| |
Abstract
Objective: The aim of this study was to assess the etiological characteristics and visual outcomes of ocular trauma with more attention to eyelid laceration.
Methods: In a cross-sectional study, 98 cases of isolated traumatic eyelid laceration were consecutively studied and its epidemiology, etiology and association with visual outcome were evaluated. The findings of this study could be used to develop healthcare related precautions and work place safety recommendations.
Results: Of the 98 patients included in the study, men exhibited a greater vulnerability and they were mostly aged around 29 years old. In terms of the place of trauma, 42 (42.8%) cases occurred in the street, 29 cases (29.6%) occurred at home, and 18 cases (18.4%) occurred at the workplace, while 5 cases (5.1%) happened in entertaining environments like parks. For 3 patients (3%), the incident took place at a public pathway, and in 1 patient (1%), the case occurred at school. As the most common cause of trauma, 41 patients (41.8%) had an object hit their eyes. In addition, assaults were a major cause of injury. The right eye and the upper lid were also the most common sites of injuries. Although no blindness occurred due to trauma causing eyelid laceration, the visual outcomes were correlated with severity of the incident defined based on the presence of open globe injuries.
Conclusion: This study could possibly highlight the risk factors of eyelid laceration and provide the healthcare community with the essential recommendations regarding the safety precautions in dangerous settings, including daily/routine work places.
Keywords: Eyelid laceration; Etiology; Epidemiology.
Introduction
Orbital and periorbital regions may be the subject of damage by many traumatic factors, not only affecting the site of direct injuries, but even developing more complications by penetrating the inner aspects of the head and face.1 Eye trauma related fields of research have earned much attention and interest during the last years. Although a lot of work has been done to determine more effective prevention and ideal management; there is still room to improve the etiology, demographics, causes, and clinical features of eye lid laceration.2
Although ocular trauma is of much importance to the health community, there is rarely a consensus on the epidemiological characteristics of this incident, especially noted outside the regions of developed nations.3,4 Acknowledging this to be one of the preventable health issues commonly seen around the world,3 it is important to address this issue in order to reduce its impact on the socioeconomics of the community.5
Among all sites of injury, eyelid laceration seems to be neglected in terms of sufficient epidemiological investigations. With a thorough understanding of the causes of eye lid lacerations, it is possible to develop a better preventive strategy and hence improve the public health policy in this respect. The aim of this case review was to identify the subjects at a greater risk of developing eyelid laceration, and to determine its etiological causes in order to facilitate the development of a preventive strategy to possibly decrease the prevalence of such trauma related incidents in high risk patients by providing work places with a series of safety precautions.
Methods
Between March 2007 and April 2009, patients attending the emergency department (ED) of Farabi Eye Hospital (one of the most referred eye hospitals in Tehran, capital of Iran) were consecutively enrolled in this case review study. Patients with any history of trauma to the eye lids were eligible for inclusion into the study. A questionnaire was completed for each case by the residing physicians at the ED, recording demographic data and other clinical findings. Each patient was evaluated by a first year resident of ophthalmology; and if needed, the case was referred to the chief resident for further assessment. Attending professors had the responsibility of supervising all complicated cases of laceration directly, or via phone calls in case of outpatient management.
As one of the most referred and excellent ophthalmologic care centers in the country, Farabi Eye Hospital is affiliated with Tehran University of Medical Sciences, located at the center of a highly prevalent area for traumatic eye injuries with high capability to manage the patients either in a clinical or emergency setting by outpatient and inpatient visits by the most experienced Ophthalmologists in the country.
The inclusion criteria were consisted of; any trauma to the eye involving lids or its margins. Patients with emergent conditions needing surgery were excluded. By using an identification code for each patient, access to the data related to the registered traumatic patients of lid laceration was possible. Lid laceration was defined as any trauma to the external surface of the lids with or without evident loss of tissue or other ocular co-morbidities; but absolutely with such significant symptom enforcing the patient to seek hospital care.
