Osteoarthritis (OA) is the most common form of degenerative joint disease of the knees, hands, and hips.1–3 OA is a multifactorial disease with several demographic, genetic, and metabolic risk factors.2–4 Knee OA occurs when the cartilage within the knee joint begins to break down resulting in underlying bony changes. The process generally occurs gradually and worsens over time, resulting in joint-related pain, stiffness, swelling, and may eventually lead to disability.4,5 The global prevalence of OA has grown from 247.5 million cases in 1990 to 527.8 million in 2019, representing an increase of 113.3% over three decades; knee OA cases comprise nearly four-fifths of this burden.4 Malaysia is also facing an increasing prevalence of OA owing to factors such as the rising longevity and obesity in the population.6
The pharmacological treatments for knee OA include analgesia and intra-articular injections such as corticosteroids and viscosupplements.7 When these fail or become suboptimal, surgical interventions are the next modality of treatment. Not all individuals who require surgical interventions may be suitable for surgery due to underlying medical comorbidities and other risks.8 Some also resort to traditional and complementary medicine.9 For such patients, genicular nerve block (GNB) is a viable intervention that reduces pain by temporarily blocking the painful genicular nerve signals in the knee by injecting a local anesthetic.10–12
The four genicular nerve branches of the knee are the superomedial genicular nerve (SMGN), superolateral genicular nerve (SLGN), inferomedial genicular nerve (IMGN), and inferolateral genicular nerve (ILGN).13 Each lies on the bony surface connected to the periosteum, accompanied by its corresponding artery.11 The GNB generally targets only three of the four genicular nerves —the SMGN, SLGN, and IMGN. The ILGN is avoided because it is near the common peroneal nerve, which could lead to foot drop if accidentally infiltrated by local anesthesia. The SLGN courses around the femur shaft to pass between the vastus lateralis and the lateral epicondyle. It accompanies the superior lateral genicular artery.13 The SMGN courses around the femur shaft, following the superior medial genicular artery, to pass between the adductor magnus tendon and the medial epicondyle below the vastus medialis.13 The IMGN courses horizontally below the medial collateral ligament between the tibial medial epicondyle and the insertion of the collateral ligament and accompanies the inferior medial genicular artery.13
Traditionally, ALG has been the preferred method to target the nerves correctly to administer GNB to the knee, but is changing to modern guidance methods such as fluoroscopy and ultrasound-guided (USG) which promise greater accuracy.14 Though fluoroscopy clearly visualizes the bony landmarks for GNB, it risks exposing the patient to radiation. The USG aids in the visualization of the genicular arteries and sometimes the genicular nerves without radiation risk. The ALG technique can be used in clinical settings with no USG or fluoroscopy facilities. Several studies conducted internationally have found that administering GNB via either USG or ALG was able to reduce chronic knee pain and stiffness and improve functionality, and that among the two, USG was more beneficial to the patient.1,15
In Malaysia, no published study has determined or compared the effectiveness of GNB based on the guidance technique used. Generalizing international findings to a local context may be inaccurate due to differences in ethnic, sociodemographic, economic, and healthcare characteristics. Therefore, the primary objective of this study was to determine the effectiveness of ALG and USG techniques in administering GNB to treat chronic knee pain and stiffness and mitigate the functional limitations in patients suffering from OA of the knee. Our secondary objective was to compare the relative effectiveness of ALG and USG in achieving the above. Evidence from this study will help policymakers and clinicians to make evidence-based decisions on choosing the appropriate guidance technique to administer GNB, especially in settings with no to limited USG facilities.
Methods
This retrospective cohort study used the data available in the medical records of patients who received GNB for chronic knee OA in two major tertiary hospitals in northern Malaysia during July–August 2022, as well as their periodic questionnaire-based feedback (also extracted from the same medical records) during the post-treatment follow-up period from day one to six weeks. Prior evidence suggests that the effectiveness of GNB treatment in alleviating knee OA symptoms is generally noticeable during this timeframe. The patients were divided into two groups based on whether they received GNB via ALG or USG.
