|
Abstract
Objective: The present study was conducted to evaluate the efficacy of Abana® (a poly-ingredient formulation with natural constituents) on in vitro platelet aggregation and occlusion-induced deep venous thrombosis in rats.
Methods: Anti-platelet property of Abana® was evaluated using ADP (Adenosin 5′-diphosphate) and adrenaline-induced platelet aggregation models, and anti-thrombotic activity was evaluated against occlusion-induced deep venous thrombosis model in wistar rats.
Results: Under the in vitro conditions, Abana® (250, 500 and 1000 µg/ml) alleviated ADP and adrenaline-induced platelet aggregation in a dose-dependent manner. Abana® (1000 µg/ml) inhibited ADP and adrenaline-induced platelet aggregation by as much as 50.69% and 64.83% respectively. Furthermore, 6 days pre-treatment with Abana® (250 and 500 mg/kg, p.o.) in an in vivo study showed significant and dose-dependent protection against occlusion-induced deep venous thrombosis in rats.
Conclusion: These findings suggest that Abana®, a polyherbal formulation possesses anti-platelet and anti-thrombotic activities in the experimental models of in vitro platelet aggregation and in vivo deep venous thrombosis in rats.
Keywords: Abana®; Anti-platelet; Anti-thrombotic; Adrenaline-induced platelet aggregation; Deep venous thrombosis.
Introduction
It is well known that platelets play an important role in the physiology of primary hemostasis and in pathophysiological processes such as thrombosis.1,2 Aberrant intravascular thrombosis is the main cause of wide variety of cardiovascular diseases.3,4 Upon activation of receptors on the platelet plasma membrane, bioactive substances such as calcium, growth factor and aggregation-related secretory biomolecules present in the granules are released in an energy-dependent process that requires ionized calcium.5,6 The signaling of these endogenous and exogenous molecules is the main factor of platelet aggregation.4 In vitro platelet aggregation can be induced by ligands such as ADP, adrenaline, collagen and thrombin.4-6 The activation of downstream signaling by these ligands leads to the change of shape and granule secretion, and thus, the integrin αIIbβ3 will be activated which results in complete platelet aggregation.5 Furthermore, in vivo platelet aggregation can be a cause of serious cardiovascular diseases, including atherosclerosis, ischemia, thrombosis, infarction and stroke.4
Deep-vein thrombosis (DVT) is a major cause of death and morbidity in hospitalized patients. Venous thromboembolism (VTE) is a major cause of morbidity and mortality, which includes deep vein thrombosis (DVT) and pulmonary embolism (PE). In the United States, it is estimated that up to 1 million people are afflicted with VTE every year. Of these, 300,000 people develop PE, which turns fatal among one-third of them.7,8 VTE is the third most common vascular disease after heart attack and stroke. Annually, PE causes more deaths than breast cancer, AIDS and traffic accidents combined.9 In addition, PE and DVT also lead to postphlebitic syndrome in upto 50% of patients.10 Thus, VTE is not only a major cause of mortality, but it also leads to significant morbidity.
Most DVT arise in the deep veins of legs, which is commonly found after surgery, particularly after orthopedic surgery. Thus, without vigorous perioperative thromboprophylaxis, there is venographic evidence of DVT in 50% to 70% of patients undergoing hip or knee arthroplasty or surgery for hip fracture. Furthermore, even with the best forms of prophylaxis, breakthrough DVT occurs in 25% to 35% of patients undergoing knee replacement surgery and in 10% to 15% of those having hip replacement surgery.11
Abana is a herbal preparation approved by the Government of India's Drug Regulatory Authority (Department of Ayush, Ministry of Health and Family Welfare). Its composition constitutes a mixture of extracts of Terminalia arjuna (bark) 30 mg, Withania somnifera (root) 20 mg, Nepeta hindostana (whole plant) 20 mg, Tinospora cordifolia (stem) 10 mg, Emblica officinalis (fruit)10 mg, Terminalia chebula (fruit rind) 10 mg, Eclipta alba (whole plant) 10 mg, Dashamoola (root) 20 mg, Glycyrrhiza glabra (root) 10 mg, Asparagus racemosus (root) 10 mg, Boerhaavia diffusa (root) 10 mg, and powders of Balsamodendron mukul (oleo-gum-resin) 30 mg, as well as Centella asiatica (whole plant) 10 mg, Convolvulus pluricaulis (whole plant) 10 mg, Ocimum sanctum (whole plant) 10 mg, Nardostachys jatamansi (rhizome) 10 mg, Piper longum (fruit) 10 mg, Carum copticum (seed) 10 mg, Zingiber officinale (rhizome), Cyperus rotundus (tubers) 5 mg, Acorus calamus (Rhizome) 5 mg, Embelia ribes (fruit) 5 mg, Syzygium aromaticum (flower bud) 5 mg, Celastrus paniculatus (fruit) 5 mg, Santalum album (wood) 5 mg, Elettaria cardamomum (fruit) 5 mg, Foeniculum vulgare (seed) 5 mg, Rosa centifolia (flower) 5 mg, Cinnamomum cassia (bark) 5mg, and Crocus sativus (Style and Stigma) 2 mg.12
Abana has been available in the market for several decades. It has been tested for its quality and consistency in each and every step of manufacturing as per the accepted principles of GMP (good manufacturing practice) and GLP (good laboratory practice). Abana has been standardized with respect to various parameters which comply to the stringent quality check specification of the finished product. The product is standardized by physical and chemical parameters such as determination of total tannin and flavonoid contents, which represent the major chemical markers for standardization. Every batch of Abana is compared with the reference control in terms of various quality parameters and also unique TLC (Thin layer chromatography) finger printing.
