Depression during pregnancy is quite common, with an estimated prevalence of 10–15% among pregnant women.1 The use of antidepressants during pregnancy has been increasing in recent years.2 However, concerns about potential risks to the fetus have limited the use of antidepressants during pregnancy. Therefore, it is crucial for physicians to understand and weigh the risks and benefits of antidepressant use during pregnancy when making prescription decisions.3 In treating women with mental illness during pregnancy, clinicians should stay updated on objective data from the medical literature and should pay mindful of their personal biases.4
A recent review highlighted inconsistencies in knowledge, attitudes, and decision-making among healthcare providers in different studies. It emphasized the need for improved dissemination of evidence-based treatments and increased training in psychopharmacology relevant to pregnancy and breastfeeding. The review cited findings from different studies that reported about 70% of physicians reading relevant scientific literature or engaging in additional training or conferences on the subject, but many healthcare providers expressed a desire for further training.5 A qualitative study conducted among psychiatrists in Scotland concluded that there is uncertainty among psychiatrists when prescribing for mothers, highlighting the importance of additional training in this area for psychiatrists, and the inclusion of perinatal psychiatry in the psychiatry training curriculum.6 In India, up to 71% of psychiatrists surveyed reported receiving some education about psychopharmacology during pregnancy as part of their training.7 In Australia, between 29% and 56.1% of healthcare providers reported having adequate training related to antidepressant use during pregnancy.8 Many healthcare providers also reported encountering incorrect information regarding the safety of antidepressants during pregnancy.5
This study aimed to gather baseline information about the confidence of psychiatrists in Oman regarding antidepressant use during pregnancy and breastfeeding, their knowledge and need for further training in this area, and their current prescribing patterns and preferences.
Methods
This survey was conducted between May and June 2017 and included all practitioners in the psychiatry specialty, including medical officers authorized to prescribe medications. The study was conducted at two tertiary care centers in Oman, Sultan Qaboos University Hospital, Behavioral Medicine Department, and Al Masarra Hospital. These centers provide psychiatric outpatient and inpatient services to patients from across the country and are also the main training centers for medical students and postgraduate psychiatric residents in Oman.
A questionnaire was specifically designed for the purpose of this study, based on available guidelines in the literature. The questionnaire included questions about the respondents' designation and experience in perinatal psychiatry. The respondents were asked to rate their confidence in prescribing antidepressants during the perinatal period, their perception of the need for more training in perinatal psychiatry, and whether they believed more training in perinatal psychiatry should be included in the psychiatry curriculum. The rating was based on a Likert-type scale including strongly agree, agree, neutral, disagree, and strongly disagree. Additionally, there were eight multiple choice questions that allowed respondents to provide more than one answer if required from the list of options given. These included drugs of choice during the first trimester of pregnancy, drugs avoided during the first trimester, reasons for choosing and avoiding antidepressants during pregnancy, drugs of choice during breastfeeding, drugs avoided during breastfeeding, and reasons for choosing and avoiding antidepressants in breastfeeding. The questionnaire was distributed to all the eligible participants.
The data were analyzed using the SPSS statistical software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). The categorical variables were presented as numbers and percentages.
This study was reviewed and approved by the Ethics Committee, College of Medicine and Health Sciences, Sultan Qaboos University (MREC#1438).
Results
A total of 42 practitioners (response rate = 89.4%) responded to the questionnaire, including two consultants, seven senior specialists, 12 specialists, three senior house officers, four medical officers, and 14 residents. Regarding experience in perinatal psychiatry, 10 (23.8%) participants had no experience, while one had experienced only during pregnancy, one had experience only during breastfeeding, and 30 (71.4%) had experience in prescribing during both pregnancy and breastfeeding periods. Approximately 64.3% (n = 27) of the participants felt confident in prescribing antidepressants for women during their perinatal period, while about 30.0% were neutral regarding their confidence in prescribing. Moreover, 35 (83.3%) participants expressed the need for more training in this area, and 34 (81.0%) believed that more training in perinatal psychiatry should be included in the psychiatry curriculum. The responses of specialists and above versus others (trainees) showed no statistically significant differences for three key items: confidence in prescribing antidepressants for women during their perinatal period (p = 0.100), the perceived need for more training in this area (p = 0.508), and the belief that more training is needed in perinatal psychiatry in the psychiatry curriculum (p = 0.412).