Informed consent was obtained from each patient and the related information was reassured to be kept confidential. Also, the declaration statement of Helsinki was followed throughout the process of the project. The Ethical and Research Committee of Tehran University of Medical Sciences approved the study and the project was carried out between 2007 and 2009. Data were analyzed using the Statistical Package for Social Service version 15 (SPSS, Chicago, Inc) and descriptive variables were reported as number (%).
Results
This study enrolled 98 patients, 24 (24.5%) females and 74 (75.5%) males, aged between 1 and 85 years old (mean ± SD age: 29.38 ± 17.82 years). Among the study participants, 26 ones (26.5%) were workers, 18 patients (18.4%) were housekeepers, 10 patients (10.2%) were employee, and 5 patients (5.1%) were unemployed and 20 patients (20.4%) were retired at the time of the study. Furthermore, 19 patients (19.4%) were children, and therefore not subject to any form of occupation. All of the studied patients were thoroughly conscious at the time of hospital admission (GCS=15/15).
In terms of the place of trauma, the incident occurred in city streets in 42 cases (42.8%), followed by 29 cases (29.6%) at home, 18 participants (18.4%) at the workplace, 5 cases (5.1%) at entertaining areas such as parks, while in 3 cases (3%), the incident occurred at a public pathway, and 1 (1%) incident was related to a child injured at school. In 41 patients (41.8%), a moving object hit the eyes, while motor vehicle accidents were the mechanism of trauma in 23 patients (23.5%), followed by 20 cases (20.4%) who reported falling to be the cause of the trauma, and assault was the cause of laceration in other 14 cases (14.3%). Furthermore, 61 patients (62.2%) reported the object causing ocular trauma to be blunt, while 36 cases (36.7%) described the object as a sharp one like broken glass. In terms of motor vehicle accidents, motorcycles were the cause in 16 cases (59.3%), and cars were responsible for the injury in 11 cases (40.7%).
Considering the characteristics of the lacerations, the right eye and upper eyelid were involved in 21 cases (21.4%), the left eye and upper eyelid were affected in 20 patients (20.4%), the right eye and lower eyelid reported by 18 cases (18.4%), while the right eye and both eyelids in were reported by 18 patients (18.4%), and the left eye and lower eyelid and the left eye and both eyelids were implicated in 11 (11.2%) and 8 (8.2%) cases, respectively. With respect to the length of laceration; the length of the laceration varied from 5 mm to 50 mm (mean ± SD: 18.81 ± 13.41) in the right eye and upper lid, the value ranged from 5-50 mm (mean ± SD: 20.19 ± 13.59) in the right eye and lower lid, and between 5 and 40 mm (mean ± SD: 18.81 ± 12.03) in the left eye and upper lid; moreover, the mean ± SD of laceration length was 19.23 ± 12.39, and ranged from 5 to 50 mm in the left eye and lower lid.