Abana® has been reported to be beneficial in several cases of hypertension and angina pectoris. In India, it has been clinically used from several decades to treat hyperlipidemia, hypertension,13-15 and other cardiovascular diseases.16-18 The mechanism behind the beneficial effect of Abana® in cardiovascular diseases has not been scientifically proven, and henceforth this study is useful in exploring those means. With this regard, present study was undertaken to evaluate anti-platelet and anti-thrombotic activities of Abana® in in vitro and in vivo conditions, respectively.
Methods
Adrenaline (Sigma Aldrich, Bangalore) and adenosine 5′- diphosphate (Himedia) were used in the study. Other solvents and chemicals used were highly pure and of analytical grade and were purchased from reputed local firms. Inbred male Wistar rats (250-300 g) were used for the study. The animals were maintained in polypropylene cages at a temperature of 25ºC ± 1°C and relative humidity of 45% to 55% in a clean environment under 12:12 hrs light-dark cycle. The animals had free access to food pellets (Pranav Agro Industry, Bangalore, India) and purified water.
All the experimental protocols were approved by Institutional Animal Ethics Committee (IAEC) of The Himalaya Drug Company and were conducted according to the guidelines of Committee for the Purpose of Control and Supervision of Experimentation on Animals (CPCSEA), India.
The anti-platelet activity was determined by preparations of platelet-rich and platelet-poor plasma. Blood samples were collected from healthy male wistar rats in 0.35% sodium citrate solution, platelet count was measured using Abacus cell counter. The citrated blood samples were centrifuged at 1000 rpm for 15 mins at room temperature; the platelet-rich plasma (PRP) was obtained by decanting the supernantant layer called platelet-poor plasma (PPP).19,20
Processing of platelet-rich plasma was done after separating PRP from citrated blood, the platelet counts were measured and PRP was diluted with Tyrode solution containing 0.35% BSA to get a platelet count of 300-400 × 103 cells/μl or 300-400 × 106 cells/ml.19,20 To determine the in vitro Adrenaline-induced platelet aggregation, a standard curve for adrenaline-induced platelet aggregation was plotted by taking different concentrations of adrenaline. In short, 10 μM of adrenaline was prepared in 0.5% DMSO (Dimethyl sulphoxide) and DM water, further dilutions (5 and 2.5 μM) were prepared by using DM water. Various concentrations of adrenaline were added to PRP and platelet aggregation was monitored by recording the change in absorbance in kinetic mode for 10 mins at 600 nm.20
In addition, to determine the ADP-induced platelet aggregation in in vitro, a standard curve for ADP-induced platelet aggregation was plotted by taking different concentrations of ADP. In short, 100 μM of APD was prepared in DM water, and from this 100μM stock solution, 50, 25, 12.5 and 6.125 μM concentration were prepared using DM water. Various concentrations of ADP were added to PRP and platelet aggregation was monitored by recording the change in absorbance in kinetic mode for 10 mins at 600 nm.19
In vitro anti-platelet activity was carried out as per the available literature.20,21 In summary, 160 μl of PRP was dispensed into a 96-well micro plate and basal absorbance was recorded at 600 nm. Then 20 μl of vehicle (DM water) or various concentrations of Abana® and Aspirin (100 µM) were added separately to the respective wells and mixed thoroughly for 1-2 mins by manual shaking. Then 20 μl of adrenaline (10 μM) /ADP (100 µM) was added and the aggregation process was monitored for next 10 mins by recording the absorbance in kinetic mode for 10 mins at 600 nm along with respective blank readings. A graph of decrease in absorbance vs. time (min) was plotted and percentage inhibition of platelet aggregation (% anti-aggregation) was calculated using following equation; where, Co = Initial absorbance PRP of respective sample (before adding the vehicle, drugs, or adrenaline) and Cf = Final absorbance (10th min) after adding the adrenaline.19,20
