A near miss is defined as an error or deviation from standard procedures or policies discovered before the patient receives a transfusion that may lead to transfusion error.1 Although near-miss events are not actual errors of transfusion, reporting and investigation of near-miss events are vital in detecting steps and factors that have high chances of causing actual transfusion errors.2 Information such as causes of near-miss events, location, and medical personnel involved helps narrow down target areas for improvement.3
Doctors were among the most common profession associated with near-miss incidents in transfusion medicine in several international studies.3,4 Analyzing and identifying other possible factors associated with near-miss events amongst doctors can further improve blood transfusion practice safety. Information on which step of the transfusion process that errors frequently occur and the typical location for potential errors can be obtained. Common risk factors or causes of near misses among healthcare staff can be analyzed and investigated. These data help determine appropriate corrective and preventive actions to ensure transfusion safety.5
The study aimed to determine the prevalence and rate of near-miss events of transfusion practice in Hospital Universiti Sains Malaysia and the factors associated with near-miss events of transfusion practice amongst house officers (HO) in the hospital. This information can help us to plan for future interventions and implement proper corrective action with the main objective of having zero transfusion error in
our hospital.
Methods
This is a descriptive cross-sectional study and a case-control study conducted in a teaching hospital. All test requests for group, screen, and hold (GSH) and group and cross match (GXM) sent to the Transfusion Medicine Unit from January 2011 to December 2017 that fulfilled the inclusion and exclusion criteria were collected in a retrospective manner. Case and control groups were sampled from HOs who sent requests for GSH and GXM.
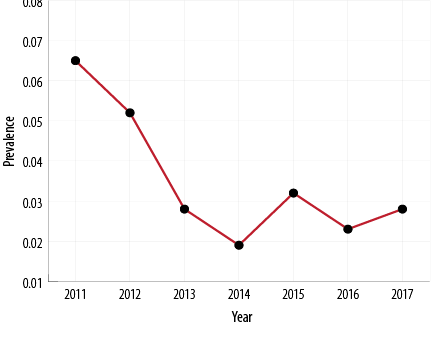
Figure 1: Trend of the yearly prevalence of near-miss events.
For the case group, all HO involved in near-miss events were included. For the control group, simple random sampling using Microsoft Excel was done among the list of HO who had sent in test requests which do not end up in a near-miss event.
The departments were divided into two main groups; medical-based (internal medicine, pediatrics, and accident and emergency) and surgical-based (surgery, orthopedics, and obstetrics and gynecology).
Near-miss events occurring in wards were categorized as clinical near miss. It is detected when there is a discrepancy between the ABO grouping of a newly received sample and pre-existing ABO grouping of the same patient recorded within the online system. According to our hospital standard operating procedure (SOP), when a near miss occurs, implicated sample need to be rejected and the ward should send a new sample for regrouping. HO will need to send an explanation letter regarding the near miss made to the head of transfusion medicine.
Table 1: Prevalence and rate of near-miss events analyzed with descriptive statistics.
|
83 |
242 004 |
0.034 |
1:2916 |
11.9 |
GSH: group, screen, and hold; GXM: group and cross match; CI: confidence interval.
*One event per number of test requests received.
Near miss occurring in a blood bank, also known as laboratory near miss, is detected when there is a discrepancy between the ABO grouping of a newly received sample and the pre-existing ABO group of the same patient in the online system record.
Data were analyzed using SPSS Statistics (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Determination of associated factors with the occurrence of near-miss events amongst HO were analyzed using simple logistic (SLR) and multiple logistic regression (MLR). The level of significance was determined at p-value < 0.050.
Table 2: Summary of causes of near-miss events using descriptive statistics.
|
Incorrect specimen handling |
4 (44.4) |
|
4 (4.8) |
1 every 60 501 |
|
Incorrect test interpretation |
5 (55.6) |
|
5 (6.0) |
1 every 48 401 |
|
Miscollected |
|
9 (12.2) |
9 (10.8) |
1 every 26 889 |
|
Mislabelled |
|
28 (37.8) |
28 (33.7) |
1 every 8 643 |
|
Unclassifiable |
|
37 (50.0) |
37 (44.6) |
1 every 6 541 |
*one event every number of requests.