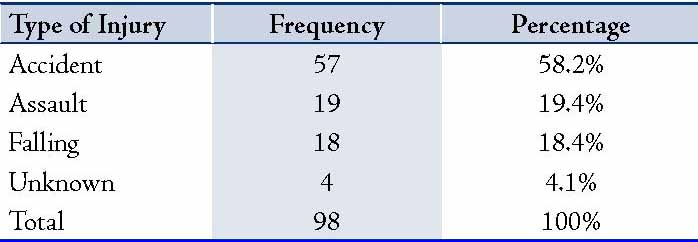
The depth of laceration was measured to be between 1 and 20 mm (mean ± SD of 6.08 ± 4.04 mm). Furthermore, the skin and subcutaneous tissue were affected in 90 cases (91.8%), while the skin, subcutaneous tissue and muscle were affected in 5 cases (5.1%), and 1 case (1%) was reported to have involve the septum. Of the 98 participants, tissue loss was reported in 4 cases (4.1%), while 93 cases (94.9%) reported laceration without any tissue loss; and overall, there was no case that needed to be repaired with grafts. The amount of tissue loss ranged from 0 mm to 10 mm (mean ± SD: 5.75 ± 5.05). Among all the studied subjects, there were no cases of upper or lower canalicular injuries. However, globe injury was reported in 6 (6.1%) cases, while no such injuries were noted in the remaining 92 patients (93.9%). In cases of globe injuries, 3 (3.1%) patient sustained microscopic injury, while laceration of the conjunctiva was noted in 3 (3.1%) patients. Also, orbital fracture was observed in 5 cases (5.1%), while there was no sign of orbital fracture in 92 cases (93.9 %); however, concomitant nasal fracture was apparent in 1 case. Moreover, only 5 cases (5.1%) showed signs of infection suggestive of cellulites. Based on the Snellen Scale, visual acuity of the right eye was as follows: in 87 patients (88.8%), the visual acuity was greater than 6/10 meter (m); while in 3 patients (3.1%), the visual acuity was less than 6/10 m. Similarly, visual acuity of the left eye was less than 6/10 m in 87 cases (88.8%), and more than 6/10 m in 3 cases (3.1%). Among these, there was no reported case of visual acuity of an eye less than 6/60 m (which is referred to as blinded). Hence, there was a significant decrease in association between visual acuity of both eyes with the severity of trauma defined based on the presence of globe injury (p<0.05). The type of injury based on the intention by which it occurred were as follows; the injury occurred accidentally in 57 cases (58.2%), injury resulted from assault in 19 cases (19.4%), the mechanism of trauma was as a result of falling in 18 cases (18.4%); and in 4 cases (4.1%), the cause of injury was unknown. (Table 1)
Table 1: Types of injuries classified by intention.
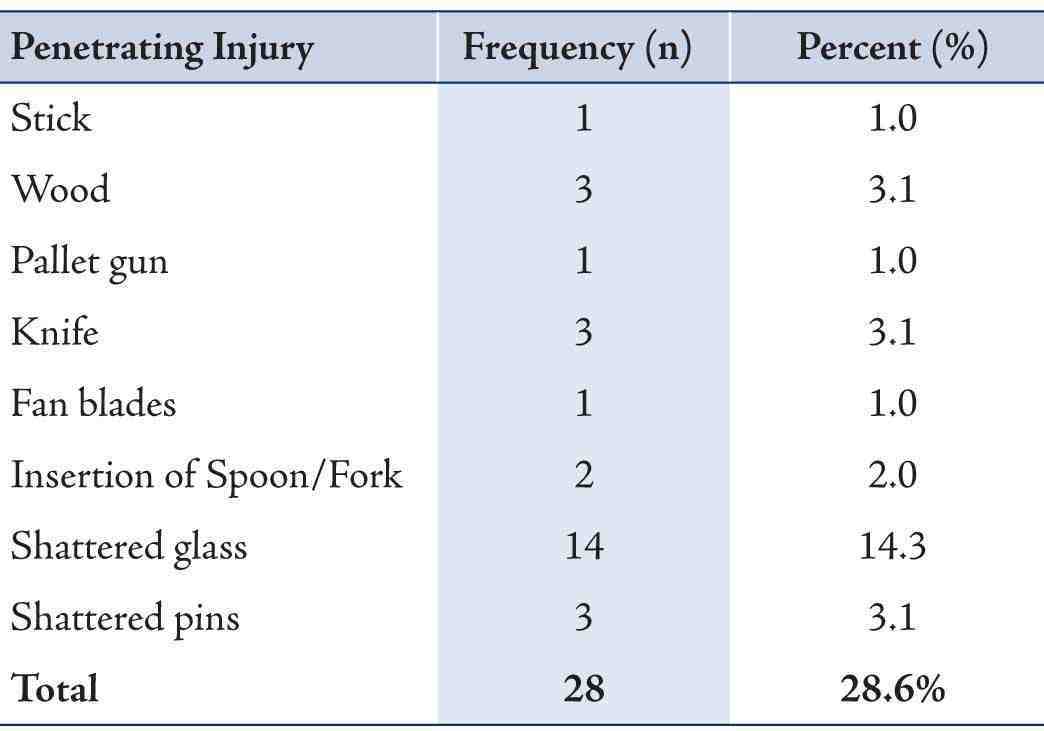
The characteristics of trauma and the underlying mechanisms are summarized in Tables 2 and 3; it indicates that the pellet gun was the cause of injury in 1 case (1%), followed by knife and shattered glass in 3 (3.1%) patients and 14 (14.3%) cases, respectively. In addition, violation was determined to be one of the major causes of injury, of which 2 cases (2%) were traumatized by the elbow, 7 cases (7.1%) by fist, and 2 cases (2 %) by foot during dual assaults, and 2 (2%) patients were reported to have hit the wall during the fight.