For the determination of Occlusion-induced venous thrombosis in rats; Wistar rats weighing 250-300 g were divided into 4 groups (n=8) on the basis of body weight, all the animals in the G-1 to G-4 underwent IVC ligation. G-1 served as positive control (only IVC ligation no treatment), G-2 and G-3 were pre-treated with Abana® 250 and 500 mg/kg, p.o., respectively; G-4 animals were pre-treated with aspirin (1 mg/kg/day, p.o.), for 6 days before the IVC ligation.21 On 7th day, all the animals from G-1 to G-4 underwent surgical procedure for IVC ligation; all the animals were anesthetized using urethane (1.5 g/kg,i.p) and the IVC was exposed through a midline laparotomy by dissecting at the level of renal veins and ligated below the renal veins until the iliac trunk (1-1.2 cm length [Fig.1]). While performing the IVC ligation, if the dissection was traumatic or the IVC was ruptured during surgery, such animals were not considered for further study. After the IVC ligation, the animals were housed individually in polypropylene cages for 1 hr and immediately after 1 hr, the ligated IVC was isolated by cutting on both the ends. In case of sham control, the freshly ligated IVC was immediately isolated. The following parameters were recorded in all the animals:
1. Total length of the ligated IVC
2. Length of the thrombus formed inside the ligated IVC
3. Weight of the thrombus formed inside the ligated IVC
Using above mentioned directly measurable quantitative parameters, the ratio of the length of the thrombus (mm) to the length of IVC ligation (mm), and the weight of the thrombus (mg) to the length of the IVC ligation (mm) were calculated or derived as follows:
The quantitative parameters obtained in drug pre-treated groups (G-2, G-3 and G-4) were compared with positive controls (G-1).21
For statistical analysis, the values were expressed as mean ± SEM. The results were analyzed statistically using one way ANOVA followed by Tukey’s multiple comparison test to determine the level of significance. The minimum level of significance was fixed at p<0.05.
Results
The anti-platelet activity in terms of adrenaline-induced platelet aggregation, indicated a dose-dependent increase in platelet aggregation in PRP separated from rat blood (Fig.2). On the basis of the dose-response curve, 10 μM concentration of adrenaline was selected for screening the anti-platelet potential. Abana® at 250, 500 and 1000 µg/ml concentrations alleviated the adrenaline-induced platelet aggregation in a significant and dose-dependent manner in in vitro conditions with a percent inhibition of 22.0%, 40.6% and 64.8%, respectively. Aspirin (100 µM) was used as a reference standard, which offered 88.53% inhibition. (Fig. 3)
In terms of ADP-induced platelet aggregation, ADP showed a dose-dependent increase in platelet aggregation in PRP separated from rat blood (Fig. 4). Abana® dose-dependently alleviated the ADP induced-platelet aggregation in in vitro conditions. Abana® at 250, 500 and 1000 µg/ml and Aspirin at 100 µM concentrations offered 22.4%, 41.3%, 50.7% and 85.3% inhibition, respectively, against ADP-induced platelet aggregation. (Fig.5)
On the other hand, occlusion-induced deep venous thrombosis is the most popular method for screening anti-thrombotic potential. In the present study, inferior venacaval ligation (IVC) caused prominent thrombus formation in the occluded region of the vena cava in wistar rats; positive control animals showed a significant increase in the length and weight of the thrombus, which was associated with a statistically significant increase in the derived parameters, that is, the ratio of thrombus weight to IVC length and ratio of thrombus length to IVC length. Pre-treatment with Abana® (250 and 500 mg/kg, p.o.) and aspirin (1 mg/kg, p.o.) for 6 days exhibited a significant inhibition against occlusion-induced deep venous thrombosis in rats. (Table 1)
Table 1: Effect of Abana® on Occlusion induced venous thrombosis in rats.