Results
There were 83 near-miss events reported among 242 004 requests for GSH and GXM from 2011 to 2017. The prevalence of near-miss events among test requests was 0.034% (95% confidence interval (CI): 0.027–0.042) [Table 1]. Overall, there was a decreasing trend of near miss prevalence from 2011 until 2014 and a static trend from 2014 until 2017 [Figure 1].
Near-miss events of transfusion practice in our hospital were predominantly clinical near miss. Clinical near miss amounted to 74 events (89.2%), in contrast with laboratory near miss with only nine (10.8%) events [Table 2].
Most clinical near-miss events were of unclassifiable causes amounting to 37 events. In 30 events, there was no explanation letter handed in by involved medical personnel; hence, the exact mechanism of how the event occurred was unknown. In seven events, the near-miss events were of the previous sample in the past, and the blood grouping from the current sample is correct; hence, further investigation was not possible. Unclassifiable causes were categorized as clinical near miss as they were detected before sample testing in the transfusion medicine laboratory. Mislabelled and miscollected contribute to about 33.7% and 10.8%, respectively.
Table 3: Distribution of location of near-miss events and staff involved using descriptive statistics.
|
Wards |
|
|
|
|
|
Pediatric |
2 |
1 |
|
3 (3.6) |
|
Accident and emergency |
4 |
1 |
|
5 (6.0) |
|
Orthopedics |
6 |
|
|
6 (7.2) |
|
Surgery |
6 |
2 |
|
8 (9.6) |
|
Obstetrics and gynecology |
26 |
|
|
26 (31.3) |
|
Internal medicine |
25 |
1 |
|
26 (31.3) |
|
Lab |
|
|
|
|
|
Transfusion medicine unit |
|
|
9 |
9 (10.8) |
HO: house officer; MO: medical officer; MLT: medical laboratory technologist.
The majority of laboratory near miss were caused by incorrect interpretation of ABO and Rhesus blood grouping. Another cause of laboratory near miss was incorrect specimen handling, which included one case of assigning the wrong barcode sticker to another patient’s sample, one case of labeling mistake on blood grouping card, and two cases of mistakenly testing the wrong sample for a patient.
Most near-miss events involved HO, followed by medical laboratory technologist (MLT) and medical officer (MO) [Table 3]. Most clinical near-miss events were from both medical wards and obstetrics and gynecology wards. Laboratory near miss was the third most frequent location with 10.8% of cases.
Discussion
The prevalence of near-miss events in our hospital was low at 0.034% (95% CI: 0.027–0.042%). Similarly, a lower prevalence of near-miss events reported in India and Pakistan, which was 0.04% and 0.035%, respectively, among cross match samples.6 In contrast, a study by Elhence et al,7 and Fastman et al,8 reported a higher near miss reporting rate of 0.45% and 1.7%, respectively.
Table 4: Descriptive data of the house officers involved in the study (n = 166).
|
Age, year, mean (SD) |
25.7 (1.0) |
26.2 (1.2) |
|
Gender |
|
|
|
Male |
15 (35.7) |
54 (43.5) |
|
Female |
27 (64.3) |
70 (56.5) |
|
Race |
|
|
|
Malay |
37 (88.1) |
114 (91.9) |
|
Non-Malay |
5 (11.9) |
10 (8.1) |
|
Department |
|
|
|
Surgical-based wards |
26 (61.9) |
81 (65.3) |
|
Medical-based wards |
16 (38.1) |
43 (34.7) |
|
Time of request |
|
|
|
Non-office hour |
22 (52.4) |
74 (59.7) |
|
Office hour |
20 (47.6) |
50 (40.3) |
|
Posting |
|
|
|
1st and 2nd |
18 (42.9) |
47 (37.9) |
|
3rd and 4th |
14 (33.3) |
51 (41.1) |
|
5th and 6th |
10 (23.8) |
26 (21.0) |
|
Blood bank attachment |
|
|
|
No |
32 (76.2) |
100 (80.6) |
SD: standard deviation.
