|
Abstract
Objective: In Rheumatology, non-steroidal anti-inflammatory drugs (NSAIDs) has been widely prescribed and used. However, despite their clinical benefits in the management of inflammatory and degenerative joint disease, NSAIDs have considerable side effects, mostly affecting the upper gastrointestinal system, which therefore, limit their use. This study was conducted to determine the patients’ knowledge and perception regarding the used of NSAIDS.
Methods: A total of 120 patients who attended the rheumatology clinic Hospital, Raja Permaisuri Bainun, Malaysia, and received NSAIDs more than 3 months were interviewed irrespective of the irrheumatological conditions. Patient’s knowledge and perception on the side effects of NSAIDs were recorded.
Result: Fifty-four percent of the patients obtained information regarding the side effect of NSAIDs either from the rheumatologist, rheumatology staff nurse or other medical staffs (75.4%). The remaining 45.8% were naive of such knowledge. Fifteen percent obtained the information by surfing the internet and 9.2% from printed media. Twenty-four (24.2%) patients, experiencedin digestion and/or stomach discomfort attributed to NSAIDsused. Two patients (1.7%) had hematemesis and malena once.
Conclusion: This study shows that half of the patients who attended the rheumatology clinic were unaware of the side effect of NSAIDs. Available data showed that most of the knowledgeable patients are more conscience and self-educated. This study also reveals the important roles of clinicians, trained staff nurses as well as the pharmacist in providing the guidance and knowledge of any medication taken by patients.
Keywords: NSAIDs; Knowledge; Side effects; Rheumatology.
Introduction
The used of NSAIDs has been well established worldwide with an estimated daily intake of 30 million people.1 Patients have easy access to these drugs either over-the-counter (OTC) formulations as well as in prescription form. NSAIDs are commonly used in both osteoarthritis (OA) and rheumatoid arthritis (RA) to reduce joint pain and to improve joint function.2,3 It is important as part of the disease management.
NSAIDs are still considered relatively safe drugs as reflected by their increased prevalent. Gastrointestinal (GI) and renal effects are the two most commonly affected systems associated with prolonged used of NSAIDs. These effects contribute to limited use of NSAIDs. Successful pharmacotherapy is virtually dependent on patient adherence and a rational choice of drug. Information regarding the pharmacological properties of the drugs including instructions for use and warnings, as well as the indication and justification should be delivered to the patients effortlessly via education. A readable and correct prescription does not guarantee appropriate use by the patient.4,5 Failure to provide such information may lead to poor compliance,6,7 where physician as well as the pharmacist can play an important role in delivering the information in order to improve patient compliance.8
Previous studies had demonstrated that, despite being widely used, the adverse effects of NSAIDs, patients’ knowledge and awareness of potential side-effects of the medicines has been poor.9 This study focuses on the knowledge and perception of patients of NSAIDs at the Rheumatology clinic setting, Hospital Raja Permaisuri Bainun, Malaysia.
Method
This is a descriptive cross sectional study involving patients who attended the Rheumatology clinic, at Hospital Raja Permaisuri Bainun Ipoh, Malaysia. The patients were aged more than 18 years, and were prescribed non-steroidal anti inflammatory drugs (NSAIDs) for more than 3 months, irrespective of their rheumatic disorder. Other demographic data such as gender, ethnicity, education levels, duration of disease and duration of NSAIDs used were recorded. The study was conducted within 4 weeks duration; with a total patient follow-up for a week for 30 patients. The study was conducted by interviewing the patients using a prepared questionnaire. The purpose of the study was explained verbally in Malay or English languages to each patient and the questionnaire was completed after obtaining written consent.
From calculation (Epi-info), assuming frequency of knowledge of Malaysian population is 50 %, with confidence Interval of 95% and lower limit of 40%, sample size was 96 patients. One-hundred-and-twenty samples were collected within 4 weeks of study due to total sampling method and to validate the sample for subgroup analysis. Descriptive statistics, including percentages, means, standard deviation, frequencies and cross-tabulations were determined.
