Diabetes mellitus is a chronic disease and one of the most common systemic metabolic disorders with an increasing prevalence across the globe. It has been called “the silent epidemic” by the World Health Organization.1 According to the statistics released by the International Diabetes Federation, more than 382 million people throughout the world had diabetes in 2013, 46.0% of whom had not been yet diagnosed. The average global prevalence is 8.3%.2 In Iran this figure is 11.3%, and almost half of the patients with diabetes are not aware of the disease. It is predicted that the number of the people who have diabetes will triple over the next 15 years meaning that one out of every five Iranians would be afflicted by or exposed to the risk of the condition.3
In Iran, the annual per capita medical costs of diabetic blindness, kidney failure, and amputation are nearly US$ 2 000, 45 000, and 29 500, respectively. Furthermore, the lack of diabetes control in Iran leads to approximately US$ 7 million of annual direct medical expenditure.4 Studies have shown that cardiovascular risk factors are significantly higher among younger type 2 diabetics (< 60 years), particularly females, (e.g., dyslipidemia, smoking, hypertension, high body mass index (BMI)). This group of diabetics requires a more stringent therapy approach.5 On the other hand, its associated cardiovascular and renal complications could, in turn, lead to unprecedented increases in healthcare expenditure on a single condition (like diabetes) and eventually bankrupt governments.6
In recognition of the increased prevalence and expensive diagnosis and control of diabetes and its acute and chronic complications, as well as the reduction of individual income due to the decreased efficiency, increased disability, and premature death caused by diabetes, it is essential to conduct effective interventions to control the complications and improve the quality of life (QOL) of those suffering the condition.2 According to Aaronson: “Quality of life is patient’s perspectives on their ability to live useful, meaningful, fulfilling lives even while burdened with disease”.7 Moreover, since patients themselves are primarily responsible for managing their disease8, supporting patients self-management is key in effective diabetic care.9 Thus, diabetes, as a chronic disease, requires a self-management approach.10
One of the most important methods to increase self-management and diabetes management is to provide appropriate training. Studies have shown that nurses play a key role in improving the self-management11 and QOL of patients.12 In addition, they are frequently responsible for the major components of self-management training programs12 including delivering individual and group training as well as offering group counseling, providing essential information via the internet and phone, and holding any follow-up sessions (e.g., such as home meetings) to provide relevant training.13,14 The use of group discussion as a medium for delivering education and training enable us to access the emotions and experiences of 5–15 individuals at the same time. Therefore, it has been proposed as an ideal approach to investigate individuals’ emotions and beliefs about diseases.15
Several studies have demonstrated the positive effect of various interventions on controlling diabetes. The interventions investigated in these studies include modifying lifestyle through improving nutritional status, increasing physical activity, quitting smoking,16–19 controlling and following-up the patients by nurses;20 performing self-care interventions,21 and engaging in interventions at the societal level.22 Self-management training based on group discussions is a simple and supportive method, for which there is, to date, little evidence in the Iranian population, particularly among patients with type 2 diabetes. The increased number of patients with diabetes and the lack of a regular self-management program for them motivated the researcher to conduct an interventional study with an emphasis on the nurses’ role. The purpose of the current study was to determine the effect of group discussion-based education on self-management in patients with type 2 diabetes.
Methods
We conducted an unblinded randomized control trial with two parallel arms on patients with type 2 diabetes. Participant recruitment was done from 10 October to 3 December 2014.
The research population included patients aged 30–70 years old with no mental health conditions, diagnosed with type 2 diabetes for at least one year. The exclusion criteria included having a serious physical or mental disorder during the intervention, participating in similar training and research sessions during the study, and being absent for more than two sessions.
The sample size was calculated based on Shirazi et al.3 Considering β = 0.20, α = 0.05, S1 = 1.83, S2 = 1.71, μ1 = 5.97, and μ2 = 7.12. A subject sample size of 37 subjects in each group was determined. Considering a possible dropout, a total of 230 patients were reviewed, 176 were enrolled, and ultimately reduced the number of samples in each group to 45 subjects.