Sociodemographic characteristics of the case group and control group were summarized in Table 4. SLR and MLR analysis was performed [Table 5 and 6]. In MLR analysis, after adjusting for other variables, only age was significantly associated with HO involved in near-miss events. HO who are a year older decrease the odds of having a near miss event by 30.0% with 95% CI between 0.51
and 0.96.
Table 5: Associated factors of near-miss events amongst house officers by simple logistic regression (n = 166).
|
Age |
-0.362 |
0.70 |
0.51–0.96 |
0.027* |
|
Gender |
|
|
|
|
Male |
|
1 |
|
|
|
Female |
0.328 |
1.39 |
0.67–2.87 |
0.374 |
|
Race |
|
|
|
|
Malay |
|
1 |
|
|
|
Non-Malay |
0.432 |
1.54 |
0.50–4.80 |
0.456 |
|
Department |
|
|
|
|
Surgical-based wards |
|
1 |
|
|
|
Medical-based wards |
0.148 |
1.16 |
0.56–2.39 |
0.689 |
|
Time of request |
|
|
|
|
Non-office hour |
|
1 |
|
|
|
Office hour |
0.297 |
1.35 |
0.67–2.72 |
0.409 |
|
Posting |
|
|
|
|
1st and 2nd posting |
|
1 |
|
|
|
3rd and 4th posting |
-0.333 |
0.72 |
0.32–1.60 |
0.416 |
|
5th and 6th posting |
0.004 |
1.00 |
0.40–2.49 |
0.993 |
|
Blood bank attachment |
|
|
|
|
No |
|
1 |
|
|
β: regression coefficient; OR: odds ratio.
p < 0.050 taken as significant value at 95% confidence interval (CI).
Table 6: Associated factors of near-miss events amongst house officers by multiple logistic regression
(n = 166).
β: regression coefficient; OR: odds ratio. Forward and backward (likelihood ratio) methods were applied.
p < 0.050 taken as significant value at 95% confidence interval (CI).
Area under receiver operating characteristics = 62.0%.
Hosmer–Lemeshow test, p-value = 0.460.
Classification table overall percentage correct = 74.7%.
The yearly trend of near miss prevalence in our hospital showed an overall reducing pattern from 2011 to 2014. Our Hospital Transfusion Committee (HTC) has found increasing near-miss events amongst HO from the previous yearly audit. Therefore, an HTC meeting resulted in the commencement of one week blood bank attachment for HO in 2011. It was one of the suggested measures in the meeting to improve hemovigilance. This reducing trend can partly be credited to the increasing awareness amongst HO because of the blood bank attachment.
The predominant near miss cases in our hospital were clinical near miss (89.2%) compared to a laboratory near miss (10.8%). Karim et al,9 and the 2016 annual serious hazards of transfusion (SHOT) report4 also showed that most near misses occurred in clinical areas with 95.4% and 76.6%, respectively.In contrast, a study by Kaur et al,3 and Masken et al,10 reported that most incidents happened inside the transfusion laboratory, which were more than those occurring in the clinical services. However, this could be attributed to underreporting of clinical
near miss.