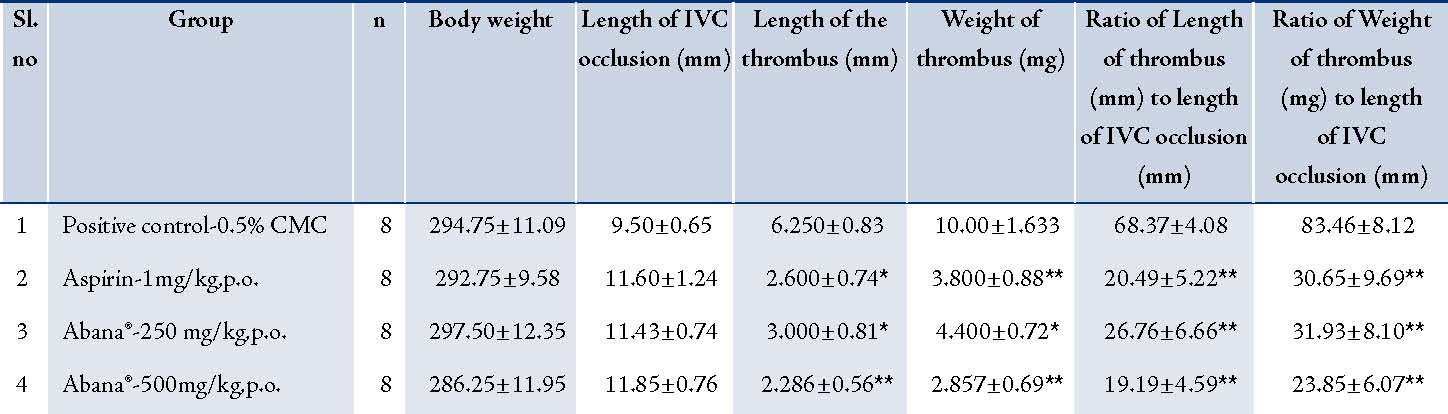
Values are expressed as mean±SEM, and compared with positive control group by one way ANOVA followed by Tukey’s multiple comparison. *p<0.05 and **p<0.01compared to positive control group.
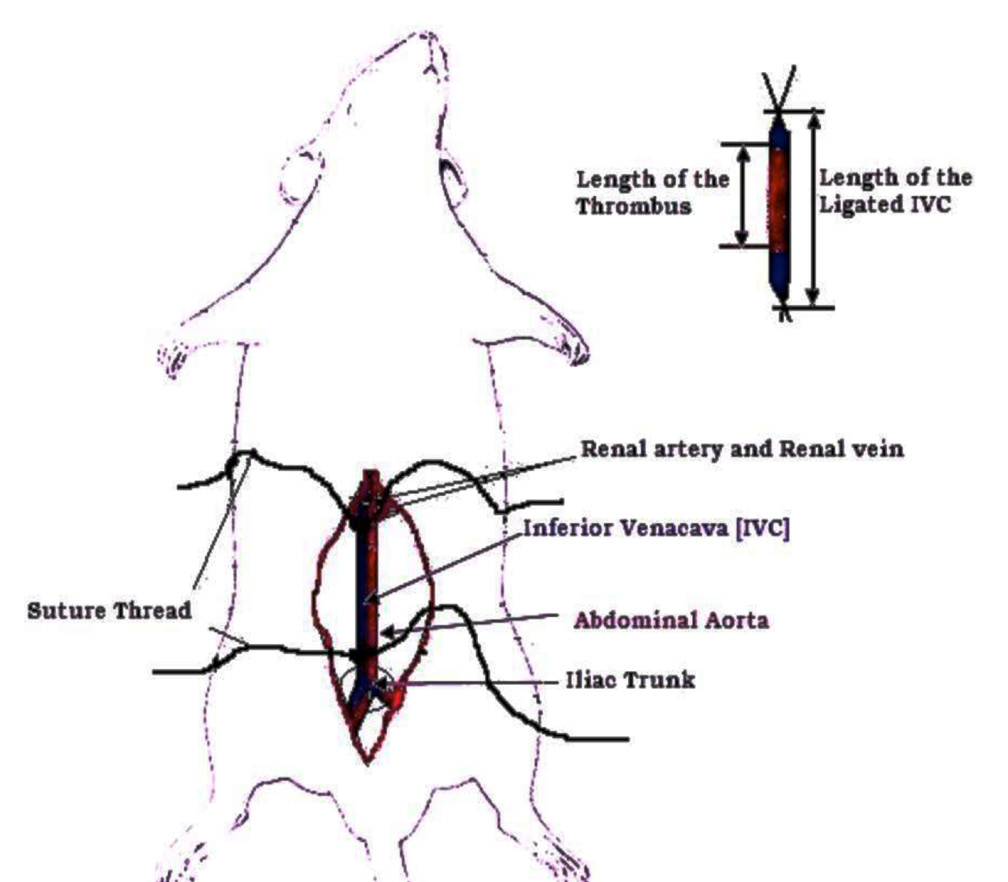
Figure 1: Diagrammatic representation of IVC ligation in rats.