The research was conducted with adults with type 2 diabetes mellitus referred to the Madani Hospital diabetes clinic, Khoy, Iran. The Madani Hospital clinic is the largest diabetes mellitus referral center in the North West Azerbaijan province, and is governed by Urmia University of Medical Sciences. About 1 800 people with diabetes mellitus are registered in this center. The researchers visited the clinic identifying potentially eligible participants. Following recruitment, the participants were then enrolled into the study and completed the sociodemographic information and Lin’s self-management questionnaire.
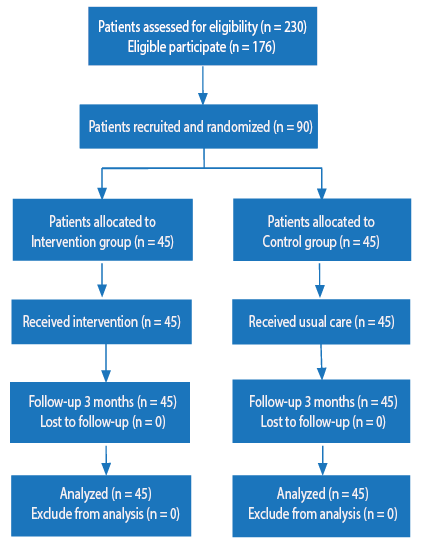
Figure 1: Study flowchart.
The study was registered under the code IRCT2014051717509N2 in the Iranian registry of clinical trials and was approved under the code IR.umsu.rec.1392.164 in the ethics council of Urmia University of Medical Sciences. All subjects were informed that participation was voluntary and assured that their personal information would remain confidential. All participants provided written consent before inclusion within the study.
Eligible patients were randomly allocated into one of two groups, one who received group discussion-based education (intervention group), and the other routine care including weight and vital signs control, laboratory tests, oral medications, and insulin adjustment (control group). Allocation was random using an even and odd method and an allocation ratio of 1:1. Random allocation was performed by a person uninvolved in sampling and data collection.
The research method included four stages. Before the group discussion, the researchers introduced the objectives of the study, and participants completed the initial assessment questionnaire. To develop and prepare the training materials and specify the time and content of the group discussion sessions, a needs assessment was performed so that the training interventions were based on the existing gap (the gap between the current and desirable levels of knowledge and skill of the patients).
The group discussion sessions were held with the participation of 15 individuals seated in a circular setting. This took place over eight sessions for each group running once a week for 1–1.5 hours over a period of eight weeks. The benefits for individuals in adopting healthy lifestyles, self-adjustment, interaction with health experts, and blood sugar control were discussed, and the participants were able to share their problems and experiences with each other. They also entered purposeful discussions to understand successful experiences of others in managing their condition. The topics discussed emphasized the patient-centered process based on the assessment of the patients’ needs and abilities by reviewing their experiences and knowledge, identifying and assessing their diabetes-specific needs including their perceived self-care obstacles. They also covered the development of individual strategies for promoting mental health and changing behavior, nutrition management and lifestyle, sensitivity in the method of measurement of blood sugar and other parameters as well as interpretation of the results, and the necessity of exercise and physical activities. Finally, they also discussed the prevention, diagnosis, and treatment of acute complications and the means of continuous communication with the health care team, and following-up their self-management behaviors. During the group discussion, while participating in the discussion and presenting the core concepts, the researcher also played the role of the group leader to guide the discussion. Finally, the materials were summarized by the participants, and the content of the subsequent session (according to the given plan) were specified.
Eventually, at the follow-up stage, the participants were encouraged to telephone the researcher for clarification or support with any further questions or problems arising. By the end of the follow-up period (three months), all subjects were again invited to the diabetes clinic to complete the post-intervention questionnaire (Lin’s self-management questionnaire).