Most clinical near miss in our study was of unclassifiable causes because there was no explanation letter from the personnel involved, which reflected inadequate documentation of near miss reporting. Poor documentation of reporting may complicate hemovigilance efforts as the possible weak links were not being addressed. In general, proper reporting of any type of error may reduce the error from recurring in the future as it is an aspect of quality assurance of a healthcare system.11,12
We also categorized seven near-miss events with a previous sample under the ‘unclassifiable cause’ category. We were not able to investigate the cause of a prior event as a repeat sample confirmed that the near miss occurred in the previous sample. The reason for errors in the previous sample went undetected because there was no second sample sent during that first admission. The British Committee for Standards in Hematology (BCSH) has recommended for a second independent sample to be submitted for any first-time patient to confirm further that the first sample was indeed the patient’s sample.13 A transfusion error surveillance reported that areas in which a second sample regrouping was done had lower rates of wrong blood in tube (WBIT).14 However, it has disadvantages such as increased cost, delay in providing blood to a patient, and is troublesome to patient and blood
sample taker.15
Mislabeling is the second most common cause of clinical near miss in our hospital (33.7%). Our hospital’s mislabeling incidents (one every 8643 samples) were less frequent than the rate reported by Elhence et al,7 (1 in 303 samples). Lower rates of mislabeled were reported by Grimm et al,16 and College of American Pathologists,17 which were only 1.12% and 0.74% of samples submitted for ABO typing, respectively.
We reported miscollected samples at 10.8%, with a rate of one in every 26 889 requests. Tondon et al,18 and Elhence et al,7 reported higher miscollection rates of one in 1489 and one in 2395, respectively.Biomedical Excellence for Safer Transfusion collaborative reported that the rate of miscollected samples ranged between 0.3 and 0.9 per 1000 samples.8 Previous studies in Pakistan and Iran reported higher miscollected samples at 61.9% and 58%, respectively.9,19
The result of our study has shown that the leading cause of near miss was clinical near miss, with mislabelling and miscollection being contributory causes. Some of the reasons given by the HO were that sample tubes were labeled before sample collection, and labelling and collection were by two different HO. Some were attributed to the chaotic working condition of wards. Few cases of mislabeling also occurred due to taking blood samples from several patients at the same time and the sample was labeled away from the location of blood-taking. Labeling away from the patient’s location was one of the major factors causing WBIT.20 Khetan et al,21 reported that more than half of their staff had labeled the tube at the counter and then collected blood from the intended patient, highlighting that incorrect practice was common in some centers.
Therefore, an area of improvement would involve strict adherence to blood bank labeling policy. O’Neill et al,22 as demonstrated a reduction in the numbers of WBIT and mislabeled after the introduction of an educational campaign re-emphasizing proper sample labeling and the implementation of a strict labeling policy.
Although the incorrect interpretation of blood group testing and improper specimen handling only contributed to a small part of near-miss events, the implications of incorrectly interpreting blood group testing can lead to grave consequences. Our hospital had a higher proportion of laboratory near miss due to incorrect blood grouping interpretation compared to a report from SHOT UK 2017.4 A study in India reported the misinterpretation of blood grouping represented only 1.1% and 0.6% of total errors, respectively.2,23 We observed that having a second MLT to reconfirm a blood grouping test is needed as these near-miss events have been discovered in that manner. Our hospital had made it compulsory for a second MLT to reconfirm a blood grouping test since 2017. The higher percentage of a laboratory near miss showed weakness from the technical aspect of the transfusion process. Regular training, as well as retraining of implicated personnel, can be beneficial in improving rates of unwanted laboratory errors.24
Another contributory cause of laboratory near miss was incorrect specimen handling. Most occurred because the laboratory technologists were distracted when handling samples. In the blood bank, possible causes of distraction included frequent phone calls made by the wards to confirm cross matching results. There were also urgent requests calls from clinicians and pressure from clinicians to release blood early, which were the same reasons described in a tertiary care hospital in India.3
Aside from that, a lower level of automation in some pretransfusion testing steps may have also contributed to errors in the laboratory.25 There are higher risks of errors by human factors when there is more reliance on the MLT to perform crucial steps manually as compared to steps performed
by machine.26
More than half of the near-miss events in our hospital involved doctors, specifically HO (83.1%). This is because most blood-taking activity is performed by the junior doctors or HO, and in only a minority of situations by medical officers and nurses. Interestingly, Karim et al,9 had a similar finding whereby interns and postgraduate trainees were mainly involved in WBIT. Likewise, in the 2016 Annual SHOT report,4 and the study by Varey et al,20 doctors were involved in a higher percentage than midwives, nurses, healthcare assistants, phlebotomists, and medical students. Similarly, in Austria and Germany, most blood taking was also performed by junior doctors. This exposed junior doctors to more chances of having a near miss event if they did not follow proper precautionary steps in blood taking. Although there are specified procedures in each center, the actual practice of blood taking is cultivated on an individual basis.27,28
MOs were involved in the least amount of near-miss events in our hospital. They are not responsible for most blood taking jobs in wards. Their longer working experience may have contributed to more awareness in ensuring transfusion safety.