Figure 1 shows the proportion of participating practitioners who prescribed and avoided prescribing different types of antidepressants during the first trimester of pregnancy and breastfeeding periods.
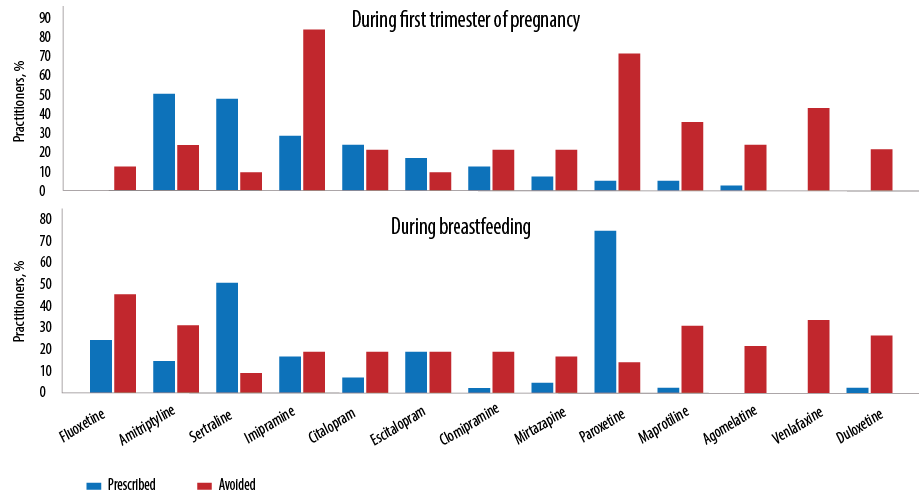 Figure 1: The proportion of participating practitioners who prescribed and avoided prescribing different types of antidepressants during the first trimester of pregnancy and breastfeeding periods.
Figure 1: The proportion of participating practitioners who prescribed and avoided prescribing different types of antidepressants during the first trimester of pregnancy and breastfeeding periods.
Fluoxetine was the drug of choice for approximately 85.0% of the practitioners during the first trimester of pregnancy but was avoided by 10.0% of practitioners in the same period. This was followed by amitriptyline (50.0% vs. 23.0%), sertraline (50.0% vs. 9.0%), imipramine (28% vs. 84.0%), citalopram (25.0% vs. 22.0%), escitalopram (18.0% vs. 9.0%), clomipramine (10.0% vs. 20.0%), and paroxetine (5.0% vs. 71.0%). Other drugs such as mirtazapine, maprotiline, and agomelatine were minimally prescribed, while venlafaxine and duloxetine were avoided.
During breastfeeding, the drug of choice was paroxetine in approximately 74.0% of the practitioners but was avoided by 15.0% of practitioners. This was followed by sertraline (50.0% vs. 8.0%). The prescribing patterns for other drugs were as follows: fluoxetine (23.0% vs. 45.0%), amitriptyline (14.0% vs. 30.0%), imipramine (16.0% vs. 17%.0), citalopram (5.0% vs. 18.0%), escitalopram (18.0% vs. 18.0%), and clomipramine (1.0% vs. 18.0%). Other drugs such as mirtazapine, maprotiline, and duloxetine were minimally prescribed, while agomelatine and venlafaxine were avoided.
