The two pelvic bones are united in the region of the pubic bone by a symphysial joint. Separation of this joint during delivery is a rare complication with an incidence reported between 1 in 300 and 1 in 30 000 pregnancies.1 With the enhanced accessibility of newer investigative modalities, the incidence seems to have increased and is likely to rise further in the future. We report two cases followed-up for one year and three months, respectively, followed by a review of the available literature with the aim of finding some insight into its associated factors, presentations, diagnosis, and management.
Case Report
Case one
A 22-year-old woman who conceived spontaneously after one year of marriage had an uneventful antenatal period, except that from the fifth month of pregnancy onwards, she started feeling pain in the region of the right buttock that radiated to the corresponding thigh. A fortnight later, she had similar pain on the other side as well.
She is 170 cm tall and had a prepregnancy body mass index of 21 kg/m2. She had been an avid athlete before pregnancy, and although she discontinued sports when she conceived, she continued to be physically active during her antenatal period.
She had spontaneous onset of labor at term, with the first stage of labor lasting seven hours and second stage spanning 30 minutes. Augmentation was done with pitocin infusion, which was started during the terminal part of the first stage. She delivered a healthy term neonate weighing 3.25 kg. During parturition, she felt as if something gave way in the region of the pubic bone anteriorly immediately before the birth of her baby.
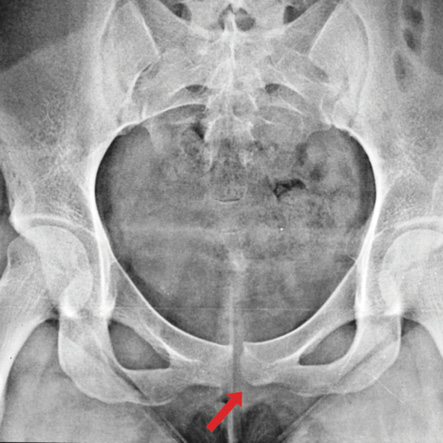
Figure 1: Posteroanterior radiograph of the pelvis of 22-year-old female shows abnormal widening of the pubic symphysis (arrow), measuring 15 mm in maximum transverse diameter. Both sacroiliac joints show no widening or fracture.
No epidural was given to her throughout labor. In the immediate postpartum period, she continued to experience pain in the pubic region particularly during movements, which caused obvious restriction of physical activity, such as turning to one side, and weight-bearing activities like walking and climbing stairs, but there was no incontinence of urine or feces. Anti-inflammatory and analgesic drugs were prescribed empirically during the subsequent days. When she continued to experience unbearable pain even a month after delivery, an orthopedic opinion was sought. Posteroanterior (PA) skiagram of the pelvis revealed a gap in the region of the pubic symphysis with the distance between the two bones of nearly 1.5 cm [Figure 1]. This was probably more initially since the skiagram was taken approximately a month postpartum. There was also a vertical displacement in the symphysis. A diagnosis of intrapartum pubic symphysis diastasis (PSD)was made, and the patient was given analgesics, anti-inflammatory drugs, and bed rest in lateral decubitus position. No pelvic binders or surgery were resorted to.

Figure 2: Posteroanterior radiograph of the pelvis shows symphysis pubis diastasis (arrow). Sacroiliac joint shows no fracture or widening.
On follow-up, she continued to take analgesics regularly for six months. Thereafter, she has been taking them occasionally. Despite being on regular physiotherapy since the time of diagnosis she is still unable to squat and rise from the ground > 12 months post delivery. However, she can now perform daily activities like walking and climbing stairs easily.
Case two
A gravida 4 para 2 (living 1, abortion 1) woman with rhesus negative blood type was referred to us for isoimmunization at 35 weeks gestation. Her middle cerebral artery peak systolic velocity was regularly monitored and she was induced with three doses of prostaglandin E2 at 37 weeks. After a prolonged labor, despite artificial rupture of membranes and pitocin augmentation, she delivered a healthy term female baby weighing 3.5 kg following a mediolateral episiotomy at 37+4 weeks. No Mc Roberts maneuver or epidural analgesia was offered to the patient at any time during her labor. Immediately post delivery, she was unable to walk, get up from her bed, turn from side-to-side or hold her child due to severe pain in the region of the pubic symphysis. A palpable, tender swelling was present in the same region. There was no associated incontinence. She delivered a baby weighing 4 kg in a previous pregnancy without any complications.
On abdominal examination, the patient had tenderness in the right iliac fossa. Vaginal examination revealed a tender right fornix.
