, Jotheeswaran AT, Sadana R, Officer A, et al. Measuring functional ability in healthy ageing: a nationwide cross-sectional survey in the Philippine older population. BMJ Open 2021 Oct;11(10):e050827.
- 66. Abu HO, Ulbricht C, Ding E, Allison JJ, Salmoirago-Blotcher E, Goldberg RJ, et al. Association of religiosity and spirituality with quality of life in patients with cardiovascular disease: a systematic review. Qual Life Res 2018 Nov;27(11):2777-2797.
- 67. Pilger C, Santos RO, Lentsck MH, Marques S, Kusumota L. Spiritual well-being and quality of life of older adults in hemodialysis. Rev Bras Enferm 2017;70(4):689-696.
- 68. Bekhet AK, Sarsour I. The relationship between positive thinking, religion, and health from the perspectives of Arab University Students. Journal of Clinical Trials and Case Reports 2018;1(2):1-6.
- 69. Manning L, Ferris M, Rosario CN, Prues M, Bouchard L. Spiritual resilience: understanding the protection and promotion of well-being in the later life. J Relig Spiritual Aging 2019;31(2):168-186.
- 70. Attum B, Hafiz S, Malik A, Shamoon Z. Cultural competence in the care of Muslim patients and their families. StatPearls Publishing LLC; 2023.
- 71. Dawson-Townsend K. Social participation patterns and their associations with health and well-being for older adults. SSM Popul Health 2019 Jun;8:100424.
- 72. Bahramnezhad F, Chalik R, Bastani F, Taherpour M, Navab E. The social network among the elderly and its relationship with quality of life. Electron Physician 2017 May;9(5):4306-4311.
- 73. Feng Z, Cramm JM, Nieboer AP. Social participation is an important health behaviour for health and quality of life among chronically ill older Chinese people. BMC Geriatr 2020 Aug;20(1):299.
- 74. Behanova M, Katreniakova Z, Nagyova I, van Ameijden EJ, van Dijk JP, Reijneveld SA. Elderly from lower socioeconomic groups are more vulnerable to mental health problems, but area deprivation does not contribute: a comparison between Slovak and Dutch cities. Eur J Public Health 2017 May;27(2)(suppl_2):80-85.
- 75. Wilkinson LR. Financial strain and mental health among older adults during the great recession. J Gerontol B Psychol Sci Soc Sci 2016 Jul;71(4):745-754.
- 76. Seah B, Espnes GA, Ang EN, Lim JY, Kowitlawakul Y, Wang W. Supporting the mobilization of health assets among older community dwellers residing in senior-only households in Singapore: a qualitative study. BMC Geriatr 2020 Oct;20(1):411.
- 77. Shahar S, Vanoh D, Mat Ludin AF, Singh DKA, Hamid TA. Factors associated with poor socioeconomic status among Malaysian older adults: an analysis according to urban and rural settings. BMC Public Health 2019 Jun 13;19(Suppl 4):549.
- 78. Huang R, Ghose B, Tang S. Effect of financial stress on self-rereported health and quality of life among older adults in five developing countries: a cross sectional analysis of WHO-SAGE survey. BMC Geriatr 2020 Aug;20(1):288.
- 79. Weida EB, Phojanakong P, Patel F, Chilton M. Financial health as a measurable social determinant of health. PLoS One 2020 May;15(5):e0233359.
- 80. Stanghelle B, Bentzen H, Giangregorio L, Pripp AH, Bergland A. Associations between health-related quality of life, physical function and pain in older women with osteoporosis and vertebral fracture. BMC Geriatr 2019 Nov;19(1):298.
- 81. Geraldes AA, da Silva WB, Júnior PB, Pereira PM. Effects of walking on the mood of physically active older people. Rev Bras Med Esporte 2019;25(1):63-66.
- 82. Hackett RA, Davies-Kershaw H, Cadar D, Orrell M, Steptoe A. Walking speed, cognitive function, and dementia risk in the English longitudinal study of ageing. J Am Geriatr Soc 2018 Sep;66(9):1670-1675.
- 83. Ribeiro F, Oliveira J. Aging effects on joint proprioception: the role of physical activity in proprioception preservation. Eur Rev Aging Phys Act 2007;4(2):71-76.