Table 1: Demographic characteristics of patients in the intervention and control groups.
|
Gender |
|
|
|
|
|
|
Male |
14 |
31.1 |
11 |
24.4 |
0.480 |
|
Female |
31 |
68.8 |
34 |
75.5 |
|
Marital status |
|
|
|
|
|
|
Married |
39 |
86.6 |
40 |
88.98 |
0.750 |
|
Single |
6 |
13.3 |
5 |
11.1 |
|
Employment status |
|
|
|
|
|
|
Unemployed |
30 |
66.6 |
33 |
73.3 |
0.260 |
|
Employed |
8 |
17.7 |
3 |
6.7 |
|
Self-employed |
7 |
15.5 |
9 |
20.0 |
|
Educational status |
|
|
|
|
|
|
Low literacy |
39 |
86.6 |
42 |
93.3 |
0.290 |
|
Diploma or higher |
6 |
13.3 |
3 |
6.6 |
|
Duration of type 2 diabetes, years |
|
|
|
|
|
|
< 5 |
13 |
28.8 |
13 |
28.9 |
0.270 |
|
6–10 |
13 |
28.8 |
7 |
15.5 |
|
> 10 |
19 |
42.2 |
25 |
55.5 |
|
Type of treatment |
|
|
|
|
|
|
Oral medications |
33 |
73.3 |
33 |
73.3 |
0.850 |
|
Insulin |
4 |
8.8 |
6 |
13.3 |
|
Therapeutic regimen |
2 |
4.4 |
2 |
4.4 |
|
All three |
6 |
13.3 |
4 |
8.8 |
|
Family history of type 2 diabetes |
|
|
|
|
|
|
Yes |
28 |
62.2 |
33 |
73.3 |
0.260 |
|
No |
17 |
37.7 |
12 |
26.6 |
|
Smoking |
|
|
|
|
|
|
Yes |
2 |
4.4 |
3 |
6.7 |
0.650 |
|
No |
43 |
95.5 |
42 |
93.3 |
|
Education history |
|
|
|
|
|
|
Yes |
6 |
13.3 |
4 |
8.8 |
0.500 |
|
No |
39 |
86.7 |
41 |
91.1 |
|
Complications |
|
|
|
|
|
|
Yes |
25 |
55.5 |
27 |
60.0 |
The data collection instruments in this research included a demographic questionnaire and Lin’s self-management questionnaire. The demographic questionnaire was composed of 12 items including age, sex, marital status, family income, duration of diabetes morbidity, family history of diabetes, and diabetes-associated complications.
The diabetes self-management instrument developed by Lin et al,23 can be used to assess how patients with type 2 diabetes take care of themselves, to implement interventions tailored to the needs of individual patients, and to develop patient-centered teaching materials. Lin’s self-management dimensions questionnaire included five dimensions: self-organization (10 items), self-adjustment (nine items), interaction with health experts and influential individuals (nine items), blood sugar self-monitoring (four items), and adherence to diet (three items), which comprised a total of 35 items. The English version of the questionnaire was measured using the five-item Likert scale. The scoring of each item ranged from never (1) to always (5) so that the self-management total score varied from 35 to 175, and the higher score represented better self-management. The validity and reliability of this instrument in Iran were achieved with the confidence level of 87% by Tol et al.4 The content validity method was used to obtain the scientific validity of the collection tool and for the reliability of the questionnaire. The internal correlation method was used, where it was calculated Cronbach’s alpha (α) for dimensions; self-organization (α = 0.88), self-adjustment (α = 0.88), interaction with health experts and influential individuals (α = 0.79), blood sugar self-monitoring (α = 0.92), and adherence to diet (α = 0.87).
Data analysis was performed using SPSS Statistics (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0. Chicago, SPSS Inc.). After collecting the data, the descriptive and inferential statistics was used for data analysis. To investigate the difference in demographic features between the two groups the chi-square and Fisher’s exact tests were used. The independent and paired t-tests were used to compare the mean scores of self-management status in different areas and the total self-management before and after the study in both groups. A p-value < 0.050 was considered statistically significant.
Results
Of the 230 patients reviewed, 176 potentially eligible patients were invited to enroll in the study. Of them, 90 patients were recruited and randomized; 45 received interventions and 45 received usual care [Figure 1].
Results of chi-square test showed no statistically significant difference between the demographic variables in the intervention and control groups. In both groups, the majority of the subjects were female, married, and with an education level below high school diploma. Additionally, they had a family history of type 2 diabetes, had diabetes for more than 10 years, and often used pills as treatment [Table 1].
Using an independent t-test, there was no significant difference between the intervention and control groups in terms of the mean age (p = 0.900), BMI (p = 0.600), number of children (p = 0.510), and monthly income (p = 0.640) [Table 2].