Table 2: Mechanisms of blunt trauma to the eyelids.
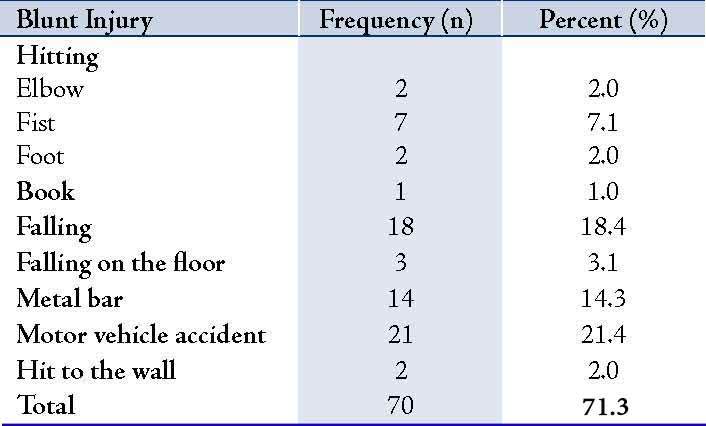
Table 3: Mechanisms of penetrating trauma to the eyelids.
Discussion
The aim of this study was to provide the evidence and grounds to encourage health policy decision makers to address the subject of traumatic eye injuries, eye lid lacerations in particular. The penetration of foreign bodies into the eyes is not the only cause of damage to either eye lids or its inner surfaces over the globe, whereby the removal of the object may potentially affect the vision or possibly other related structures.6 To our knowledge, we noted not a single study which was methodologically well designed which examined the epidemiology of eyelid laceration or at least has organized the population based findings; thus it would appear that such injury alone is not a matter of serious concern to the public health community. Most studies have addressed the capability of sharp objects like fishing hooks to penetrate the eye lids and the probable damage it would afflict on the cornea.7-10 But since there are no reports describing the impact of eyelid laceration on the social and economical health status,5 it is worth mentioning this matter in a more concise manner.
The results showed a greater prevalence for eyelid lacerations among male patients (75.5%) of active age (i.e., 29 years old in our society), most of whom were occupied at factories, workshops or were just workers in one form or another. This is totally consistent with other reports, in which ocular trauma was shown to be more prevalent among children, younger adults, men, and even of higher incident in less skilled workers.11-13 However, in contrast to the reports from developed countries with different social and cultural backgrounds, the results seem to be different.14,15 Similar to our study, a male predominance in globe injuries has been well documented universally.5,14,16-18 This could be due to the fact that men tend to occupy higher risk jobs, and are also involved in activities such as; operating motor vehicle with less safety and immunity and practicing vigorous sports. Men are also implicated in a higher rate of assaults or other violent crimes, and they even exhibit a lack of concepts of safety and caution at the work place. However, attention should be paid to the changing position of women’s roles outdoors and the subsequent alteration in predisposition of high risk conditions and related injuries.19-21
The study results revealed that the most common places where accidents occurred were the work place followed by the home; a finding which is in line with other reports.11,14,22,23 In the developing countries, it is well established that for women at home occupied with household chores, housekeeping duties and taking care of children, as well as other house related tasks; it is very difficult for them to pay attention to safety and immunity while performing such tasks. In addition, workers in Tehran are more likely to develop traumatic injuries including lid lacerations in a wide spectrum of jobs irrespective of the extensive safety policies put in place for the workplace environment; the importance seems to be based on how well it pays or how easily it is managed.