- 84. Bortone I, Sardone R, Lampignano L, Castellana F, Zupo R, Lozupone M, et al. How gait influences frailty models and health-related outcomes in clinical-based and population-based studies: a systematic review. J Cachexia Sarcopenia Muscle 2021 Apr;12(2):274-297.
- 85. Perez-Sousa MA, Venegas-Sanabria LC, Chavarro-Carvajal DA, Cano-Gutierrez CA, Izquierdo M, Correa-Bautista JE, et al. Gait speed as a mediator of the effect of sarcopenia on dependency in activities of daily living. J Cachexia Sarcopenia Muscle 2019 Oct;10(5):1009-1015.
- 86. Carrier N, Villalon L, Lengyel C, Slaughter SE, Duizer L, Morrison-Koechl J, et al. Diet quality is associated with malnutrition and low calf circumference in Canadian long-term care residents. BMC Nutr 2019 Dec;5(1):57.
- 87. Chen CY, Tseng WC, Yang YH, Chen CL, Lin LL, Chen FP, et al. Calf circumference as an optimal choice of four screening tools for sarcopenia among ethnic Chinese older adults in assisted living. Clin Interv Aging 2020 Dec;15:2415-2422.
- 88. Liu Q, Cai H, Yang LH, Xiang YB, Yang G, Li H, et al. Depressive symptoms and their association with social determinants and chronic diseases in middle-aged and elderly Chinese people. Sci Rep 2018 Mar;8(1):3841.
- 89. Kim S, Kim M, Lee Y, Kim B, Yoon TY, Won CW. Calf circumference as a simple screening marker for diagnosing sarcopenia in older Korean adults: the Korean frailty and aging cohort study (KFACS). J Korean Med Sci 2018 Apr;33(20):e151.
- 90. Pagotto V, Santos KF, Malaquias SG, Bachion MM, Silveira EA. Calf circumference: clinical validation for evaluation of muscle mass in the elderly. Rev Bras Enferm 2018;71(2):322-328.
- 91. Urquiza M, Fernandez N, Arrinda I, Sierra I, Irazusta J, Rodriguez Larrad A. Nutritional status is associated with function, physical performance and falls in older adults admitted to geriatric rehabilitation: a retrospective cohort study. Nutrients 2020 Sep;12(9):1-14.
- 92. Sun YS, Kao TW, Chang YW, Fang WH, Wang CC, Wu LW, et al. Calf Circumference as a novel tool for risk of disability of the elderly population. Sci Rep 2017 Nov;7(1):16359.
- 93. Dos Santos L, Cyrino ES, Antunes M, Santos DA, Sardinha LB. Sarcopenia and physical independence in older adults: the independent and synergic role of muscle mass and muscle function. J Cachexia Sarcopenia Muscle 2017 Apr;8(2):245-250.
- 94. Wang DX, Yao J, Zirek Y, Reijnierse EM, Maier AB. Muscle mass, strength, and physical performance predicting activities of daily living: a meta-analysis. J Cachexia Sarcopenia Muscle 2020 Feb;11(1):3-25.
- 95. Singh-Manoux A, Sabia S, Bouillon K, Brunner EJ, Grodstein F, Elbaz A, et al. Association of body mass index and waist circumference with successful aging. Obesity (Silver Spring) 2014 Apr;22(4):1172-1178.
- 96. Xu F, Earp JE, Greene GW, Cohen SA, Lofgren IE, Delmonico MJ, et al. Temporal association between abdominal weight status and healthy aging: findings from the 2011–2018 national health and aging trends study. Int J Environ Res Public Health 2020 Aug;17(16):1-13.
- 97. Darsini D, Hamidah H, Notobroto HB, Cahyono EA. Health risks associated with high waist circumference : a systematic review. J Public Health Res 2020 Jul 3;9(2):1811.
- 98. Shariff Ghazali S, Seman Z, Zainuddin NH, Omar MA, Sooryanarayana R, Ariaratnam S, et al. Prevalence and factors associated with multimorbidity among older adults in Malaysia: a population-based cross-sectional study. BMJ Open 2021 Oct;11(10):e052126.