One possible solution to reduce near misses is to have a dedicated phlebotomist or staff with proper phlebotomy training.29 A systemic review has shown decreased incidences of WBIT with the availability of dedicated and trained phlebotomy service.30
In our hospital, most near-miss events were from medical wards and obstetrics and gynecology wards. A study in India reported the two most common places of requisition errors were emergency services and medical wards.31 Varey et al,20 reported that the highest incidence of WBIT was in the medical and pediatrics department. Previous studies revealed that the high number of near miss cases in the obstetrics and gynecology department were attributed to a large number of received antenatal samples.20,32,33
We reported that the laboratory was the third most common area, accounting for 10.8% of cases, which is similar to a study by Lundy et al,34 that reported laboratory near misses accounted for 10% of cases. The US Food and Drug Administration reported 33.0% of transfusion-related mortalities from acute hemolysis occurred within blood bank.35 In contrast, other studies reported only 7.0–13.0% of diagnostic laboratory errors occur during the analytical phase when compared to pre-analytical or post-analytical phases.36,37
Our study found a significant association between the ages of doctors with the occurrence of near-miss events. Doctors who are a year older decrease the odds of having a near miss event by 30.0%. There was no exact study analyzing the association of age with near-miss events in transfusion practice amongst doctors. Tanaka et al,38 reported, having fewer years of experience, implying a younger age was associated with near-miss events, which is similar to
our study.
We observed a predominance of near-miss events among HO in surgical-based wards (61.9%) in comparison to medical-based wards (38.1%). One possible contributing factor is the higher number of samples sent from these wards as all patients admitted would have their samples sent for either GSH or GXM as a prerequisite before any
surgical procedure.
Another relevant factor that was analyzed was the timing of requests. We found that more than half of the HOs involved in near-miss events sent the sample requests outside of office hours (52.4%). A study in Hong Kong showed that most near misses occurred during on-call shifts, which was attributed to a higher number of procedures per person and more decision-making during on-call hours.39 Das et al,2 and Kaur et al,3 observed a higher portion of errors outside of blood bank occurred at night shift, which was attributed to a higher workload with less staff on duty available during the night shift.
We observed that almost half of the HO (42.9%) involved with near-miss events had recently started their service. They were in their first and second rotation posting of their housemanship service. A study by Chow et al,39 on the association of near-miss events among junior doctors with their working experience revealed that doctors within their first month of working have double the odds of having near miss when compared with those within subsequent months. Most HO in their first rotation have minimal working experience and may find it difficult to navigate through unfamiliar settings and working practices. New doctors were overwhelmed with many skills they needed to learn within a short period in each posting. Therefore, the practice of proper blood taking may have taken a
back seat.27
In 2011, our hospital began including blood bank attachment for HO as part of housemanship training. During this attachment, part of the teaching included an emphasis on necessary precautions and standard operating procedures of the transfusion process. We observed that among the HO who were involved in a near miss, most (76.2%) did not attend any blood bank attachment before the event. Results from a study by Lundy et al,34 concluded that training that includes hemovigilance and transfusion safety is necessary. Transfusion education amongst medical students and residents should be enhanced, considering its impact on clinical medicine.40
Our study found that there were inadequacies in positive patient identification leading to mislabeled and miscollected cases. In a few cases, it resulted from staff labeling pre-printed stickers on the wrong tube sample. A printed sticker of patient details was meant to speed up the labeling process. However, it inadvertently resulted in mislabeling errors when the wrong sticker was printed for an intended patient. Despite having the wrong sticker, the blood taker also failed to reconfirm the details on the sticker with the patient before proceeding to take blood.