The sample size for the study was estimated using the Open Epi software version 3.01 (available at https://www.openepi.com/Menu/OE_Menu.htm). Wherein for the mean difference in Numeric Rating Scale (NRS-11) scores across both groups, the following parameters in Open Epi software were used α = 0.05, 80% power, and mean NRS-11 scores across both groups was 32.0±6.1 and 26.0±5.5, respectively based on a study by Cankurtaran et al.1 This estimated the required sample size = 30 with 15 in each group [Table 1]. For the mean difference in the Western Ontario and McMaster Universities Osteoarthritis Index Questionnaire (WOMAC) scores across both groups, the following parameters in Open Epi software were used: α = 0.05, 80% power, and mean WOMAC scores across each group were 1.2±0.7 and 2.1±0.9, respectively based on a study by Cankurtaran et al.1 The estimated sample size increased to 32 with 16 in each group [Table 2]. Adding an attrition rate of 20%, the final sample size was determined as 40 with 20 in each group, which was compatible with similar previous studies.1,15
Table 1: Sample size based on Numeric Rating Scale (NRS-11) score difference using Open Epi software version 3.
|
CI (2-sided)
|
95%
|
|
|
|
Power
|
80%
|
|
|
|
Ratio of sample size (Group 2/group 1)
|
1
|
|
|
|
Mean (SD)
|
32.0 (6.1)
|
26.0 (5.1)
|
6.0
|
|
Variance
|
37.21
|
30.25
|
|
*Difference between the means.
Table 2: Sample size based on the Western Ontario and McMaster Universities Osteoarthritis Index Questionnaire (WOMAC) score difference using Open Epi software version 3.
|
CI (2-sided)
|
95%
|
|
|
|
Power
|
80%
|
|
|
|
Ratio of sample size (Group 2/group 1)
|
1
|
|
|
|
Mean (SD)
|
1.2 (0.7)
|
2.1 (0.9)
|
-0.9
|
|
Variance
|
0.51
|
0.92
|
|
*Difference between the means.
The study participants were selected using simple random sampling. First, data with respect to all patients receiving GNB for the treatment of chronic knee OA from July 2022 to August 2022 were retrieved from the hospital's electronic medical record system. The inclusion criteria required the participants to be aged between 50 and 80 years and suffering from chronic knee pain of radiological tibiofemoral OA Kellgren-Lawrence grade 2–4 for more than three months.16 Excluded were patients who had knee pain of less than three months duration; had received intraarticular knee injection during the preceding three months; had undergone knee surgery; or had underlying inflammatory arthritis, connective tissue disease, spinal pathology, polyneuropathy, or neurological disorders. The patients meeting the eligibility criteria were then categorized into two groups based on whether ALG or USG was the mode of GNB administration. From each group, 20 patients were selected using the @RAND function in Microsoft Excel, a simple random sampling method. The study flow chart is shown in Figure 1.
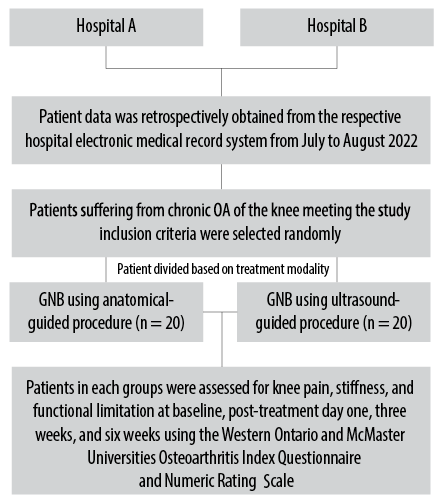 Figure 1: Flow chart depicting participant selection process.
Figure 1: Flow chart depicting participant selection process.
All data was sourced from the electronic medical records systems of the respective hospitals using a data collection form. We extracted data relating to patient sociodemographic, clinical, and intervention information such as sex, age in years, body mass index, duration of knee OA, underlying comorbidities, Kellgren Lawrence osteoarthritis grade, the mode of guidance (USG or ALG) to administer GNB, and post GNB complications. The data extracted also included the patient’s subjective assessment of the overall knee pain, stiffness, functional limitation score, recorded on four occasions—at baseline and post GNB procedure intervals at one day, end of three weeks, and end of six weeks—by clinic interviews. Knee pain, stiffness, and functional limitation scores were assessed using the recorded patient responses to the questionnaires WOMAC and NRS-11, both of which are reliable and valid instruments to assess pain scores of knee OA sufferers.17,18 In this study, the overall WOMAC score was used to represent the overall knee pain, stiffness, and functional limitation. The pain intensity was assessed using the NRS-11 score where 0 = no pain and 10 = maximum pain.17
The injections were delivered to the patient in a supine position. The GNB injection solution comprised 2 mL of lignocaine 2%, 5 mL of bupivacaine 0.5%, adrenaline (1:200 000), and 2 mL of triamcinolone acetonide (20 mg). The total injection volume per knee was 9 mL, with each injection site receiving 3 mL using a Vygon 22 G × 50 mm Echoplex+ needle (Ref 6194.503, France). No analgesia or sedative was administered before the procedure.