Table 2: Comparing demographic characteristics in studied patients in both groups.
|
Age, years |
52.6 ± 8.0 |
52.4 ± 7.1 |
0.12 |
88 |
0.900 |
|
BMI |
28.2 ± 3.9 |
27.7 ± 4.1 |
0.53 |
88 |
0.600 |
|
Number of children |
3.8 ± 1.7 |
4.1 ± 2.0 |
-0.66 |
88 |
0.510 |
Data given as mean ± standard deviation. BMI: body mass index.
The difference of the mean scores in the dimensions of self-organization (p = 0.750), self-adjustment (p = 0.230), interaction with health experts (p = 0.170), blood sugar self-monitoring (p = 0.120), adherence to the proposed diet (p = 0.170), and total self-management criterion (p = 0.190) before the group discussion indicated no statistically significant difference between the intervention and control groups. However, after the group discussion, there was a statistically significant difference between the two groups in all dimensions and total self-management criterion [Table 3].
Table 3: Mean score of self-management dimensions in studied patients between the two groups before and after group discussion.
|
Self-organization |
Before |
30.3 ± 7.3 |
29.8 ± 8.6 |
0.32 |
88 |
0.750 |
|
After |
43.3 ± 4.6 |
29.8 ± 6.6 |
11.18 |
88 |
< 0.001 |
|
Difference |
12.9 ± 5.8 |
-0.0 ± 5.1 |
11.24 |
88 |
< 0.001 |
|
Self-adjustment |
Before |
27.2 ± 9.2 |
24.9 ± 8.0 |
1.20 |
88 |
0.230 |
|
After |
38.6 ± 4.2 |
24.9 ± 8.0 |
10.12 |
88 |
< 0.001 |
|
Difference |
11.4 ± 8.1 |
0.0 ± 6.1 |
7.53 |
88 |
< 0.001 |
|
Interaction with health experts |
Before |
26.6 ± 7.9 |
24.2 ± 8.5 |
1.37 |
88 |
0.170 |
|
After |
35.3 ± 5.0 |
23.9 ± 7.0 |
8.79 |
88 |
< 0.001 |
|
Difference |
8.6 ± 7.8 |
-0.3 ± 2.6 |
7.31 |
88 |
< 0.001 |
|
Blood sugar self-monitoring |
Before |
12.7 ± 3.8 |
11.3 ± 4.3 |
1.59 |
88 |
0.120 |
|
After |
17.7 ± 1.9 |
11.7 ± 3.6 |
9.63 |
88 |
< 0.001 |
|
Difference |
5.0 ± 3.9 |
0.4 ± 2.7 |
6.42 |
88 |
< 0.001 |
|
Adherence to proposed diet |
Before |
12.0 ± 2.4 |
11.2 ± 2.5 |
1.38 |
88 |
0.170 |
|
After |
14.6 ± 0.9 |
11.6 ± 2.5 |
7.49 |
88 |
< 0.001 |
|
Difference |
2.6 ± 2.5 |
0.4 ± 1.3 |
5.22 |
88 |
< 0.001 |
|
Before |
108.8 ± 23.8 |
103.3 ± 28.8 |
0.98 |
88 |
0.190 |
|
After |
149.7 ± 13.1 |
103.8 ± 24.1 |
11.38 |
88 |
< 0.001 |
The difference in the mean scores in dimensions of self-organization (p = 0.950), self-adjustment (p = 1.000), interaction with health experts (p = 0.430), blood sugar self-monitoring (p = 0.310), adherence to the proposed diet (p = 0.051), and total self-management criterion (p = 0.840) indicated no statistically significant difference before and after the group discussion. However, in the intervention group, there was a statistically significant difference in all dimensions and the total self-management criterion [Table 4].