Table 1 presents the most common reasons for choosing or avoiding the prescription of different types of antidepressants during pregnancy and breastfeeding. Safety, evidence-based practice, and low teratogenicity were the most common reasons for prescribing antidepressants during pregnancy. For breastfeeding, the main reasons for prescription were low levels of the drug in breast milk, safety, and evidence-based practice. On the other hand, high teratogenicity, neonatal side effects, limited data, and lack of evidence were among the most common reasons for avoiding prescription during pregnancy. During the breastfeeding period, high levels of breast milk, neonatal side effects, limited evidence, and safety concerns were the most common reasons for avoiding antidepressant prescriptions. Among the respondents, three (7.1%) participants who had no psychiatric experience in prescribing reported that they would avoid prescribing antidepressants during pregnancy, as did 11 (26.2%) practitioners during breastfeeding. Additionally, one of the participants reported prescribing antidepressants because they had observed other doctors doing so.
Table 1: Reasons for choosing and avoiding prescribing different types of antidepressants during pregnancy and breastfeeding among mental health practitioners (n = 42).
|
Safety
|
37 (88.1%)
|
Low levels in breast milk
|
30 (71.4%)
|
|
Evidence-based
|
31 (73.8%)
|
Safe
|
24 (57.1%)
|
|
Low teratogenicity
|
31 (73.8%)
|
Evidence-based
|
22 (52.4%)
|
|
Well tolerated by mother
|
13 (31.0%)
|
Less neonatal side effects
|
16 (38.1%)
|
|
Can be continued to breastfeeding
|
10 (23.8%)
|
Effective
|
11 (26.2%)
|
|
Efficacy
|
9 (21.4%)
|
Well tolerated by mother
|
8 (19.0%)
|
|
Experience
|
8 (19.0%)
|
All antidepressants have low risk
|
4 (9.5%)
|
|
Few drug interactions
|
3 (7.1%)
|
Practitioner experience
|
3 (7.1%)
|
|
Seen other doctors
|
1 (2.4%)
|
Low risk of overdose
|
2 (4.8%)
|
|
|
As for pregnancy
|
2 (4.8%)
|
|
|
Seen other doctors use it
|
1 (2.4%)
|
|
High teratogenicity
|
28 (66.7%)
|
High levels of breast milk
|
30 (71.4%)
|
|
Neonatal side effects
|
26 (61.9%)
|
Neonatal side effects
|
29 (69.0%)
|
|
Limited data
|
25 (59.5%)
|
Limited evidence
|
19 (45.2%)
|
|
Evidence-based
|
21 (50.0%)
|
Unsafe
|
19 (45.2%)
|
|
Unsafe
|
19 (45.2%)
|
Limited practitioner experience
|
11 (26.2%)
|
|
Obstetric complications
|
13 (31.0%)
|
Maternal side effects
|
9 (21.4%)
|
|
Toxic in overdose
|
8 (19.0%)
|
Toxic in overdose
|
5 (11.9%)
|
|
No practitioner experience
|
3 (7.1%)
|
Cardiotoxicity
|
5 (11.9%)
|
Discussion
This is the first study in Oman to investigate psychiatrists’ attitudes toward prescribing antidepressants during pregnancy and breastfeeding. The findings revealed no consistent prescribing patterns among the participating practitioners during the first trimester of pregnancy and breastfeeding. For instance, discrepancies were observed in the prescription and avoidance of drugs like fluoxetine, amitriptyline, and imipramine. Similar contrasting patterns were observed regarding the prescribing and avoidance of paroxetine during breastfeeding. This variation may be attributed to the difference in experience levels, with half of the respondents being senior and experienced while the other half were less experienced, including senior house officers, medical officers, and residents. It is concerning that a small number of practitioners with no psychiatric experience in prescribing during pregnancy and breastfeeding reported avoiding the prescription of antidepressants. Additionally, one participant mentioned prescribing antidepressants based on the observation of other doctors doing so. Although the numbers were small, this raises concerns about the safety of their practices. It is important to note that the choice of antidepressants for practitioners is sometimes limited by availability in the treating center. For example, while both fluoxetine and paroxetine were available at both sites, sertraline, which is approved for use during pregnancy and breastfeeding, was not available. These findings emphasized the need for training in this area of practice. Furthermore, considering the erosion of the ‘chemical depletion hypothesis’ for depressive illness and the observed poor efficacy of antidepressants as documented in recent systematic reviews, judicious use of such compounds during pregnancy and breastfeeding is warranted.9