For administering GNB using the ALG technique, we followed the procedure described by Cankurtaran et al.1 Initially, three lines were drawn with a surgical marking pen to determine the injection points. With the knee in full extension, the first line was drawn longitudinally through the fibular head extending superiorly along the femur to a level 4 cm superior to the tip of the lateral femoral epicondyle. The second line was drawn horizontally between the medial and lateral femur epicondyles. Lastly, a third line was drawn from the femur medial epicondyle to the tibial medial epicondyle [Figure 2]. As local anesthesia, 1 mL of 2% lignocaine was given at the skin of each target point. The GNB injection needle was then advanced into the point for SMGN, SLGN, and IMGN deep enough to contact the underlying bone. Following this the needle was slightly retracted, aspiration was done to confirm the position and the injection was administered.
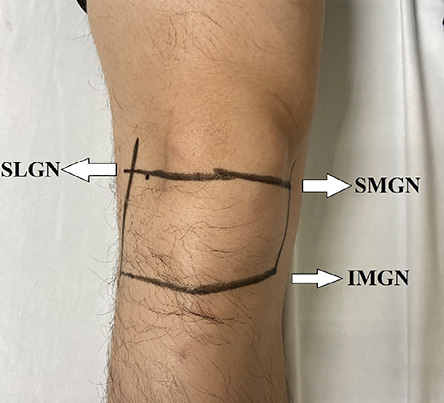 Figure 2: Anterior view of the right knee showing the lines drawn for the anatomical landmark guided technique to deliver genicular nerve block which consists of injections targeting the superomedial genicular nerve (SMGN), superolateral genicular nerve (SLGN), and inferomedial genicular
Figure 2: Anterior view of the right knee showing the lines drawn for the anatomical landmark guided technique to deliver genicular nerve block which consists of injections targeting the superomedial genicular nerve (SMGN), superolateral genicular nerve (SLGN), and inferomedial genicular
nerve (IMGN).
To administer GNB using the USG technique, we used a 12-MHz linear transducer (LOGIQ e; GE Medical Systems China Co., Ltd). The transducer was wrapped in a sterile covering. With the knee flexed over a pillow, the transducer was first placed on the junctions between the shaft of the femur, and medial and lateral epicondyles of femur, and junction between the shaft of tibia and the tibia epiphysis. The transducer was then moved proximally and distally to identify the genicular arteries near the periosteum. This was confirmed by color Doppler USG. The SLGN, SMGN, and IMGN travel alongside their respective genicular arteries as depicted in Figures 3 and 4.15 Local anesthetic (1 mL of 2% lignocaine) was given subcutaneously at each target point. The GNB needle was inserted along the long axis of the transducer using the in-plane technique. Once the needle tip was next to the genicular artery, aspiration was done to confirm the position and the injection was administered.
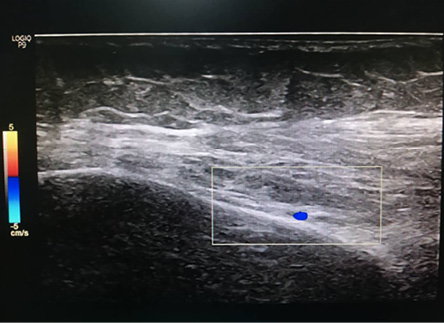 Figure 3: Ultrasound image of the superomedial genicular artery in the coronal plane.
Figure 3: Ultrasound image of the superomedial genicular artery in the coronal plane.