Table 4: Mean score of self-management dimensions in studied patients within both groups before and after group discussion.
|
Self-organization |
Intervention |
30.6 ± 7.3 |
43.3 ± 4.6 |
-14.98 |
44 |
< 0.001 |
|
Control |
29.8 ± 8.6 |
29.8 ± 6.6 |
0.06 |
44 |
0.950 |
|
Self-adjustment |
Intervention |
27.2 ± 9.2 |
38.6 ± 4.2 |
-9.44 |
44 |
< 0.001 |
|
Control |
24.9 ± 8.8 |
24.9 ± 8.0 |
0.00 |
44 |
1.000 |
|
Interaction with health experts |
Intervention |
26.6 ± 7.9 |
35.3 ± 5.0 |
-7.44 |
44 |
< 0.001 |
|
Control |
24.2 ± 8.5 |
23.9 ± 7.0 |
0.80 |
44 |
0.430 |
|
Blood sugar self-monitoring |
Intervention |
12.7 ± 3.8 |
17.7 ± 1.9 |
-8.54 |
44 |
< 0.001 |
|
Control |
11.3 ± 4.3 |
11.7 ± 3.6 |
-1.03 |
44 |
0.310 |
|
Adherence to the proposed diet |
Intervention |
12.0 ± 2.4 |
14.6 ± 0.9 |
-6.92 |
44 |
< 0.001 |
|
Control |
11.2 ± 2.5 |
11.6 ± 2.5 |
-2.54 |
44 |
0.051 |
|
Intervention |
109.0 ± 23.2 |
149.7 ± 13.1 |
-13.92 |
44 |
< 0.001 |
Discussion
Our findings indicated that group discussion improved self-management in patients with diabetes. The growth of the elderly population and increased prevalence of chronic diseases has meant health care providers’ have started to focus on preparing patients to be active participants in caring for and managing their health problems.24 In this regard, self-management of chronic diseases as one of the major strategies for changing a patient to an active member in the treatment process is of
significant importance.25
The intervention significantly affected both the selected dimensions and the total self-management score after participation in the group discussion sessions. Previous studies of similar interventions have shown findings that are both consistent and inconsistent with our findings. Kulzer et al,26 indicated that the group self-management program would improve behavioral outcomes, which can be attributed to the interaction with professionals and other influential individuals in diabetes self-management behaviors. Their results also demonstrated that diabetic patients with higher education levels and better perceptions of their disease would adopt more appropriate self-management behaviors. According to Olokoba et al,27 education of the populace is still key to the control of this emerging epidemic. A study performed by Afshar et al,28 revealed that group discussion is an effective method to achieve the treatment goals in adolescents with diabetes. Thus, group discussion, as a modern training strategy, could be useful in empowering patients with type 2 diabetes.
In a study conducted on Korean patients with diabetes undergoing self-management programs, Choi and Rush,29 reported a significant decrease in glycated hemoglobin test (HbA1C), waist circumference, and cholesterol level in the subjects after three months follow-up. However, in this study, there was no control group, and the results were obtained only from the pre- and post-test comparison of the variables.29 Different findings imply that it is impossible to design a self-management promotion program with unique content and structure, and program developers should design the programs for the intervention groups considering their cultural conditions and socioeconomic backgrounds.
On the other hand, the obtained results showed that the self-monitoring dimension of diabetes self-management acquired a low score. The self-monitoring behavior in patients with diabetes played a motivational and instrumental role in the perception of diabetes so that in such patients, lack of an appropriate scheduling program and lack of proper decision-making in the process of care and treatment are the main reasons for undesirable levels of diabetes control.30,31 Since regular control of blood sugar is difficult in the long term for many patients with diabetes, maintaining the motivation for blood sugar self-monitoring is a permanent problem in diabetic care.32
The effectiveness of the self-management program approach has led to the development of standard protocols, in accordance with social conditions, in order to be used in the health centers in some countries.33 Findings of the present study showed that self-management in patients with diabetes can be effective as a nursing intervention in health promotion. These findings can help researchers design diabetic self-management programs in accordance with the ground conditions of the society and, thereby, ensure promotion of its desirability and acceptability among the patients.
The present study was conducted in a diabetes clinic, which had some training programs for their patients, but there was a difference between these training programs and the self-management program. However, patients’ previously undergoing comprehensive training were not included in this study. We would recommend conducting a similar study on patients with diabetes along with a long-term follow-up to investigate the sustainability of the self-management interventions as well as a similar study with the participation of at least one active family member.
Another point is that this study did not assess the clinical outcomes related to diabetes, such as HbA1C and weight, since the duration of the study was not considered long enough to expect any significant effects for the intervention within the timescale. Our follow-up period was relatively short (three months), and further studies should examine the long-term effects of these interventions.