One suggestion would be to abolish the use of pre-printed stickers and make it compulsory for pretransfusion samples to be labeled at the bedside and handwritten instead. Gonzalez-Porras et al,41 reported that inappropriately labeled samples had a significant association with the use of pre-printed labels compared to handwritten labels. BCSH guidelines recommended against the use of pre-printed labels. Only those printed ‘on-demand’ and attached to the patient’s sample tube bedside at the time of blood taking were accepted. They also emphasized the need for accurate and legible handwritten labels.42
Another suggestion would be using an electronic positive patient identification (i.e., handheld barcode scanners to confirm the patient’s identity via barcoded patient wristbands before sample collection). Reduction of labeling errors were reported after the implementation of bar code technology.43
Conclusion
The prevalence of near-miss events in our center was relatively low. Proper reporting is vital and should be scrutinized to determine any corrective and preventive action. A joint effort involving both the clinical and laboratory sides are necessary to improve transfusion safety. Additionally, encouraging healthcare staff compliance to guidelines is a must. Our analysis had found that older doctors have lesser odds of being involved in a near miss event. Therefore, proper education and adequate training in clinical and laboratory areas are imperative to minimize the risk of mistransfusion.
Disclosure
The authors declared no conflicts of interest. No funding was received from this study.
Acknowledgements
The authors thanked all transfusion medicine staff for their precious assistance with data collection and analysis.
references
- 1. Thomas D, Thompson J and Ridler B. All blood counts: a manual for blood conservation and patient blood management. TFM Publishing Limited; 2016.
- 2. Das S, Chakrabarty R, Zaman R. Monitoring errors in a blood bank immunohematology laboratory: Iimplementing strategies for safe blood transfusion. Global Journal of Transfusion Medicine 2017;2(2):118-123.
- 3. Kaur G, Kaur G, Kaur P. Nature and causes of errors in the blood transfusion chain – a step towards patient safety. ISBT Sci Ser 2019;14(2):193-200.
- 4. Bolton-Maggs PH, Poles D, Watt A, Thomas D. On behalf of the serious hazards of transfusion (SHOT) steering group. The 2016 Annual SHOT Report 2017, SHOT Office, Manchester Blood Centre, Manchester, UK; 2016.
- 5. Sheikhtaheri A. Near misses and their importance for improving patient safety. Iran J Public Health 2014 Jun;43(6):853-854.
- 6. Sidhu M, Meenia R, Akhter N, Sawhney V, Irm Y. Report on errors in pretransfusion testing from a tertiary care center: a step toward transfusion safety. Asian J Transfus Sci 2016 Jan-Jun;10(1):48-52.
- 7. Elhence P, Shenoy V, Verma A, Sachan D. Error reporting in transfusion medicine at a tertiary care centre: a patient safety initiative. Clin Chem Lab Med 2012 Nov;50(11):1935-1943.
- 8. Fastman BR, Kaplan HS. Errors in transfusion medicine: have we learned our lesson? Mt Sinai J Med 2011 Nov-Dec;78(6):854-864.
- 9. Karim F, Ali M, Rashid A, Shaikh MS, Karim M, Moiz B. Monitoring near-miss events in a hospital blood bank. ISBT Sci Ser 2017;12(3):381-385.
- 10. Maskens C, Downie H, Wendt A, Lima A, Merkley L, Lin Y, et al. Hospital-based transfusion error tracking from 2005 to 2010: identifying the key errors threatening patient transfusion safety. Transfusion 2014 Jan;54(1):66-73.