Moving objects, motor vehicle accidents, falling, and fighting were the main causes of lid lacerations in the study population. Other studies have also reported moving objects with blunt features to be the most common etiology of lid laceration.22 Among victims of motor vehicle accidents, motor cycles were responsible for more than half of the reported cases, followed by cars. In developing countries with lower socioeconomic status, the mode of transportation is mostly on light motor vehicles but people tend not to use safety apparatus such as a motor cycling helmet; particularly when they are involved in more dangerous errands such as transporting furniture or fast delivery of products. Altogether, this particular category remains at a greater risk of incurring ocular trauma and subsequent eye lid laceration.
Among all eye trauma with lid lacerations in the current study, only 5 cases were suspicious of infectious cellulites as they showed signs of infection around the sites of injury; this low rate of infection has been previously noted in traumatic occulopathies, where post traumatic endophtalmitis were rarely seen among the victims of ocular trauma.24,25 In addition, tissue involvement of skin to muscle was observed in five cases, while only one patient was found to have a ruptured septum; moreover, five cases showed orbital fracture compared with only one case noted to have concomitant fracture of nasal bones.
Of the four cases with tissue loss, none needed repair with tissues grafting. Moreover, no canalicular injury was reported. In contrast, only six patients in our study had globe injuries of which three were microscopic and the remaining three exhibited evident conjunctival laceration. Visual acuity of both eyes was significantly different between cases with lid laceration and concomitant open globe injuries, compared with non-globe injury cases; this is consistent with other studies in which open globe injuries were considered to be the most important prognostic factor for vision and visual outcomes.26-31 However, other complications such as infections or fractures were not significantly associated with the severity of the trauma.
It is worth mentioning that we pay attention to the alertness of all the traumatic cases which showed a Glasgow Coma Scale (GCS) of 15 at the time of admission to the emergency department (ED). This constitutes a study limitation where the study population was selected among patients with ocular trauma of mild to moderate severity. Other limitations include the small sample size, the fact that it was a single-center study rather than it being population-based, as well as the cross-sectional design of the study. However, the main objective of this study was achieved and that was the determination of high risk individuals and high risk conditions which raise concern for eye lid laceration along with/without serious ocular trauma. From this, it is possible to propose preventive recommendations and safety precautions for work places to lower the incidence of avoidable injuries in our society. Certainly, further studies are needed to enrich the current findings and resolve the pitfalls in the current investigation.
Conclusion
The results of this study provide a series of high risk conditions which would be better avoided and lists a number of factors which could be modified. By distinguishing the individuals already at greater risk of developing eye lid laceration, recommendations could be established to prevent such incidents from occurring and avoid excessive costs and other burdens imposed on our society as a result. This is particularly true in developing countries like Iran, where drawing attention towards cost-effective expenditure of resources is essential, and this alone may prove to be of great benefit to the nation and its people.
Acknowledgements
We hereby thank our dear colleagues, Ms. Shahbanoo Partovi, Ms. Soheila Partovi, and Mr. Ayatollah Akbari from Farabi Eye Hospital who were friendly and supported us in performing this research study.
References
1. Bert F, Ouahes O, Lambert-Zechovsky N. Brain abscess due to Bacillus macerans following a penetrating periorbital injury. J Clin Microbiol 1995 Jul;33(7):1950-1953.
2. Cillino S, Casuccio A, Di Pace F, Pillitteri F, Cillino G. A five-year retrospective study of the epidemiological characteristics and visual outcomes of patients hospitalized for ocular trauma in a Mediterranean area. BMC Ophthalmol 2008;8:6.
3. Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ 2001;79(3):214-221.
4. Tielsch J. Frequency and consequences of ocular trauma: a population perspective. Ophthalmol Clinics North Am. 1995; (8):559-67.
5. Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol 1998 Sep;5(3):143-169.
6. Karcioglu ZA, Nasr AM. Diagnosis and management of orbital inflammation and infections secondary to foreign bodies: a clinical review. Orbit 1998 Dec;17(4):247-269.
7. Srinivasan S, Macleod S. Fish hook injury to the eyelid - an unusual case. Indian J Ophthalmol 2001 Jun;49(2):115-116.
8. Inchingolo F, Tatullo M, Abenavoli FM, Inchingolo AD, Inchingolo AM, Dipalma G. Fish-hook injuries: a risk for fishermen. Head Face Med 2010;6:28.