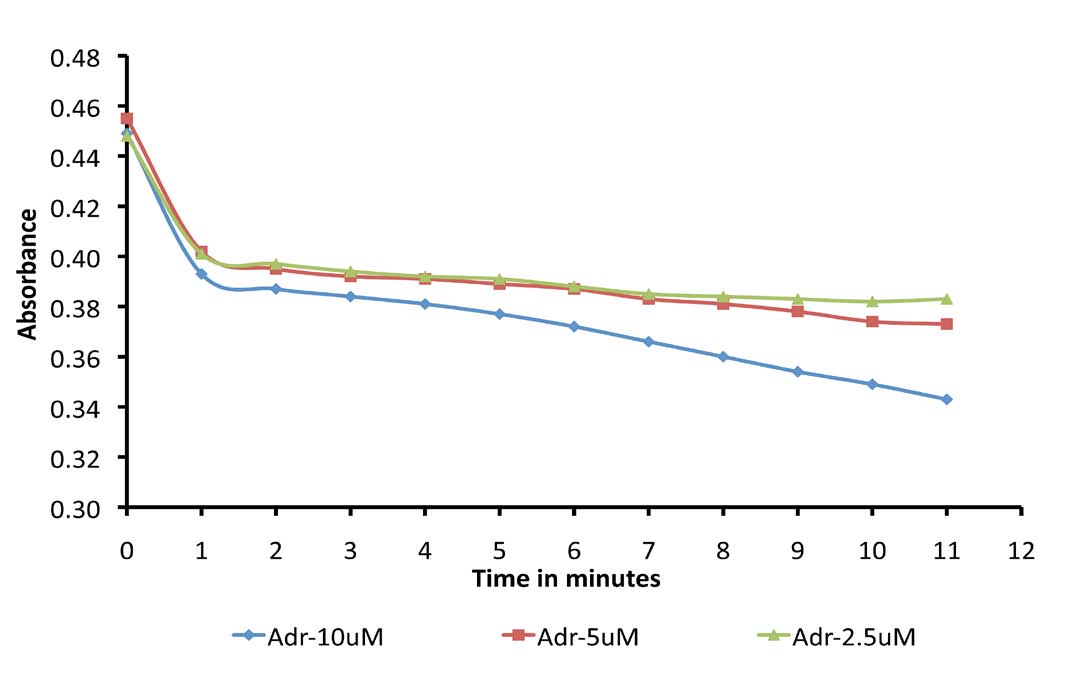
Figure 2: Standard curve for adrenaline induced platelet aggregation.
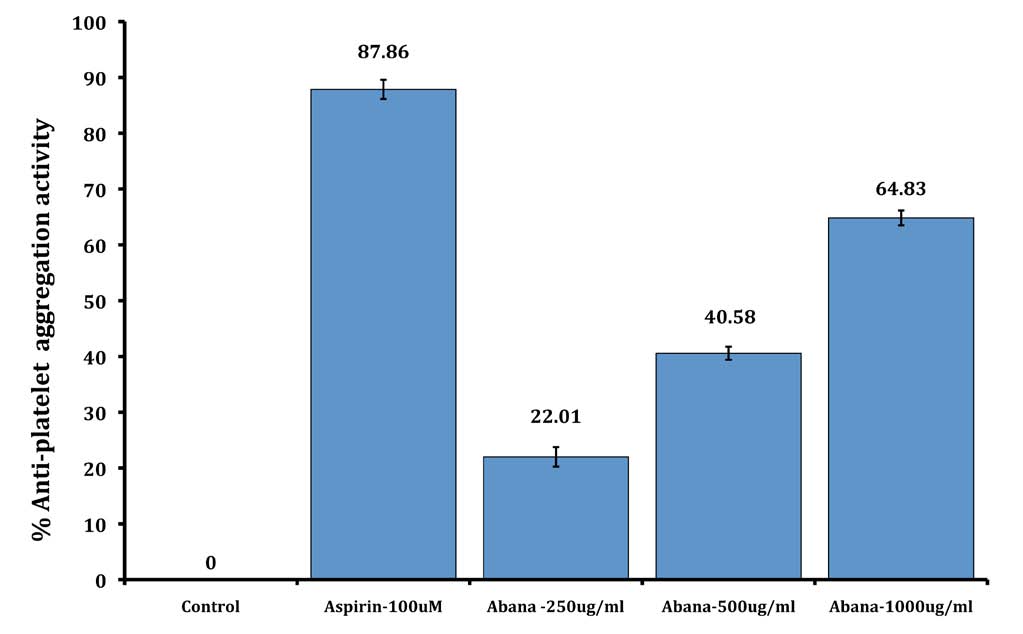
Figure 3: Effect of Abana® on adrenaline induced platelet aggregation.