Results
A total of 120 patients were interviewed with a 100% response rate. The study population was predominantly female (68.3%) with a mean (SD) age of 53 ±(12), as well as Malay ethnic group (44.2%) followed by Chinese (32.5%) and Indian (22.5%). Most patients received their formal education at primary (17.5%), secondary (51.7%) and tertiary (27.5%) levels. While the majority of patients suffered from rheumatic diseases of 5 years duration (54.2%). All 120 patients were prescribed NSAIDs ever since follow-up at the rheumatology clinic. (Table 1)
Table 1: Baseline demographics and clinical characteristics.
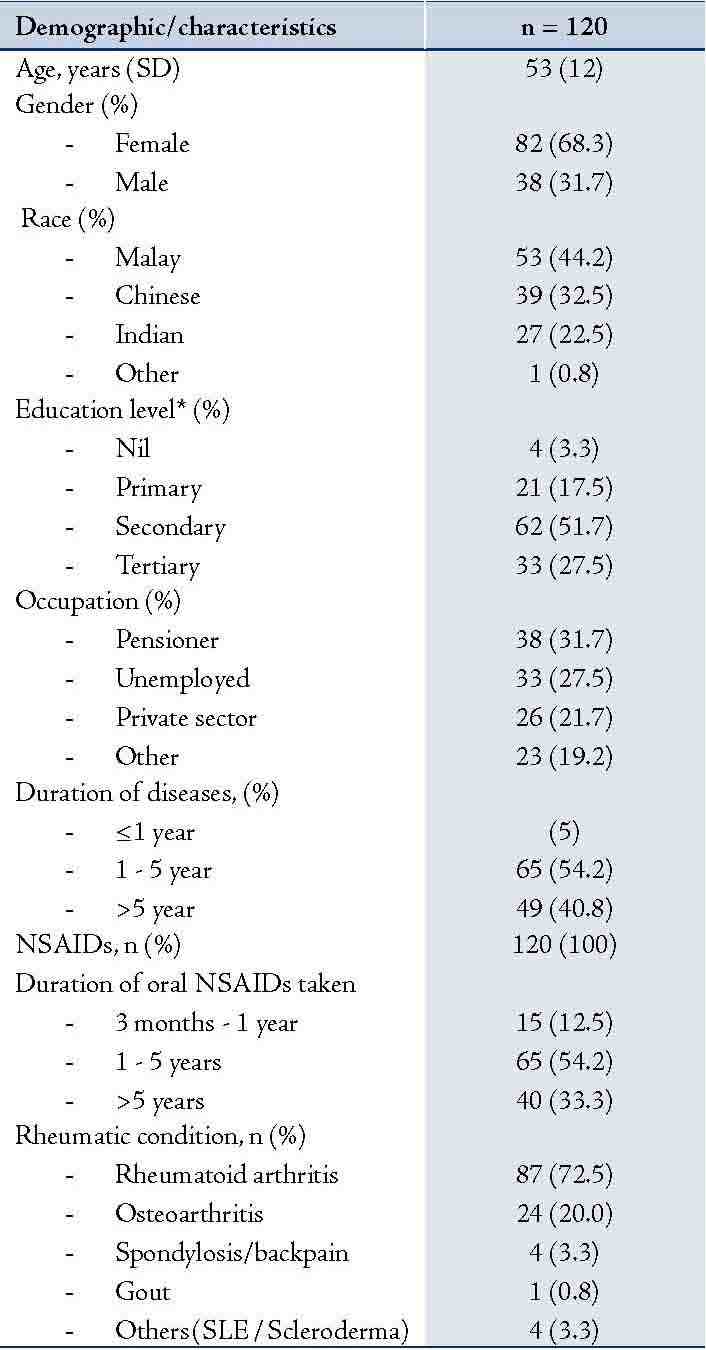
*Primary = primary school, age from 7 year to 12 year; Secondary = secondary school, age from 13 year to 19 year; Tertiary = College or university levels.