To avoid selection bias and ensure allocation concealment, the patients did not know at the time of registration whether they would be in the group discussion or serve as controls. Some patients dropped out after randomization to the intervention group, possibly wanting to participate in the study as a control only. Selection bias may be occurring here and future studies should address this.
Conclusion
The findings of the present research demonstrated that group discussion is an effective method for improving self-management in patients with diabetes. Furthermore, the use of a group discussion method can be an effective approach for holding active training sessions, improving self-management, and facilitating the learning process in real environments. We showed that the program could be presented by nurses in hospitals and outpatient centers, evidently indicating the society-oriented role of the nursing profession. Therefore, with regard to the ability, experience, and knowledge of nurses and abilities of clients, it is recommended to use this method in the self-management of the patients with type 2 diabetes.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
Acknowledgements
The authors wish to thank the cooperation and assistance of authorities in Urmia University of Medical Sciences. We especially thank the patients who participated in this study.
References
- 1. Hazavehei SM, Khani Jeihooni A, Hasanzadeh A, Amini S. The effect of educational program based on BASNEF model for eye care in non-insulin dependent diabetic patients. J Res Health Sci 2010 Dec;10(2):81-90.
- 2. International Diabetes Federation IDF DIABETES ATLAS 6th edition 2013. https://www.idf.org/e-library/epidemiology-research/diabetes-atlas.html.
- 3. Shirazi M, Anoosheh M, Rajab A. The effect of self care program education through group discussion method on knowledge and practice in diabetic adolescent girls referring to Iranian Diabetes Society. Iranian J Med Educ 2011;10(5):982-993.
- 4. Tol A, Majlessi F, Mohebbi B, Froshani AR. Communication between health workers and patients: An Effective Factor in Living With Diabetes. J hospital 2013;12(1):49-56.
- 5. Al-Mukhtar SB, Fadhil NN, Hanna BE. General and gender characteristics of type 2 diabetes mellitus among the younger and older age groups. Oman Med J 2012 Sep;27(5):375-382.
- 6. Al-Lawati JA. Diabetes mellitus: A local and global public health emergency! Oman Med J 2017 May;32(3):177-179.
- 7. Vergara N, Montoya JE, Luna HG, Amparo JR, Cristal-Luna G. Quality of life and nutritional status among cancer patients on chemotherapy. Oman Med J 2013 Jul;28(4):270-274.
- 8. van Puffelen AL, Rijken M, Heijmans MJ, Nijpels G, Rutten GE, Schellevis FG. Living with diabetes: a group-based self-management support programme for T2DM patients in the early phases of illness and their partners, study protocol of a randomised controlled trial. BMC Health Serv Res 2014 Apr;14(1):144.
- 9. Liu S, Bi A, Fu D, Fu H, Luo W, Ma X, et al. Effectiveness of using group visit model to support diabetes patient self-management in rural communities of Shanghai: a randomized controlled trial. BMC Public Health 2012 Dec;12(1):1043.
- 10. Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, et al; 2012 Standards Revision Task Force. National standards for diabetes self-management education and support. Diabetes Care 2013 Jan;36(Suppl 1):S100-S108.
- 11. Vaccaro JA, Feaster DJ, Lobar SL, Baum MK, Magnus M, Huffman FG. Medical advice and diabetes self-management reported by Mexican-American, Black- and White-non-Hispanic adults across the United States. BMC Public Health 2012 Mar;12:185.
- 12. Corl DE, McCliment S, Thompson RE, Suhr LD, Wisse BE. Efficacy of diabetes nurse expert team program to improve nursing confidence and expertise in caring for hospitalized patients with diabetes mellitus. J Nurses Prof Dev 2014 May-Jun;30(3):134-142.
- 13. Le Vine S, Polak J. Factors associated with young adults delaying and forgoing driving licenses: results from Britain. Traffic Inj Prev 2014;15(8):794-800.
- 14. Stone L. Reframing chaos–a qualitative study of GPs managing patients with medically unexplained symptoms. Aust Fam Physician 2013 Jul;42(7):501-502.