9. Kamath G. Fish hook injury of the eyelid: an unusual case. Br J Ophthalmol 2000 Apr;84(4):441-442.
10. Levy J, Lifshitz T. Eyelid fish-hook injury. Int Ophthalmol 2001;24(5):297-298.
11. Wong TY, Klein BE, Klein R. The prevalence and 5-year incidence of ocular trauma. The Beaver Dam Eye Study. Ophthalmology 2000 Dec;107(12):2196-2202.
12. Glynn RJ, Seddon JM, Berlin BM. The incidence of eye injuries in New England adults. Arch Ophthalmol 1988 Jun;106(6):785-789.
13. Dandona L, Dandona R, Srinivas M, John RK, McCarty CA, Rao GN. Ocular trauma in an urban population in southern India: the Andhra Pradesh Eye Disease Study. Clin Experiment Ophthalmol 2000 Oct;28(5):350-356.
14. McCarty CA, Fu CL, Taylor HR. Epidemiology of ocular trauma in Australia. Ophthalmology 1999 Sep;106(9):1847-1852.
15. Katz J, Tielsch JM. Lifetime prevalence of ocular injuries from the Baltimore Eye Survey. Arch Ophthalmol 1993 Nov;111(11):1564-1568.
16. Fong LP. Eye injuries in Victoria, Australia. Med J Aust 1995 Jan;162(2):64-68.
17. Casson RJ, Walker JC, Newland HS. Four-year review of open eye injuries at the Royal Adelaide Hospital. Clin Experiment Ophthalmol 2002 Feb;30(1):15-18.
18. Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton MP. Gender differences in etiology and outcome of open globe injuries. J Trauma 2005 Jul;59(1):175-178.
19. Tielsch JM, Parver L, Shankar B. Time trends in the incidence of hospitalized ocular trauma. Arch Ophthalmol 1989 Apr;107(4):519-523.
20. Karlson TA, Klein BE. The incidence of acute hospital-treated eye injuries. Arch Ophthalmol 1986 Oct;104(10):1473-1476.
21. Klopfer J, Tielsch JM, Vitale S, See LC, Canner JK. Ocular trauma in the United States. Eye injuries resulting in hospitalization, 1984 through 1987. Arch Ophthalmol 1992 Jun;110(6):838-842.
22. Schein OD, Hibberd PL, Shingleton BJ, Kunzweiler T, Frambach DA, Seddon JM, et al. The spectrum and burden of ocular injury. Ophthalmology 1988 Mar;95(3):300-305.
23. Nirmalan PK, Katz J, Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, et al; Aravind Comprehensive Eye Survey. Ocular trauma in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology 2004 Sep;111(9):1778-1781.
24. Thompson WS, Rubsamen PE, Flynn HW Jr, Schiffman J, Cousins SW. Endophthalmitis after penetrating trauma. Risk factors and visual acuity outcomes. Ophthalmology 1995 Nov;102(11):1696-1701.
25. Schmidseder E, Miño de Kaspar H, Klauss V, Kampik A. [Post-traumatic endophthalmitis after penetrating eye injuries. Risk factors, microbiological diagnosis and functional outcome]. Ophthalmologe 1998 Mar;95(3):153-157.
26. Sternberg P Jr, de Juan E Jr, Michels RG, Auer C. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am J Ophthalmol 1984 Oct;98(4):467-472.
27. Esmaeli B, Elner SG, Schork MA, Elner VM. Visual outcome and ocular survival after penetrating trauma. A clinicopathologic study. Ophthalmology 1995 Mar;102(3):393-400.
28. Hutton WL, Fuller DG. Factors influencing final visual results in severely injured eyes. Am J Ophthalmol 1984 Jun;97(6):715-722.
29. Kearns P. Traumatic hyphaema: a retrospective study of 314 cases. Br J Ophthalmol 1991 Mar;75(3):137-141.
30. Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology 1988 Jul;95(7):911-916.
31. Verma N, Verma A, Jacob G, Demok S. Profile of ocular trauma in Papua New Guinea. Aust N Z J Ophthalmol 1997 May;25(2):151-155.
|
|