Irrespective of the rheumatic disorders, 66 (55.0%) patients were using Meloxicam (Mobic) followed by 40 (33.3%) patients using Celecoxib (Celebrex) and 8 (6.7%) were on diclofenac sodium (voltaren), while 6 (5.0%) patients were taking Etoricoxib (Arcoxia).
Worsening of pain was influenced by the change in treatment for majority of the patients. While most of the patients (77.5%) tried other therapy such as exercise, 10% of them decided to remain with the status quo and others (5.8%) either increased the dosage of the drug or the doctor changed the NSAID. Meanwhile, 27 (22.5%) patients used traditional medicine in combination with NSAIDs. However, out of those, 6 (22.2%) continued with the NSAID while 21 (77.8%) discontined therapy. The main reason for discontinuation being that the drug was ineffective.
A large proportion of the patients were prescribed NSAIDs due to of pain and symptoms of swollen joints. Some of the patients had developed irreversible damage leading to deformities and disability due to active disease, while 87% of the studied patients had been taking NSAIDs for more than 1 year. Moreover, over half (54.2%) of the study participants actually had knowledge or awareness of the side effects attributed to NSAIDs. However, the remaining 45.8% of patients were unaware of the adverse implications of the drugs. The results indicate that females (61%) exhibited greater knowledge and concerns about the side effects compared to their male counterparts (39.5%). As far as ethnicity is concerned, 71.1% of Malays were more knowledgeable about the side effects of NSAIDs, followed by 46.2% Chinese and 33.3% Indian patients. However, this finding was not significant since the distributions of the sample was not equal and the sample frequencies were small. Language barriers, low socio-economic and educational levels were among the main factors affecting these results.
Meloxicam was most commonly used for osteoarthritis (50%) and rheumatoid arthritis (59%), followed by celecoxib and diclofenac sodium. Diclofenac sodium was the drug of choice for gouty arthritis. In addition, only 65 patients were aware of the possible side effects of NSAIDs; the information was mainly obtained from Hospital (75.4%), either from the clinician or nurses, 15.4% (10) and 9.2% (6) obtained the information by surfing the internet and from newspapers, respectively. However, none of the patients reported that they obtained information from television, colleagues or magazines. Patients were advised to seek immediate treatment at hospital (31; 47.7%) or stop taking the medication (30; 6.2%) when they experienced adverse effects of the NSAIDs. Only a small number of patients were advised to continue with the therapy but with precaution (4; 6.2%).
From the total of 120 patients, 29 (24.2%) patients experienced indigestion/stomach pain while on NSAIDs. Two patients developed peptic ulcer bleeding once in their life which warranted admission (Table 3). Only 13 (10.8%) from the total number of patients used gastro protective agents (i.e., antacid, H2-antagonist and proton pump inhibitors). All patients were prescribed NSAIDs and advised to take on pro re nata (PRN) basis. Forty-one (34.2%) patients took all the NSAIDs that they were prescribed. Meanwhile, the remaining patients either consumed a quarter or half to three quarters of the amount of NSAIDs they were prescribed. (Table 4)
Table 2: Distribution of types of NSAIDs used in difference diseases.
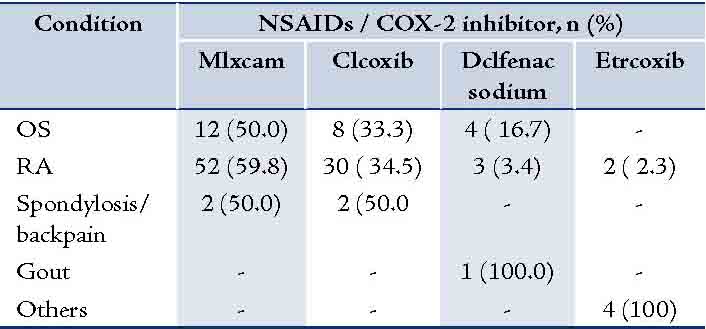
OS: Osteoarthritis; RA: Rheumatiod arthritis; Mlxcam: Meloxicam; Clcoxib: Celecoxib; Etrcoxib: Etoricoxib.