- 15. Spencer JE, Cooper HC, Milton B. The lived experiences of young people (13-16 years) with Type 1 diabetes mellitus and their parents–a qualitative phenomenological study. Diabet Med 2013 Jan;30(1):e17-e24.
- 16. Agborsangaya CB, Gee ME, Johnson ST, Dunbar P, Langlois MF, Leiter LA, et al. Determinants of lifestyle behavior in type 2 diabetes: results of the 2011 cross-sectional survey on living with chronic diseases in Canada. BMC Public Health 2013 May;13:451.
- 17. Daivadanam M, Absetz P, Sathish T, Thankappan KR, Fisher EB, Philip NE, et al. Lifestyle change in Kerala, India: needs assessment and planning for a community-based diabetes prevention trial. BMC Public Health 2013 Feb;13:95.
- 18. Rise MB, Pellerud A, Rygg LØ, Steinsbekk A. Making and maintaining lifestyle changes after participating in group based type 2 diabetes self-management educations: a qualitative study. PLoS One 2013 May;8(5):e64009.
- 19. Xiao L, Yank V, Wilson SR, Lavori PW, Ma J. Two-year weight-loss maintenance in primary care-based diabetes prevention program lifestyle interventions. Nutr Diabetes 2013 Jun;3(6):e76.
- 20. Nisari M, Zakir M, Rajab A, Faghih Zadeh S, Bassampor S, Rahmani M. Effect of nurse telephone follow-up on glucose and lipid control, in patients with type 2 diabetes. Iranian Journal of Diabetes and Lipid Disorders 2009;8(2):115-122.
- 21. Amiri SJ, Zabihi A, Babaieasl F, Eshkevari N, Bijani A. Self care behaviors in diabetic patients referring to diabetes clinics in Babol City, Iran. Journal of Babol University of Medical Sciences 2010;12(4):72-78.
- 22. White N, Manning ML, Brawer R, Plumb J. Using accreditation standards as a framework to evaluate and improve a community-based diabetes self-management education program. Popul Health Manag 2014 Feb;17(1):8- 12.
- 23. Lin CC, Anderson RM, Chang CS, Hagerty BM, Loveland-Cherry CJ. Development and testing of the diabetes self-management instrument: a confirmatory analysis. Res Nurs Health 2008 Aug;31(4):370-380.
- 24. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002 Oct;288(14):1775-1779.
- 25. Sieber WJ, Newsome A, Fiorella M, Mantila H. Translating patient self-management research into primary care: challenges and successes with group medical visits. Transl Behav Med 2012 Dec;2(4):535-542.
- 26. Kulzer B, Hermanns N, Gorges D, Schwarz P, Haak T. Prevention of diabetes self-management program (PREDIAS): effects on weight, metabolic risk factors, and behavioral outcomes. Diabetes Care 2009 Jul;32(7):1143-1146.
- 27. Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: a review of current trends. Oman Med J 2012 Jul;27(4):269-273.
- 28. Afshar M, Memarian R, Mohammadi E. The effect of group discussion on the quality of life and HbA1c levels of adolescents with diabetes. Iran Red Crescent Med J 2014 Aug;16(8):e21110.
- 29. Choi SE, Rush EB. Effect of a short-duration, culturally tailored, community-based diabetes self-management intervention for Korean immigrants: a pilot study. Diabetes Educ 2012 May-Jun;38(3):377-385.
- 30. Davidson MB. Daily self-monitoring unlikely to be cost-effective in adults with type 2 diabetes not using insulin in Canada. Evid Based Med 2010 Jun;15(3):75-76.
- 31. Clar C, Barnard K, Cummins E, Royle P, Waugh N; Aberdeen Health Technology Assessment Group. Self-monitoring of blood glucose in type 2 diabetes: systematic review. Health Technol Assess 2010 Mar;14(12):1-140.
- 32. Ali MK, Shah S, Tandon N. Review of electronic decision-support tools for diabetes care: a viable option for low- and middle-income countries? J Diabetes Sci Technol 2011 May;5(3):553-570.
- 33. Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, et al; 2012 Standards Revision Task Force. National standards for diabetes self-management education and support. Diabetes Care 2014 Jan;37(Suppl 1):S144-S153.