On pelvis X-ray PA view, a gap in the region of pubic symphysis was visualized, suggesting the diagnosis of PSD [Figure 2]. On further investigation, magnetic resonance imaging (MRI) of the pelvis revealed an increased distance between the pubic rami measuring 16 mm in the midline with disruption of associated ligaments. It also showed a loculated, irregularly marginated collection in relation to the pubic symphysis extending anteriorly and posteroinferiorly communicating along the tract between the two pubic rami. The sacroiliac articulation, however, was unaffected [Figure 3a].
A fortnight later, the patient developed a soft tissue swelling in her vulva predominantly on the right side. It was tender, inflamed, and excruciatingly painful. The following day when her incision and drainage was planned under general anesthesia in liaison with team from orthopedics, the medial side of right labium majus developed a sinus draining copious amounts of pus. During incision and drainage of this abscess, the orthopedicians could not identify any communication of the sinus tract with the pubic symphysis. Thus, we concluded that this was an incidental development not directly related to the collection in the region of the diastasis. Review MRI confirmed the suspicion [Figure 3b].
At three-month follow-up, the patient was able to walk more than a few meters without help. Weight-bearing activity, turning from side-to-side, climbing stairs, and squatting were still not possible.
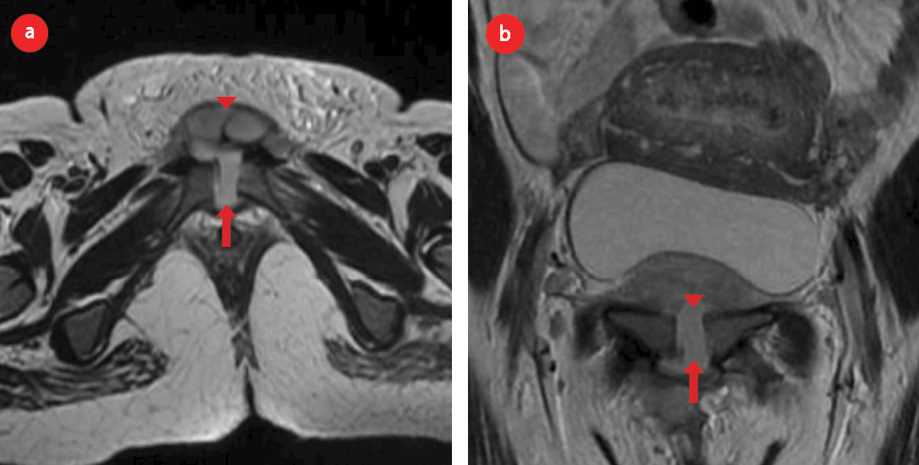
Figure 3: (a) Axial and (b) coronal T2-weighted magnetic resonance images confirms the X-ray finding in the same patient and shows wide separation of symphysis pubis (arrow). There was associated fluid collection and hematoma (arrowhead).
Discussion
PSD is a rarely encountered and often under-reported complication of pregnancy. This makes it difficult to elucidate the associated high-risk factors, symptom complex, and management algorithm.
The pubic symphysis is a secondary cartilaginous joint which under mechanical pressure and the influence of hormones progesterone and relaxin, relaxes by about 3–7 mm starting the first trimester of pregnancy.2 According to a study that assessed the dynamics of pubic symphysis during labor and postpartum, using ultrasonography, widening of symphysis took place in 59% to 94% parturients depending upon the exact site studied. The magnitude of widening varied from 9% to 139% of the original gap.3
Traditionally, as advocated by Hagen,4 a separation of more than 1 cm postpartum is said to be pathological and defines symphysial diastasis. However, several studies have demonstrated that there is no definite correlation between the magnitude of separation and severity of symptoms.4,5
In our first case, the lady was a primigravida with an athletic body and short span of labor. In the second case, she was a homemaker, thus relatively more sedentary and had a prolonged course of induction and labor. Neither woman had a history of epidural analgesia and shoulder dystocia or Mc Roberts maneuver associated with their case. The diverse histories led to a common pathway of diastasis and similar restriction of physical activity. Management was also conservative in both cases. Upon review of the literature, no factor was consistently associated with the occurrence of diastasis.
Cowling et al,6 reported a case of a primigravida with 5.4 cm separation intrapartum, with a loud crack audible just before delivery coupled with severe low back pain and difficulty in leg raising and hip flexion that was treated using a pelvic brace. Their case was associated with precipitate labor and Mc Roberts maneuver.6
In another report, history of macrosomia, prolonged second-stage of labor and epidural analgesia were associated with PSD.7 An association has also been seen with shoulder dystocia.8
In a report by Gräf et al,9 a multiparous patient who experienced shoulder dystocia managed by Mc Roberts maneuver and suprasymphysial pressure developed symphysial separation of 60 mm and was treated with open reduction and internal fixation with good clinical outcome.