- 99. Banerjee S, Kumar P, Srivastava S, Banerjee A. Association of anthropometric measures of obesity and physical activity with cardio-vascular diseases among older adults: evidence from a cross-sectional survey, 2017-18. PLoS One 2021 Dec;16(12):e0260148.
- 100. He P, Zhong J, Zhu DC, Ge B, Lei SF, Deng FY. Does obesity mediate the relationship between diabetes and osteoporosis in Chinese elderly population? Am J Hum Biol 2022 Mar;34(3):e23630.
- 101. Misra D, Fielding RA, Felson DT, Niu J, Brown C, Nevitt M, et al; MOST study. Risk of knee osteoarthritis with obesity, sarcopenic obesity, and sarcopenia. Arthritis Rheumatol 2019 Feb;71(2):232-237.
- 102. Santamaría-Ulloa C, Chinnock A, Montero-López M. Association between obesity and mortality in the Costa Rican elderly: a cohort study. BMC Public Health 2022 May;22(1):1007.
- 103. Engelheart S, Brummer R. Assessment of nutritional status in the elderly: a proposed function-driven model. Food Nutr Res 2018 Apr;62:1-6.
- 104. Aphamis G, Stavrinou PS, Andreou E, Giannaki CD. Hydration status, total water intake and subjective feelings of adolescents living in a hot environment, during a typical school day. Int J Adolesc Med Health 2019 Apr;33(4):1-7.
- 105. Säve-Söderbergh M, Toljander J, Mattisson I, Åkesson A, Simonsson M. Drinking water consumption patterns among adults-SMS as a novel tool for collection of repeated self-reported water consumption. J Expo Sci Environ Epidemiol 2018 Mar;28(2):131-139.
- 106. Pross N. Effects of dehydration on brain functioning: a life-span perspective. Ann Nutr Metab 2017;70(Suppl 1):30-36.
- 107. Nakamura Y, Watanabe H, Tanaka A, Yasui M, Nishihira J, Murayama N. Effect of increased daily water intake and hydration on health in Japanese adults. Nutrients 2020 Apr;12(4):1-17.
- 108. Young HA, Cousins A, Johnston S, Fletcher JM, Benton D. Autonomic adaptations mediate the effect of hydration on brain functioning and mood: evidence from two randomized controlled trials. Sci Rep 2019 Nov;9(1):16412.
- 109. Wleklik M, Uchmanowicz I, Jankowska EA, Vitale C, Lisiak M, Drozd M, et al. Multidimensional approach to frailty. Front Psychol 2020 Mar;11(564):564.
- 110. Sobhani A, Sharifi F, Fadayevatan R, Kamrani AA, Moodi M, Khorashadizadeh M, et al. Low physical activity is the strongest factor associated with frailty phenotype and frailty index: data from baseline phase of Birjand longitudinal aging study (BLAS). BMC Geriatr 2022 Jun;22(1):498.
- 111. World Health Organization. WHO clinical consortium on healthy ageing: topic focus: frailty and intrinsic capacity: report of consortium meeting, 1–2 December 2016 in Geneva, Switzerland. Vol. WHO/FWC/A. Geneva; 2017.
- 112. Wang X, Hu J, Wu D. Risk factors for frailty in older adults. Medicine (Baltimore) 2022 Aug;101(34):e30169.
- 113. Mohd Hamidin FA, Adznam SN, Ibrahim Z, Chan YM, Abdul Aziz NH. Prevalence of frailty syndrome and its associated factors among community-dwelling elderly in East Coast of Peninsular Malaysia. SAGE Open Med 2018 May;6:2050312118775581.
- 114. Ringer T, Hazzan AA, Agarwal A, Mutsaers A, Papaioannou A. Relationship between family caregiver burden and physical frailty in older adults without dementia: a systematic review. Syst Rev 2017 Mar;6(1):55.
- 115. Mohd SN, Ishak AA, Selvaratnam DP. Ageing population’s impact on economic growth in Malaysia from 1981 to 2019: evidence from an autoregressive distributed lag approach. Front Public Health 2021 Nov;9:731554.