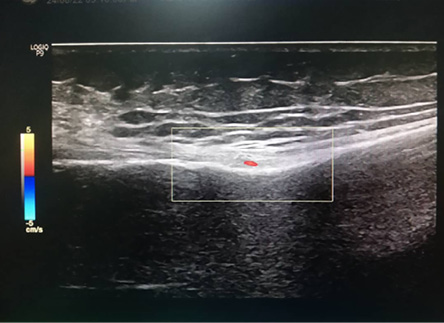 Figure 4: Ultrasound image of the inferomedial genicular artery in the coronal plane.
Figure 4: Ultrasound image of the inferomedial genicular artery in the coronal plane.
The data was analyzed using the IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). After subjecting to preprocessing, which ensured there were no missing, duplicate, or abnormal values, the data was analyzed descriptively using percentages and frequencies for categorical variables and mean SD for continuous variables.
Dependent t-test was used to determine the reductions in WOMAC and NRS-11 scores post-treatment day one, week three, and week six, respectively compared to baseline pain scores among all patients and compared the two groups based on their GNB administration technique. Significance was set at p < 0.05. The assumption of dependent t-test was tested prior to analysis to ensure all assumptions were sufficiently satisfied. These include the assumption of (a) normality in the differences between the dependent variables which was tested using the Shapiro–Wilk test, wherein p-values < 0.05 indicated a normal distribution; (b) the dependent variable was measured on a continuous scale; and (c) presence of outliers in the dependent variable was tested using box plots, wherein values beyond the upper and lower quartile limits of the interquartile range were considered as outliers.
An independent t-test was used to determine the difference in WOMAC and NRS-11 scores between both groups (GNB administration technique) at day one, week three, and week six, respectively. The independence of observation and homogeneity of variance between the two groups were verified using chi-square and Levene’s tests.
Results
The participants consisted of N = 40 patients comprising 20 each of males and females. Their mean age was 68.2 year and mean body mass index level 29.9. They were suffering from OA for a mean period of 86.8 months, and the condition of 82.5% was categorized at Kellgren Lawrence grade 4. The majority (62.5%) of the subjects had underlying comorbidities. Only one patient had a complication post-procedure (hypopigmentation at the injection site). Twenty participants underwent GNB via USG and the other 20 via ALG. Table 3 summarizes the characteristics of the study participants and demonstrates that there were no significant differences between the two groups.
Table 3: Comparative characteristics of the anatomical landmark-guided (n = 20) ultrasound-guided
(n = 20) participants.
|
Sex
|
|
|
|
|
|
Male
|
20 (50.0)
|
11 (55.0)
|
9 (45.0)
|
0.527
|
|
Female
|
20 (50.0)
|
9 (45.0)
|
11 (55.0)
|
|
|
Age, mean (SD), years
|
68.2 (8.5)
|
71.2 (7.3)
|
65.1 (8.7)
|
0.195
|
|
BMI, mean (SD), kg/m2
|
29.9 (4.1)
|
29.5 (3.7)
|
30.3 (4.5)
|
0.378
|
|
Osteoarthritis, mean (SD), months
|
86.8 (74.2)
|
82.5 (88.5)
|
91.2 (58.6)
|
0.327
|
|
Kellgren Lawrence grade
|
|
|
|
|
|
3
|
7 (17.5)
|
2 (10.0)
|
5 (25.0)
|
0.212
|
|
4
|
33 (82.5)
|
18 (90.0)
|
15 (75.0)
|
|
|
Comorbidity
|
|
|
|
|
|
Yes
|
25 (62.5)
|
15 (75.0)
|
10 (50.0)
|
0.102
|
|
No
|
15 (37.5)
|
5 (25.0)
|
10 (50.0)
|
|
|
Post GNB complication
|
|
|
|
|
|
Yes
|
1 (2.5)
|
1 (5.0)
|
0 (0.0)
|
0.311
|
Chi-square test was used for categorical variables and Independent t-test for continuous variables. BMI: body mass index; GNB: genicular nerve block.
For the entire cohort (N = 40), the mean WOMAC score (representing pain, stiffness, and function) was 52.4 at baseline, and fell sharply to 27.4 on post treatment day one, representing 47.7% of symptom-reduction. By the end of week three, the mean score had risen slightly to 30.3 (representing 42.2% of post-treatment symptom reduction) and at the end of week six to 34.5 (34.2% of post-treatment decline). The mean pain scores as assessed by the NRS-11 scale were 7.0, 3.1, 4.4, and 4.8 at baseline, post-treatment day one, three weeks, and six weeks, respectively. Pain scores reduced by 55.7% (day one post-treatment), 37.1% (three weeks post-treatment), and 31.4% (six weeks post-treatment) [Table 4 and Figure 5].