Primiparity and multiple pregnancies were identified as risk factors in a study from South Korea.10 Henry reported postpartum diastasis of 24 mm in a primipara who had a history of active, athletic pursuit. They used chiropractic interventions such as transcutaneous electrical nerve stimulation, moist heat, and low force chiropractic adjustments of L4, L5, sacrum and innominate bones in addition to a sacroiliac belt.11
Many reports of operative management of diastasis including open reduction with internal fixation, external fixation, and local infiltration and stabilization of the posterior pelvic ring using minimally invasive surgery have been reported.12–14 Common indications for operative management include, traumatic rupture, failure of conservative therapy, or persistence or recurrence of symptoms after puerperium. Parker et al,13 suggest that surgical correction should be offered if the diastasis is more than 3 cm wide. One case report has also supported neuromodulation with spinal cord stimulator.15
We conclude that various high-risk factors such as primiparity, abnormally greater or less duration of labor, shoulder dystocia, Mc Roberts maneuver, and epidural anesthesia are associated with the phenomenon of PSD. The magnitude of separation, however, does not correlate well with severity of clinical features. Management of each case has to be individualized. However, conservative therapy offers resolution of symptoms in the majority of cases.
Not having a radiograph of the immediate postpartum period is both a weakness of the first case report and its strength, since it led to the second case being more promptly and thoroughly investigated. It serves to highlight the low index of suspicion for this entity among practitioners.
Conclusion
PSD is a rare complication of labor. It should be suspected in any patient who complains of something giving way during parturition followed by excruciating pain in the region of the pubic symphysis, particularly during weight-bearing activity. An abnormally long or short duration of labor, shoulder dystocia, Mc Roberts maneuver, and epidural anesthesia have been found to be associated with this complication as per the literature reviewed. History of active, athletic pursuit should be regarded as a high-risk factor for this pathology. MRI evaluation in addition to conventional radiography can add valuable clues to the diagnostic workup. This case series serves to make obstetricians and orthopedic surgeons consider this differential in a relatively low-risk population.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Snow RE, Neubert AG. Peripartum pubic symphysis separation: a case series and review of the literature. Obstet Gynecol Surv 1997 Jul;52(7):438-443.
- 2. Kharrazi FD, Rodgers WB, Kennedy JG, Lhowe DW. Parturition-induced pelvic dislocation: a report of four cases. J Orthop Trauma 1997 May;11(4):277-281,discussion 281-282.
- 3. Rustamova S, Predanic M, Sumersille M, Cohen WR. Changes in symphysis pubis width during labor. J Perinat Med 2009;37(4):370-373.
- 4. Hagen R. Pelvic girdle relaxation from an orthopaedic point of view. Acta Orthop Scand 1974;45(4):550-563.
- 5. Scriven MW, Jones DA, McKnight L. The importance of pubic pain following childbirth: a clinical and ultrasonographic study of diastasis of the pubic symphysis. J R Soc Med 1995 Jan;88(1):28-30.
- 6. Cowling PD, Rangan A. A case of postpartum pubic symphysis diastasis. Injury 2010 Jun;41(6):657-659.
- 7. Khorashadi L, Petscavage JM, Richardson ML. Postpartum symphysis pubis diastasis. Radiol Case Rep 2015 Nov;6(3):542.
- 8. Nitsche JF, Howell T. Peripartum pubic symphysis separation: a case report and review of the literature. Obstet Gynecol Surv 2011 Mar;66(3):153-158.
- 9. Gräf C, Sellei RM, Schrading S, Bauerschlag DO. Treatment of Parturition-Induced Rupture of Pubic Symphysis after Spontaneous Vaginal Delivery. Case Reports in Obstetrics and Gynecology;2014(2014):485916.
- 10. Yoo JJ, Ha Y-C, Lee Y-K, Hong JS, Kang B-J, Koo K-H. Incidence and risk factors of symptomatic peripartum diastasis of pubic symphysis. J Korean Med Sci 2014 Feb;29(2):281-286.
- 11. Henry L. Chiropractic management of postpartum pubic symphysis diastasis: A case report. J Can Chiropr Assoc 2015 Mar;59(1):30-36.
- 12. Najibi S, Tannast M, Klenck RE, Matta JM. Internal fixation of symphyseal disruption resulting from childbirth. J Orthop Trauma 2010 Dec;24(12):732-739.
- 13. Parker JM, Bhattacharjee M. Images in clinical medicine. Peripartum diastasis of the symphysis pubis. N Engl J Med 2009 Nov;361(19):1886.
- 14. Osterhoff G, Ossendorf C, Wanner GA, Simmen HP, Werner CM. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: technique and perioperative complications. Arch Orthop Trauma Surg 2011 Jun;131(6):809-813.
- 15. Idrees A. Management of chronic symphysis pubis pain following child birth with spinal cord stimulator. J Pak Med Assoc 2012 Jan;62(1):71-73.