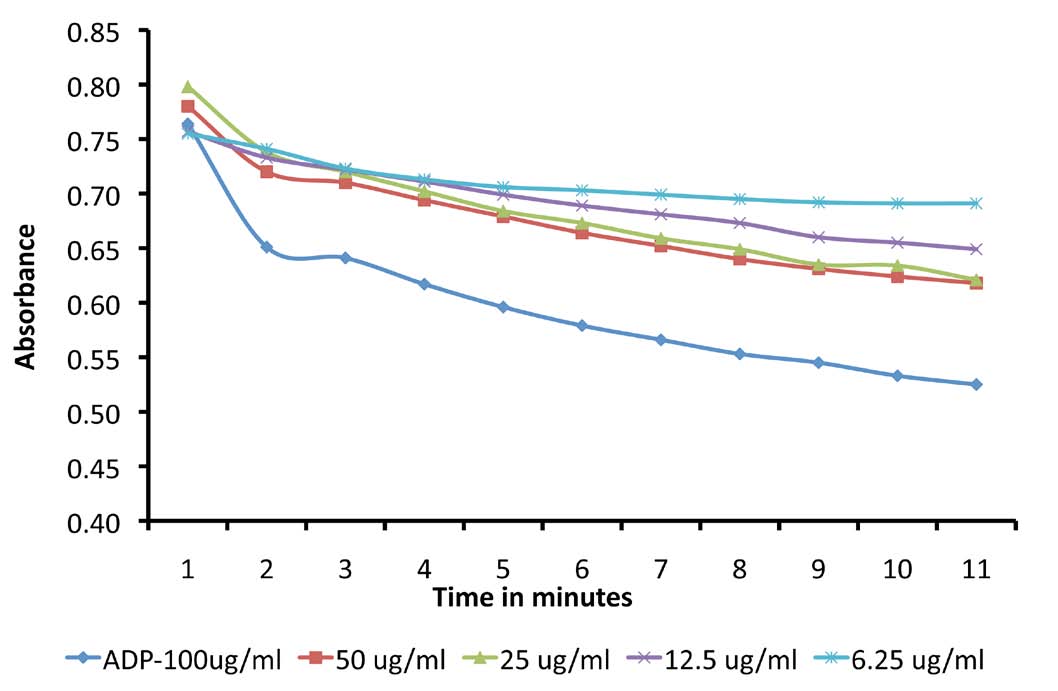
Figure 4: Standard curve for ADP induced platelet aggregation.
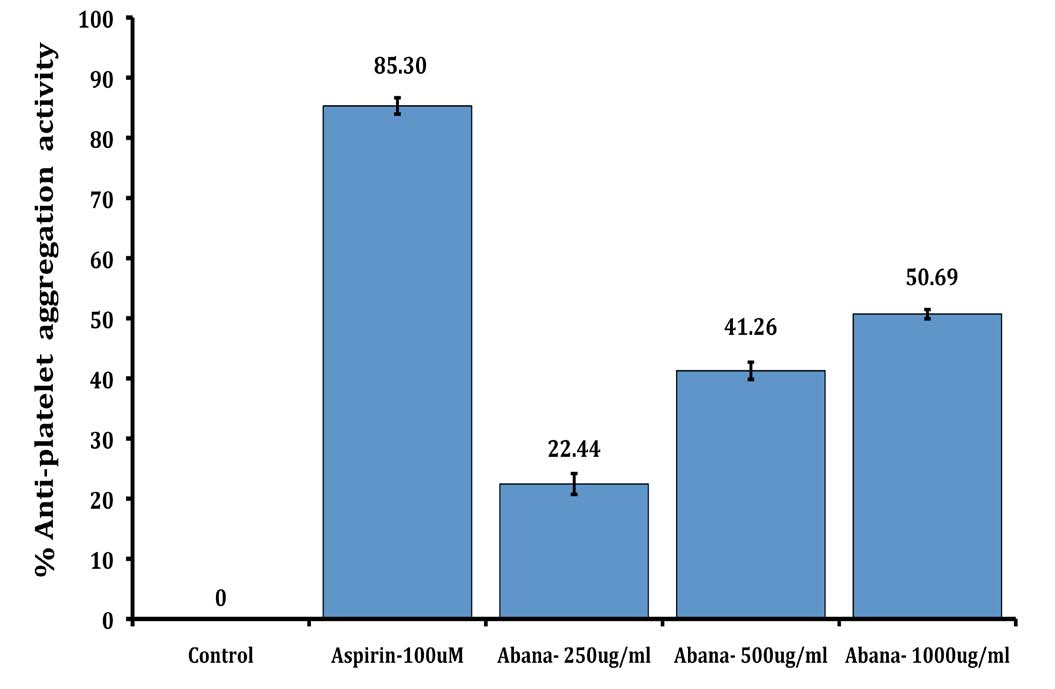
Figure 5: Effect of Abana® on ADP induced platelet aggregation.