Table 4: Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and Numeric Rating Scale (NRS-11) scores at baseline and post-treatment intervals (day one, three weeks, and six weeks).
|
A. All patients (n = 40)
|
|
WOMAC
|
52.4 (14.7)
|
27.4 (15.3)
|
11.3
(< 0.001)
|
30.3 (15.3)
|
8.1 (< 0.001)
|
34.5 (18.4)
|
6.8
(< 0.001)
|
|
NRS-11
|
7.0 (1.3)
|
3.1 (1.8)
|
14.7
(< 0.001)
|
4.4 (2.1)
|
8.4 (< 0.001)
|
4.8 (2.3)
|
6.7
(< 0.001)
|
|
B. Anatomical landmark guided GNB group (n = 20)
|
|
WOMAC
|
54.6 (16.0)
|
31.8 (18.5)
|
6.1 (< 0.001)
|
29.1 (16.5)
|
6.0 (< 0.001)
|
40.1 (22.2)
|
3.2
(< 0.004)
|
|
NRS-11
|
7.1 (1.5)
|
2.9 (2.1)
|
9.4 (< 0.001)
|
4.5 (2.5)
|
4.5 (< 0.001)
|
5.1 (2.4)
|
3.5
(< 0.002)
|
|
C. USG guided GNB group (n = 20)
|
|
WOMAC
|
50.3 (12.4)
|
22.9 (9.9)
|
12.0
(< 0.001)
|
31.5 (14.3)
|
5.4 (< 0.001)
|
28.2 (10.6)
|
7.6
(< 0.001)
|
*Comparison post treatment intervals with baseline WOMAC and NRS-11 scores, wherein significance is set at p < 0.05; t denotes the dependent t statistic.
GNB: genicular nerve block; USG: ultrasound-guided.
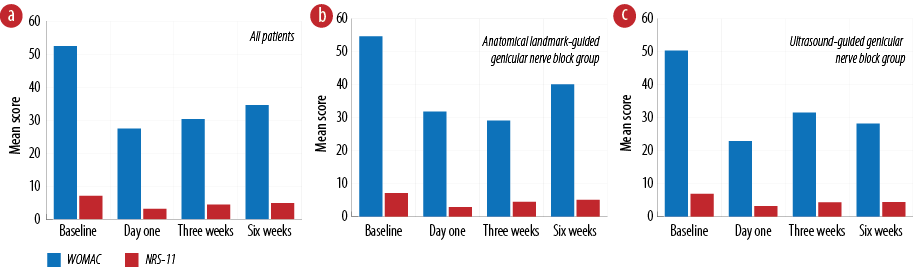 Figure 5: Western Ontario and McMaster Universities Osteoarthritis Index Questionnaire (WOMAC)
Figure 5: Western Ontario and McMaster Universities Osteoarthritis Index Questionnaire (WOMAC)
and Numeric Rating Scale (NRS-11) score comparison at baseline and post-treatment intervals among
(a) all patients, (b) anatomical landmark-guided (n = 20), and (c) ultrasound-guided (n = 20) participants. (lower scores represent more relief experienced by the patient).
The comparative reductions in mean WOMAC scores between the USG and ALG groups are listed in Table 4 (sections B and C) and in sub-charts b and c in Figure 5. For the ALG group, WOMAC scores reduced by 41.7% (post-treatment day one), 46.7% (post-treatment three weeks), and 26.6% (post-treatment six weeks) compared to baseline pain score. For the USG group, WOMAC scores reduced by 54.5% (post-treatment day one), 37.4% (post-treatment three weeks), and 43.9% (post-treatment six weeks).
The comparative Groupwise breakup of NRS-11 scale results is also given in Table 4 (scale C) and Figure 4 (b and c) pain scores reduced by 59.2% (post-treatment day one), 36.6% (post-treatment three weeks), and 28.2% (post-treatment six weeks). For the USG group, pain scores reduced by 53.6% (post-treatment day one), 37.7% (post-treatment three weeks), and 36.2% (post-treatment six weeks).