Table 3: Distribution of side effects of NSAIDs.
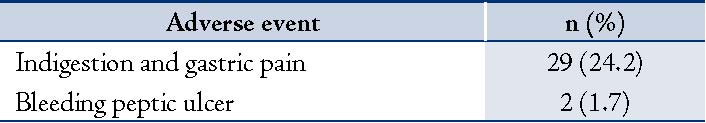
Table 4: Amount of NSAIDs prescribed consumed by patient.
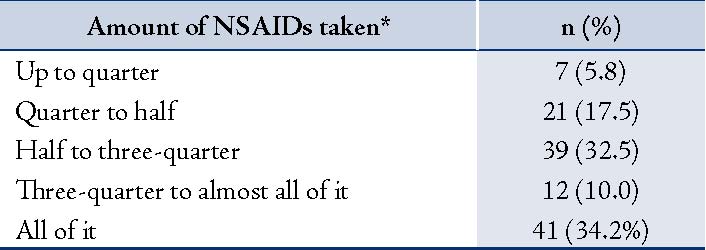
*Estimated amount of NSAIDs prescribed taken by patients following each consultation visit.
Discussion
Although the study sample was relatively small, the study still provides important information pertaining to knowledge of medication prescribed to rheumatic patients, (i.e. not only on NSAIDs, but it also applies to disease modifying anti rheumatic drugs (DMARDs) and other treatment). Evidence suggests that increased information with regards NSAIDs and other forms of pharmacotherapy leads to greater patient satisfaction.10,11 Low socio-economic and educational or literacy status, self consciences were the main factors identified to be affecting the knowledge of medication prescribed. However, there was no significant difference between patients who were aware and those who were unaware of the side effects of NSAIDs in the current study. As a comparison, previous studies have established and demonstrated better results as far as awareness is concerned.12,13 However, medical staff (i.e., doctors and nurses) were found to be the main source of drug information obtained by patients in our study, as well as in other studies. Nevertheless, other sources such as drug information leaflets, internet, colleagues and pharmacist were equally important in providing details of the prescribed medications.12,13,14,15
NSAIDs were prescribed for almost all arthritic patients either in regular or pro re nata basis irrespective of the rheumatological diagnosis. In our survey, rheumatoid arthritis patients receiving NSAIDs outnumbered other rheumatic disorders compared to the study conducted by Wynne and Long where NSAIDs were mostly prescribed for osteoarthritis followed by rheumatoid arthritis and other disorders.13 The difference appears to be attributed to the number of RA patients most commonly seen at our rheumatology clinic, whereas more of OA patients are treated by orthopedic surgeons.
The choice of NSAIDs prescribed is individualized and varies in different practices.14,16 Drug availability, cost, familiarity and tolerability are among many factors which play an important role in the treatment strategy for rheumatic diseases. At our centre, most of the older NSAIDs (indomethacin, diclofenac sodium, ibuprofen, naproxen, meloxicam) and newer COX-2 inhibitors (celecoxib, etoricoxib) are readily available. The duration of NSAIDs usage and the quantity needed to be taken varies from patient to patient. This variation can be explained by the fact that increased awareness of the side effects of NSAIDs among patients, ineffectiveness of the NSAIDs, improvement in the clinical disease activity with DMARDs and the introduction of biologic agents leads to better pain control. Hence, reduce the use of NSAIDs. Pain threshold, though it is a subjective perception, may also affect the usage of NSAIDs and this may be attributed to certain ethnic groups. Over the counter prescription or self-prescriptions (NSAIDs, corticosteroid or alternative medicine with or without containing both) are also important contributing factors. Moreover, patient compliance was poor as reported elsewhere.13
In this study, the number of patients who developed gastrointestinal symptoms due to chronic usage of NSAIDs were relatively high compared to the study conducted by Silvani et al.17 However, only a small number of the studied patients (10.8%) had taken the prescribed medication with gastro protective agents, either H2 antagonists or proton pump inhibitors (PPI).