- 11. Oremakinde AA, Bernstein M. A reduction in errors is associated with prospectively recording them. J Neurosurg 2014 Aug;121(2):297-304.
- 12. Roxby D, Magrin G. Application of quality principles in clinical transfusion laboratory practice. ISBT Sci Ser 2011;6(2):291-295.
- 13. Milkins C, Berryman J, Cantwell C, Elliott C, Haggas R, Jones J, et al; British Committee for Standards in Haematology. Guidelines for pre-transfusion compatibility procedures in blood transfusion laboratories. Transfus Med 2013 Feb;23(1):3-35.
- 14. Strauss R, Downie H, Wilson A, Mounchili A, Berry B, Cserti-Gazdewich C, et al. Sample collection and sample handling errors submitted to the transfusion error surveillance system, 2006 to 2015. Transfusion 2018 Jul;58(7):1697-1707.
- 15. Glisch C, Jawa Z, Brener A, Carpenter E, Gottschall J, Treml A, et al. Evaluation of a two-sample process for prevention of ABO mistransfusions in a high volume academic hospital. BMJ Open Qual 2018 Jul;7(3):e000270.
- 16. Grimm E, Friedberg RC, Wilkinson DS, AuBuchon JP, Souers RJ, Lehman CM. Blood bank safety practices: mislabeled samples and wrong blood in tube–a Q-Probes analysis of 122 clinical laboratories. Arch Pathol Lab Med 2010 Aug;134(8):1108-1115.
- 17. Novis DA, Lindholm PF, Ramsey G, Alcorn KW, Souers RJ, Blond B. Blood bank specimen mislabeling: a college of American pathologists Q-probes study of 41 333 blood bank specimens in 30 institutions. Arch Pathol Lab Med 2017 Feb;141(2):255-259.
- 18. Tondon R, Pandey P, Mickey KB and Chaudhary R. Errors reported in cross match laboratory: a prospective data analysis. Transfusion and Apheresis Science 2010;43(3):309-314.
- 19. Adibi H, Khalesi N, Ravaghi H, Jafari M, Jeddian AR. Root-cause analysis of a potentially sentinel transfusion event: lessons for improvement of patient safety. Acta Med Iran 2012;50(9):624-631.
- 20. Varey A, Tinegate H, Robertson J, Watson D, Iqbal A. Factors predisposing to wrong blood in tube incidents: a year’s experience in the North East of England. Transfus Med 2013 Oct;23(5):321-325.
- 21. Khetan D, Katharia R, Pandey HC, Chaudhary R, Harsvardhan R, Pandey H, et al. Assessment of bedside transfusion practices at a tertiary care center: a step closer to controlling the chaos. Asian J Transfus Sci 2018 Jan-Jun;12(1):27-33.
- 22. O’Neill E, Richardson-Weber L, McCormack G, Uhl L, Haspel RL. Strict adherence to a blood bank specimen labeling policy by all clinical laboratories significantly reduces the incidence of “wrong blood in tube”. Am J Clin Pathol 2009 Aug;132(2):164-168.
- 23. Bolton-Maggs PH, Cohen H. Serious hazards of transfusion (SHOT) haemovigilance and progress is improving transfusion safety. Br J Haematol 2013 Nov;163(3):303-314.
- 24. Koh MB, Alcantara R. Transfusion errors and management. ISBT Sci Ser 2009;4(n2):216-220.
- 25. Vuk T, Barišić M, Očić T, Mihaljević I, Sarlija D, Jukić I. Error management in blood establishments: results of eight years of experience (2003-2010) at the Croatian institute of transfusion medicine. Blood Transfus 2012 Jul;10(3):311-320.
- 26. South SF, Casina TS, Li L. Exponential error reduction in pretransfusion testing with automation. Transfusion 2012 Aug;52(8):81S-87S.