The overall pain, stiffness, and functional limitation scores assessed using the WOMAC scale reported a greater reduction in mean overall pain, stiffness, and functional scores of 8.9 at post-treatment day one and 12.8 at six weeks among those receiving GNB via USG than ALG. Pain scores assessed using the NRS-11 scale reported a greater reduction in mean pain scores of 0.3 and 0.7 at three weeks and six weeks post-treatment, respectively among those who receiving GNB via USG instead of ALG [Table 5]. Overall, higher reduction in mean WOMAC and NRS-11 scores was observed among the USG group than the AGL group, which became statistically significant six-weeks post-treatment (p = 0.026).
Table 5: Comparison of Western Ontario and McMaster Universities Osteoarthritis Index Questionnaire (WOMAC) and Numeric Rating Scale (NRS-11) scores between the ultrasound-guided (USG) and anatomical landmark guided (ALG) groups post-treatment.
|
Day one
|
ALG
|
WOMAC
|
31.8
|
8.9
|
0.065
|
|
USG
|
|
22.9
|
|
|
|
ALG
|
NRS-11
|
2.9
|
0.3
|
0.609
|
|
USG
|
|
3.2
|
|
|
|
Three weeks
|
ALG
|
WOMAC
|
29.1
|
2.4
|
0.627
|
|
USG
|
|
31.5
|
|
|
|
ALG
|
NRS-11
|
4.5
|
0.3
|
0.669
|
|
USG
|
|
4.2
|
|
|
|
Six weeks
|
ALG
|
WOMAC
|
40.9
|
12.8
|
0.026**
|
|
USG
|
|
28.1
|
|
|
|
ALG
|
NRS-11
|
5.1
|
0.7
|
0.302
|
* Difference between the USG pain mean scores compared to ALG mean pain scores; **significance set at p < 0.005.
Discussion
This study determines the effectiveness of GNB in reducing knee pain, stiffness, and improving functional limitation among patients suffering from OA of the knee. We found that GNB treatment modality a significantly reduced knee pain, stiffness, and functional limitation scores by 34.2% to 47.7% for the WOMAC scale and reduced knee pain scores by 31.4% to 55.7% for the NRS-11 scale post-treatment compared to baseline scores among all patients. Similar findings have been reported by studies from Korea, Turkey, Spain, and the USA.1,15,16,19,20 Several reasons could attribute to this finding, the GNB treatment modality directly blocks the painful genicular nerve signals temporarily in the nerves that innervate the knee joint.10 GNB’s benefits are observed as soon as one-day post-treatment.21
Furthermore, this study found that the administration of GNB using the ALG technique had significantly reduced knee pain, stiffness, and functional limitation scores by 26.6% to 46.7% for the WOMAC scale and reduced knee pain by 28.2% to 59.2% for the NRS-11 scale post-treatment compared to baseline scores among all patients. While the administration of GNB using the USG technique had significantly reduced knee pain, stiffness, and functional limitation scores by 37.4% to 54.5% for the WOMAC scale and reduced knee pain scores by 36.2% to 53.6% for the NRS-11 scale post-treatment compared to baseline scores among all patients.
The post-treatment mean pain, stiffness, and functional limitations scores at day one, three weeks, and six weeks were significantly lower compared to the baseline score for the WOMAC and NRS-11 scale in all patients as well as in those who received USG and ALG techniques for GNB, maximum pain reduction being reported one-day post-treatment. At weeks three and six, the scores rose slightly, yet remained significantly below the baseline scores. The additive effect of both the short and long acting local anesthetic used in the GNB would result in the highest pharmacological efficacy immediately post-administration.22 With the passing of time, the waning effects of the short-term analgesic may become apparent resulting in a lower reduction of pain scores at three and six weeks compared to one-day post-procedure.22 These findings provide evidence that the GNB treatment modality administered using both the ALG and USG techniques is effective in reducing knee pain, stiffness, and functional limitation at day one, three weeks, and six weeks post-treatment. This provides evidence to recommend GNB treatment in patients suffering from chronic knee OA.