The current study revealed that the majority of patients were taking less than the number of NSAIDs prescribed after consultation with a clinician. Overall, one fourth of the study participants expressed worry and concerns about the side effects of the drugs they were prescribed. There was also a patient who shared their prescribed medication with other family members.
Conclusion
In summary, as with other studies, as part of the rational pharmacotherapy of rheumatology; clinicians and pharmacists play a major role in educating and providing patients with the necessary details of the prescribed medications. Programs such as medication therapy adherence clinic (MTAC), which recently started at our rheumatology clinic and run by a pharmacist, have attained a positive response from patients. Factors such as knowledge, attitudes and motivation are particularly important in terms of patient compliance and the effectiveness of therapy. These factors may be influenced by the patient’s education level, gender, the type of the disease and medication, as well as doctor-patient relationship, and culture, etc. Further larger scale studies addressing this issue should be undertaken in the near future.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastrointestinal complications. J Rheumatol Suppl. 1999;56:18-24.
2. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee. Arthritis Rheum. 2000;43:1905-1915.
3. American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis. Arthritis Rheum. 2002;46:328-346.
4. De Vries TPGM, Henning RH, Hogerzeil HV, Fresle DA. Guide to Good Prescribing. World Health Organization, Action Programme on Essential Drugs, 1994. WHO/DAP/94:11.
5. De Vries TPGM. Presenting clinical pharmacology and therapeutics: a problem based approach for choosing and prescribing drugs. Br J Clin Pharmacol 1993; 35: 581-6.
6. WHO. (15-27 October 1998) Promoting rational drug use. Trainer’s guide. Accra, Ghana 1998.
7. Popovich NG. Ambulatory patient care. In: Gennaro AR, ed. Remington’s pharmaceutical sciences, 17th ed. Pennsylvania: Mack Publishing Company, 1985: 1681-701.
8. Edwards L, Roden DM. Principles of prescription order writing and patient compliance. In: Gilman AG, edr. Goodman & Gilman’s The pharmacological basis of therapeutics. Tenth edition. USA: McGraw-Hill, 2001: 1903-15.
9. Isacson D, Bingefors K. Attitudes towards drugs - a survey in the general population. Pharm World Sci 2002; 24: 104-10.
10. Ridout S, Water W, George CF. Knowledge of and attitudes to medicines in the Southampton community. Br J Clin Pharmacol 1986; 21: 701-702.
11. George CF, Waters WE, Nicholas JA. Prescription information leaflet: a pilot study in general practice. Br Med J 1983; 287: 1193-1196.
12. Hürriyet YILMAZ, Selim GÜREL, Oktay ÖZDEMİR; Turkish patients with osteoarthritis: Their awareness of the side effects of NSAIDs; The Turkish Journal of Gastroenterology 2005;16:89-92.
13. Wynne HA, Long A. Patient awareness of the side effects of non-steroidal anti inflammatory drugs (NSAIDs). Br J Clin Pharmacol 1996;42:253-256.
14. Jobanputra P, Arthur V, Pugh M, Spannuth F, Griffiths P, Thomas E, Sheeran T. Quality of care for NSAID users: Development of an assessment tool; Rheumatology 2005; 44: 633-637.
15. Ornbjerg LM, Andesen HB, Kryger P, Cleal B 2008; What do patient in Rheumatologic care know about the risk of NSAIDs? J Clin Rheumatol 2008;14:69-73.
16. Paul AD, Chanhan CK. Study of usage pattern of NSAIDs among difference practice categories in India clinical setting; Eur J Clin Pharmacol 2005;60:889-892.
17. Silvani MC, Motola D, Elisabetta Poluzzi, Ambrogio Bottoni; Gastrointestinal problems and concomitant medication in NSAID users: additional findings from a questionnaire based survey in Italy; Eur J Clin Pharmacol 2006; 62:235-241.
|