Our study replicates the findings of a study by Kean et al,6 conducted in Scotland on prescribing antidepressants for mothers among psychiatrists. The response rate in our study was higher than that in the Scottish study (71.6%). In both studies, the majority of practitioners felt confident in prescribing and expressed the need for training and more training in this area. Both studies also found that the majority favored fluoxetine but avoided paroxetine during pregnancy. Interestingly, our study identified some participants who still recommend using paroxetine during pregnancy, despite international guidelines and other studies highlighting its risk of causing congenital cardiac defects.3 Imipramine has been documented to be relatively safe during pregnancy and lactation.10 Although it was one of the most chosen drugs during pregnancy in the Scottish study,6 it was among the most avoided antidepressants in our study due to the cardiac toxicity and other side effects associated with tricyclic antidepressants, to which imipramine belongs.11 However, in both studies, the majority recommended avoiding paroxetine during pregnancy. Both our study and the Scottish study found that paroxetine and sertraline were the antidepressants of choice during breastfeeding.6 While the choice of antidepressants was similar to that observed in the Scottish study, the proportion of participants prescribing these drugs was higher in our study. The reasons for this discrepancy are unclear. In both studies, fluoxetine was the most avoided drug during lactation, and participants decided to prescribe or avoid specific antidepressants based on their presence in breast milk.
This study highlights the variability in the reasons for choosing and avoiding antidepressants during pregnancy and breastfeeding, as well as prescribing patterns. In the current era of evidence-based practice guidelines and protocols, addressing this discrepancy is crucial, and attributing it to seniority or experience levels cannot be justified.
Conclusion
There was inconsistency among practitioners in making prescription decisions and in their prescribing patterns. Urgent measures are needed to improve training in perinatal mental health for psychiatrists and to incorporate perinatal psychiatry into the curriculum of psychiatry training.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Kean LJ, Hamilton J, Shah P. Antidepressants for mothers: what are we prescribing? Scott Med J 2011 May;56(2):94-97.
- 2. Cooper WO, Willy ME, Pont SJ, Ray WA. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol 2007 Jun;196(6):544.e1-544.e5.
- 3. Robinson GE. Controversies about the use of antidepressants in pregnancy. J Nerv Ment Dis 2015 Mar;203(3):159-163.
- 4. Vemuri M. Ethics commentary: ethical considerations in treating women with mental illness during pregnancy. Focus 2012 Jan;10(1):36-40.
- 5. Eakley R, Lyndon A. Antidepressant use during pregnancy: knowledge, attitudes, and decision-making of patients and providers. J Midwifery Womens Health 2022 May;67(3):332-353.
- 6. Kean LJ, Pasupuleti P, Shah P. Antidepressants for mothers: what are psychiatrists prescribing? Scott Med J 2013 Nov;58(4):228-233.
- 7. Godbole K, Vehale M, Phadke S. A survey among psychiatrists regarding psychotropic drug use in reproductive age women. Asian J Psychiatr 2011 Dec;4(4):272-276.
- 8. Williams S, Bruxner G, Ballard E, Kothari A. Prescribing antidepressants and anxiolytic medications to pregnant women: comparing perception of risk of foetal teratogenicity between Australian obstetricians and gynaecologists, speciality trainees and upskilled general practitioners. BMC Pregnancy Childbirth 2020 Oct;20(1):618.
- 9. Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry 2022 Jul:1-4.
- 10. Misri S, Sivertz K. Tricyclic drugs in pregnancy and lactation: a preliminary report. Int J Psychiatry Med 1991;21(2):157-171.
- 11. Wilson K, Mottram P. A comparison of side effects of selective serotonin reuptake inhibitors and tricyclic antidepressants in older depressed patients: a meta-analysis. Int J Geriatr Psychiatry 2004 Aug;19(8):754-762.