This study found that administering GNB using the USG technique resulted in a greater reduction of pain, stiffness, and functional limitation compared to the ALG technique. This reduction, though consistently observed across each interval post-treatment, was significant only at six weeks post-treatment (p = 0.026). This is in line with previous studies whose results also pointed to the superiority of USG to ALG.1 One of the reasons for this is that USG facilitates accurate identification of genicular nerves readily, allowing for proper administration of GNB in a timely manner, thus reducing procedure time.1,23 In addition, the use of USG technique helps prevent damage to surrounding structures leading to lower procedural-related pain or complications; and also enables the detection of additional pathologies that may be difficult to detect or missed when using the ALG technique.1,23
GNB is considered a safe and low-risk procedure.1,23 The risks of GNB injection described in previous literature include infection, bleeding, neuroma formation, hypopigmentation, and allergic reactions.1 In this study, there was only one reported adverse effect which was hypopigmentation at the injection site in a patient from the ALG group. The comparison of the current findings with previous studies is shown in Appendix 1 and 2. The current study provides baseline data on the effectiveness of GNB in treating knee OA among the Malaysian population which to date is lacking. Therefore, the findings of this study add more data to the literature with regards to this topic. In addition, this study also provides closer follow-up intervals (three and six weeks) compared to other similar studies; and therefore, would yield additional valuable information to the existing body of evidence.
There are several limitations in this study, among them includes the use of a retrospective cohort design rather than a double-blind randomized design, which was due to personnel and budget constraints. The maximum duration of patient follow-up in the study was six weeks post-treatment. A longer follow-up period would have enabled the assessment of symptom-rebound or worsening of pain scores. Another limitation is the small sample size. Although the final sample size was extrapolated from statistical calculations, we were constrained by the limited number of available patients who met the inclusion criteria.
Despite these limitations, this study has its strengths. This is the first study in Malaysia to determine and compare the effectiveness of GNB administered using ALG and USG techniques in the treatment of chronic knee pain, stiffness, and improving functional limitation among patients suffering from OA of the knee. This study therefore bridges a gap in the literature and its findings should enable local clinicians to make timely and evidence-based decisions regarding the use of GNB treatment for chronic knee OA. In addition, the methodological strengths of this study include sampling patients from two hospitals which would increase the generalization of study findings. Sourcing data from official hospital electronic records and matching baseline characteristics among patients in both groups ensured that the samples were reliable and comparable.
Conclusion
GNB administration using either USG or ALG technique was effective in significantly reducing pain, stiffness, and functional limitation as soon as day one to six-week post-treatment among patients suffering from chronic knee OA. However, based on patient feedback, the USG technique appeared to be more effective than ALG in mitigating symptoms. Nevertheless, GNB administration based on ALG remains an effective modality, especially in healthcare settings with limited to no USG facilities.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgments
We would like to thank the Director General of Health Malaysia for granting permission to publish this article. Also, we would like to thank the respective hospitals who gave full cooperation during data collection.
references
- 1. Cankurtaran D, Karaahmet OZ, Yildiz SY, Eksioglu E, Dulgeroglu D, Unlu E. Comparing the effectiveness of ultrasound guided versus blind genicular nerve block on pain, muscle strength with isokinetic device, physical function and quality of life in chronic knee osteoarthritis: a prospective randomized controlled study. Korean J Pain 2020 Jul;33(3):258-266.
- 2. Al-Zadjali N, Al-Khaldi S, Samir N, Rizvi S, Al-Zakwani I, Al-Mahrezi A. Characteristics of chronic pain patients attending a primary health care center in Oman. Oman Med J 2017 Nov;32(6):461-466.
- 3. Al Saleh J, Sayed ME, Monsef N, Darwish E. The prevalence and the determinants of musculoskeletal diseases in Emiratis attending primary health care clinics in Dubai. Oman Med J 2016 Mar;31(2):117-123.
- 4. Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine 2020 Nov;29-30:100587.
- 5. Centre of Disease and Prevention. Osteoarthritis (OA). [cited 2022 October 19]. Available from: https://www.cdc.gov/arthritis/basics/osteoarthritis.htm#:~:text=Osteoarthritis.
- 6. Yeap SS, Abu Amin SR, Baharuddin H, Koh KC, Lee JK, Lee VK, et al. A Malaysian Delphi consensus on managing knee osteoarthritis. BMC Musculoskelet Disord 2021 Jun;22(1):514.