Discussion
In the present study, anti-platelet activity of Abana® was evaluated against ADP and adrenaline-induced platelet aggregation models in vitro. ADP can mainly bind to purinergic G-protein-coupled receptors (P2Y1) and can activate phospholipase C (PLc).22,23 Upon activation, PLc hydrolyses phosphatidylinositol 4,5-bisphosphate (PIP3) to inositol-1,4,5-triphosphate (IP3), and diacylglycerol (DAG). IP3 contributes to the release of calcium from intracellular organelles such as endoplasmic reticulum and DAG that activates protein kinase C (PKc).22,23 The cytosolic calcium (third messenger) is a highly versatile regulator acting through calmodulin (CAM), PKc, and other effectors mediate contractions and release of various platelet activation factors from the granules of the platelets which further potentiate the platelet activation process and finally leads to platelet aggregation.22,23
Incubation of adrenaline with PRP in in vitro exhibits a characteristic biphasic aggregation curve, the first phase denoting aggregation mediated through α-adrenoceptors.24 When adrenaline occupies these receptors present on the platelet membrane, adenylate cyclase activity is inhibited, cAMP production is consequently decreased, and platelets tend to aggregate.25 The second aggregation phase is mediated entirely through prostaglandin endoperoxides (PGG and PGH) and thromboxane A2.25,26
In the present study, Abana® at 250, 500 and 1000 µg/ml concentrations showed significant and dose-dependent inhibition against ADP and adrenaline-induced platelet aggregation in in vitro. Furthermore, the possible mechanism behind the anti-platelet activity of the Abana® is considered to be associated with the inhibition of one of the common mediator/pathways involved in ADP and adrenaline-induced platelet aggregation and/or by stabilizing the platelet membrane from a platelet activation process due to externally added ADP and adrenaline. Also in the present study, aspirin (100 µM) was used as a reference standard, it is a well-known non-steroidal anti-inflammatory drug (NSAID) proved to be very beneficial in the prophylaxis of atherosclerosis and arteriosclerosis conditions. Aspirin (100 µM) showed 85.3% and 87.8% inhibition against ADP and adrenaline-induced platelet aggregation, respectively.
On the other hand, IVC occlusion/statis-induced venous thrombosis model in rats is the most common and effective models for screening anti-thrombotic activity of the drugs. Previous studies have proved that statis or IVC occlusion results in excessive secretion of potent platelet aggregating factors, namely platelet factor-4 and β-thromboglobulin from α-granules of the activated platelets; in addition, the elevated levels of serum inflammatory cytokines such as TNF-α and IL-1β, observed as an indication of vein wall inflammation process, is associated with increased myeloperoxidase (MPO) activity. This cascade of events finally results in the formation of venous thrombosis in vivo.27 In the current study, pre-treatment with Abana® (250 and 500 mg/kg, p.o.) for 6 days showed a significant and dose-dependent inhibition against IVC occlusion-induced platelet aggregation and the probable mechanism was believed to be associated with the inhibition of platelet aggregation due to released platelet-activating factors during IVC occlusion.
Conclusion
Abana®-a poly-ingredient formulation possesses very good anti-platelet and anti-thrombotic activity in in vitro and in vivo models, respectively; and the probable mechanism behind its anti-platelet and anti-thrombotic activity is considered to be associated with the inhibition of platelet aggregation caused by various platelet-activating factors.
Acknowledgments
The authors are thankful to M/S The Himalaya Drug Company, Makali, Bangalore for providing all the necessary facilities to carry out the research work. The authors reported no conflict of interest.
References
1. Bernhard N, Markus M, Irina P, David VS, Sue M, David C, et al. Loss of talin1 in platelets abrogates integrin activation, platelet aggregation, and thrombus formation in vitro and in vivo. J Experiment medicine 2007; 204(13):3113-3118.
2. Stouffer GA, Smyth SS. Effects of thrombin on interactions between beta3-integrins and extracellular matrix in platelets and vascular cells. Arterioscler Thromb Vasc Biol 2003 Nov;23(11):1971-1978.
3. Grenache DG, Coleman T, Semenkovich CF, Santoro SA, Zutter MM. Alpha2beta1 integrin and development of atherosclerosis in a mouse model: assessment of risk. Arterioscler Thromb Vasc Biol 2003 Nov;23(11):2104-2109.
4. Huo Y, Ley KF. Role of platelets in the development of atherosclerosis. Trends Cardiovasc Med 2004 Jan;14(1):18-22.
5. Leclerc JR. Platelet glycoprotein IIb/IIIa antagonists: lessons learned from clinical trials and future directions. Crit Care Med 2002 May;30(5)(Suppl):S332-S340.