- 27. Jeffcott S. Reducing harm in blood transfusion ‐ investigating the human factors behind ‘wrong blood in tube’ (WBIT) events in the emergency department. Melbourne, Vic., Australia: Victorian Managed Insurance Authority 2010;99.
- 28. Simundic A-M, Cornes M, Grankvist K, Lippi G, Nybo M, Kovalevskaya S, et al. Survey of national guidelines, education and training on phlebotomy in 28 European countries: an original report by the European federation of clinical chemistry and laboratory medicine (EFLM) working group for the preanalytical phase (WG-PA). Clinical chemistry and laboratory medicine (CCLM) 2013;51(8):1585-1593.
- 29. Warekois RS, Richard Robinson N. Phlebotomy: worktext and procedures manual. Elsevier Health Sciences; 2015.
- 30. Cottrell S, Watson D, Eyre TA, Brunskill SJ, Dorée C, Murphy MF. Interventions to reduce wrong blood in tube errors in transfusion: a systematic review. Transfus Med Rev 2013 Oct;27(4):197-205.
- 31. Jain A, Kumari S, Marwaha N, Sharma RR. The role of comprehensive check at the blood bank reception on blood requisitions in detecting potential transfusion errors. Indian J Hematol Blood Transfus 2015 Jun;31(2):269-274.
- 32. Figueroa PI, Ziman A, Wheeler C, Gornbein J, Monson M, Calhoun L. Nearly two decades using the check-type to prevent ABO incompatible transfusions: one institution’s experience. Am J Clin Pathol 2006 Sep;126(3):422-426.
- 33. Victoria State Government. Serious transfusion incident report 2016-2017; 2018.
- 34. Lundy D, Laspina S, Kaplan H, Rabin Fastman B, Lawlor E. Seven hundred and fifty-nine (759) chances to learn: a 3-year pilot project to analyse transfusion-related near-miss events in the Republic of Ireland. Vox Sang 2007 Apr;92(3):233-241.
- 35. Simon TL, Snyder EL, Stowell CP, Strauss RG, Solheim BG, Petrides M. Rossi’s principles of transfusion medicine. 4th ed. Wiley-Blackwell; 2009.
- 36. Najat D. Prevalence of pre-analytical errors in clinical chemistry diagnostic labs in Sulaimani city of Iraqi Kurdistan. PLoS One 2017 Jan;12(1):e0170211.
- 37. Cornes MP, Atherton J, Pourmahram G, Borthwick H, Kyle B, West J, et al. Monitoring and reporting of preanalytical errors in laboratory medicine: the UK situation. Ann Clin Biochem 2016 Mar;53(Pt 2):279-284.
- 38. Tanaka K, Otsubo T, Tanaka M, Kaku A, Nishinoue N, Takanao T, et al. Similarity in predictors between near miss and adverse event among Japanese nurses working at teaching hospitals. Ind Health 2010;48(6):775-782.
- 39. Chow KM, Szeto CC, Chan MH and Lui SF. Near-miss errors in laboratory blood test requests by interns. QJM 2005;98(10):753-756.
- 40. Panzer S, Engelbrecht S, Cole-Sinclair MF, Wood EM, Wendel S, Biagini S, et al. Education in transfusion medicine for medical students and doctors. Vox Sang 2013 Apr;104(3):250-272.
- 41. Gonzalez-Porras JR, Graciani IF, Alvarez M, Pinto J, Conde MP, Nieto MJ, et al. Tubes for pretransfusion testing should be collected by blood bank staff and hand labelled until the implementation of new technology for improved sample labelling. Results of a prospective study. Vox Sang 2008 Jul;95(1):52-56.
- 42. British Committee for Standards in Haematology (BCSH). Guideline on the administration of blood components. Appendix 2009;6:51.
- 43. Morrison AP, Tanasijevic MJ, Goonan EM, Lobo MM, Bates MM, Lipsitz SR, et al. Reduction in specimen labeling errors after implementation of a positive patient identification system in phlebotomy. Am J Clin Pathol 2010 Jun;133(6):870-877.