- 7. Crawford DC, Miller LE, Block JE. Conservative management of symptomatic knee osteoarthritis: a flawed strategy? Orthop Rev (Pavia) 2013 Feb;5(1):e2.
- 8. Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, et al. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg 2008 Dec;51(6):428-436.
- 9. Nik Shafii NA, Yaacob LH, Ishak A, Kadir AA. Traditional and complementary medicine use in knee osteoarthritis and its associated factors among patients in Northeast Peninsular Malaysia. Oman Med J 2018 Mar;33(2):148-153.
- 10. Lebleu J, Fonkoue L, Bandolo E, Fossoh H, Mahaudens P, Cornu O, et al. Lower limb kinematics improvement after genicular nerve blockade in patients with knee osteoarthritis: a milestone study using inertial sensors. BMC Musculoskelet Disord 2020 Dec;21(1):822.
- 11. Conger A, Gililland J, Anderson L, Pelt CE, Peters C, McCormick ZL. Genicular nerve radiofrequency ablation for the treatment of painful knee osteoarthritis: current evidence and future directions. Pain Med 2021 Jul;22(Suppl 1):S20-S23.
- 12. Santana-Pineda MM, Vanlinthout LE, Santana-Ramírez S, Vanneste T, Van Zundert J, Novalbos-Ruiz JP. A randomized controlled trial to compare analgesia and functional improvement after continuous neuroablative and pulsed neuromodulative radiofrequency treatment of the genicular nerves in patients with knee osteoarthritis up to one year after the intervention. Pain Med 2021 Mar;22(3):637-652.
- 13. The New York School of Regional Anesthesia. Genicular nerve blocks. 2022 [cited 2022 October 19]. Available from: https://www.nysora.com/techniques/lower-extremity/nysora-com-genicular-nerve-blocks/.
- 14. Yasar E, Kesikburun S, Kılıç C, Güzelküçük Ü, Yazar F, Tan AK. Accuracy of ultrasound-guided genicular nerve block: a cadaveric study. Pain Physician 2015;18(5):E899-E904.
- 15. Yilmaz V, Umay E, Gundogdu I, Aras B. The comparison of efficacy of single intraarticular steroid injection versus the combination of genicular nerve block and intraarticular steroid injection in patients with knee osteoarthritis: a randomised study. Musculoskelet Surg 2021 Apr;105(1):89-96.
- 16. Sotelo VG, Maculé F, Minguell J, Bergé R, Franco C, Sala-Blanch X. Ultrasound-guided genicular nerve block for pain control after total knee replacement: preliminary case series and technical note. Revista Española de Anestesiología y Reanimación (English Edition) 2017 Dec;64(10):568-576.
- 17. Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005 Jun;30(11):1331-1334.
- 18. Bilbao A, Quintana JM, Escobar A, Las Hayas C, Orive M. Validation of a proposed WOMAC short form for patients with hip osteoarthritis. Health Qual Life Outcomes 2011 Sep;9(1):75.
- 19. Kim D-H, Lee M-S, Lee S, Yoon S-H, Shin J-W, Choi S-S. A prospective randomized comparison of the efficacy of ultrasound- vs fluoroscopy-guided genicular nerve block for chronic knee osteoarthritis. Pain Physician 2019 Mar;22(2):139-146.
- 20. McCormick ZL, Korn M, Reddy R, Marcolina A, Dayanim D, Mattie R, et al. Cooled radiofrequency ablation of the genicular nerves for chronic pain due to knee osteoarthritis: six-month outcomes. Pain Med 2017 Sep;18(9):1631-1641.
- 21. Tas B, Akpinar P, Aktas I, Unlu Ozkan F, Kurucu IB. Effects of genicular nerve block in patients with knee osteoarthritis who have neuropathic or nociceptive pain. Ann Rheum Dis 2020;79(Suppl 1):788-789.
- 22. Taylor A, McLeod G. Basic pharmacology of local anaesthetics. BJA Educ 2020 Feb;20(2):34-41.
- 23. Sarı S, Aydın ON, Turan Y, Şen S, Özlülerden P, Ömürlü İK, et al. Which imaging method should be used for genicular nerve radio frequency thermocoagulation in chronic knee osteoarthritis? J Clin Monit Comput 2017 Aug;31(4):797-803.