6. Nesbitt WS, Westein E, Tovar-Lopez FJ, Tolouei E, Mitchell A, Fu J, et al. A shear gradient-dependent platelet aggregation mechanism drives thrombus formation. Nat Med 2009 Jun;15(6):665-673.
7. Schulman S, Beyth RJ, Kearon C, Levine MN; American College of Chest Physicians. Hemorrhagic complications of anticoagulant and thrombolytic treatment: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008 Jun;133(6)(Suppl):257S-298S.
8. Lilienfeld DE. Decreasing mortality from pulmonary embolism in the United States, 1979-1996. Int J Epidemiol 2000 Jun;29(3):465-469.
9. Coombes R. Venous thromboembolism caused 25,000 deaths a year, say MPs. BMJ 2005 Mar;330(7491):559.
10. Kahn SR, Ginsberg JS. Relationship between deep venous thrombosis and the postthrombotic syndrome. Arch Intern Med 2004 Jan;164(1):17-26.
11. Agarwal BV. Trial of AbanaÆ in ischaemia heart disease and hypertension. Probe 1986;4:314-315.
12. Vidyashankar S, Godavarthi A, Varma RS, Nandakumar KS. Water-soluble compounds in the herbal preparation Abana inhibit lipid biosynthesis and enhance cholesterol efflux in HepG2 cells. Can J Physiol Pharmacol 2010 Apr;88(4):456-464.
13. Dadkar VN, Tahiliani RR, Jaguste VS, Damle VB, Dhar HL. Double blind comparative trial of Abana and methyldopa for monotherapy of hypertension in Indian patients. Jpn Heart J 1990 Mar;31(2):193-199.
14. Tiwari AK, Gode JD. A comparative study of AbanaÆ and cholesramine on serum lipids and lipoproteins in hypercholesterolemic rabbits. Arogya J Health Sci 1990;16:88-95.
15. Dubey GP, Agrawal A, Srivastava VK. Regulation of cardiovascular functions with AbanaÆ. Probe 1985;1:27-33.
16. Basu DP, Joshi RL. Abana in cardiac neurosis and similar conditions. Probe 1986;2:131-134.
17. Rao R. AbanaÆ in cardiac disease and cardiac neurosis. Probe 1988;4:274-279.
18. Yajnik VH, Acharya HK. Cardiovascular response to mental and physical stress: modification by AbanaÆ. Probe 1992;4:299-303.
19. Won JO, Mehari E, Ji-Young P, Yi-Seong K, Suk K, Gon-Sup K, et al. The inhibitory effect of Opuntia humifusa Raf. Ethyl acetate extract on platelet aggregation. J Med Plants Resear 2011;5(8):1418-1424.
20. Chien MW, Shu CW, Wan JC, Hsien CL, Kun TC. Antiplatelet Effect and Selective Binding to Cyclooxygenase (COX) by Molecular Docking Analysis of Flavonoids and Lignans. Int J Mol Sci 2007;8:830-841 .
21. Madiha AE, Tarek AE, Samia MA. Effect of selective and non-selective cyclooxygenase inhibitors on survival, platelet function and vein wall inflammation in rat model of deep vein thrombosis. Bull Alex Fac Med 2006;42:239-240.
22. Woulfe DS. Platelet G protein-coupled receptors in hemostasis and thrombosis. J Thromb Haemost 2005 Oct;3(10):2193-2200.
23. Chang CC, Lu WJ, Chiang CW, Jayakumar T, Ong ET, Hsiao G, et al. Potent antiplatelet activity of sesamol in an in vitro and in vivo model: pivotal roles of cyclic AMP and p38 mitogen-activated protein kinase. J Nutr Biochem 2010 Dec;21(12):1214-1221.
24. Dunlop PC, Leis LA, Johnson GJ. Epinephrine correction of impaired platelet thromboxane receptor signaling. Am J Physiol Cell Physiol 2000 Dec;279(6):C1760-C1771.
25. Schwertz H, Weyrich AS. Platelet precursors display bipolar behavior. J Cell Biol 2010 Nov;191(4):699-700.
26. Gresele P, Falcinelli E, Loffredo F, Cimmino G, Corazzi T, Forte L, et al. Platelets release matrix metalloproteinase-2 in the coronary circulation of patients with acute coronary syndromes: possible role in sustained platelet activation. Eur Heart J 2011 Feb;32(3):316-325.
27. Eriksson EE, Karlof E, Lundmark K, Rotzius P, Hedin U, Xie X. Powerful inflammatory properties of large vein endothelium in vivo. Arterioscler Thromb Vasc Biol 2005 Apr;25(4):723-728.
|