A 32-year-old female patient, para 2 living 2, with both vaginal deliveries, was presented to the outpatient department with complaints of urgency and increased frequency of micturition after one week of insertion of copper-T at a primary health center. She was referred to a higher center for further management. Her urine routine microscopic analysis was suggestive of 25–30 pus cells/hpf with absent bacteria. On per speculum examination, the copper-T thread was not seen from the cervical os. With the help of a copper-T removal hook, uterine probing was performed for the copper-T’s location but could not be felt. Per vaginal examination revealed a normal-sized, anteverted uterus, with free bilateral fornices and no forniceal tenderness.
On transvaginal ultrasonography, the copper-T was not seen in the uterine cavity, and the patient did not report a history of spontaneous expulsion. The diagnosis of a misplaced intrauterine device (IUD) was made, as the uterine cavity was empty. A whole abdominal scan and pelvic scan with a full urinary bladder were conducted to locate the copper-T [Figure 1].
 Figure 1: Ultrasound scan revealing the location of the copper-T located in the cavity of the organ anterior to the uterus.
Figure 1: Ultrasound scan revealing the location of the copper-T located in the cavity of the organ anterior to the uterus.
Question
- Where is the copper-T?
a. Cervix.
b. Urinary bladder.
c. Peritoneal cavity.
d. Bowel.
Answer
b. Urinary bladder.
The patient had complained of micturition, with no difference in symptoms upon postural changes. This has raised suspicions of the migration of the copper-T to the bladder. We directed our search for the misplaced copper-T to the urinary bladder. A transvaginal scan was performed with a full bladder, and to our surprise, the copper-T was located in the urinary bladder. Upon detailed examination, the vertical stem of the copper-T was found in the urethra [Figure 2], and a thread-like structure was visualized extending from the urethra [Figure 3]. The copper-T thread was grasped with artery forceps, and under the guidance of ultrasonography, the copper-T was gently and cautiously extracted to prevent injury to the urethra [Figure 3].
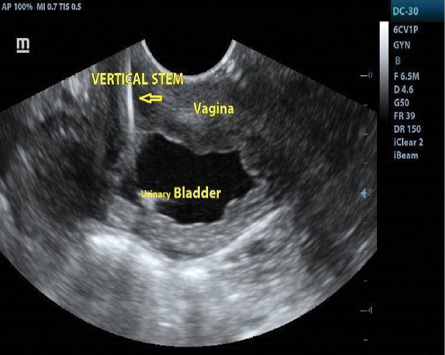 Figure 2: The vertical limb of copper-T is seen inside the urethra and horizontal limbs at the urinary bladder neck.
Figure 2: The vertical limb of copper-T is seen inside the urethra and horizontal limbs at the urinary bladder neck.
 Figure 3: Retrieval of the copper-T.
Figure 3: Retrieval of the copper-T.
Discussion
The copper-T is widely popular and one of the most accepted forms of contraception worldwide. It is inserted as an outpatient procedure, does not interfere with sexual activity, does not require anesthesia like tubal ligation, and is primarily carried out at easily accessible primary healthcare centers. It also involves minimal follow-ups.
However, complications have also increased due to the widespread nature of IUD insertion procedures. The rarer and more dangerous complications, such as the misplaced copper-T, are referred to tertiary care centers.
The incidence of the ‘missed string’ complication is 5%, and migration of the IUD outside the uterus to the bladder, sigmoid, and peritoneal cavity is rare but can lead to serious complications.1 We present a case of a misplaced IUD, which was referred due to urinary complaints after IUD insertion, and the copper-T was found in the urinary bladder. Prompt diagnosis using imaging techniques and appropriate treatment is crucial to prevent further complications. Similar cases have been noted in the literature, which can be detected using various imaging methods like hysterosalpingography, ultrasonography, and X-ray pelvis.2 Ultrasonography is especially important in diagnosing cases like ours, where the copper-T has migrated to the bladder.
The removal of the misplaced copper-T can be a challenging task. In our case, since the thread was protruding through the urethral meatus, retrieval was relatively straightforward. However, cystoscopy is often necessary for extracting the copper-T from the bladder. Additionally, instances of vesical stone formation around the copper-T have been reported in the literature, which can complicate matters to the extent that surgical procedures like suprapubic cystolithotomy are needed for removal.3 This can also result in the formation of vesicovaginal fistulas and vaginal calculi.4
While most misplaced IUD cases in the bladder are associated with a previous cesarean scar, in our case, the patient had undergone vaginal deliveries. This raises the suspicion that the healthcare worker may have mistaken the urethra for the cervical os during insertion.
In conclusion, patients should be counseled about regular follow-ups for their IUD devices and report immediately if they notice the thread is missing or misplaced. Diligent searching for misplaced IUDs is essential and should involve various imaging techniques to prevent the potentially severe complications associated with these long-standing intrauterine contraceptive devices. Special attention and training are required to avoid such complications.
Disclosure
The authors declared no conflicts of interest. Written consent was taken from the patient.
references
- 1. Marchi NM, Castro S, Hidalgo MM, Hidalgo C, Monteiro-Dantas C, Villarroeal M, et al. Management of missing strings in users of intrauterine contraceptives. Contraception 2012 Oct;86(4):354-358.
- 2. Vahdat M, Gorginzadeh M, Mousavi AS, Afshari E, Ghaed MA. Cystoscopic removal of a migrated intrauterine device to the bladder: a case report. Contracept Reprod Med 2019 Jul;4:7.
- 3. Ghanem MA, Sultan SM, Ghanem AA, Zanaty FM. Double intravesical migration of intrauterine device: presented with vesical stone formation. World J Nephrol Urol 2013 Nov;2(2):79-81.
- 4. Yan D, Shi Z, Wang L, Zhao X. Migration of a fractured ring IUD resulting in vesicovaginal fistula and vaginal calculus. Eur J Contracept Reprod Health Care 2018 Oct;23(5):387-389.