A healthy 44-year-old woman presented to the Emergency Department at Sultan Qaboos University Hospital with a three-day-history of sore throat, difficulty swallowing, and neck stiffness. Her medical history was unremarkable. On examination, her vital signs were normal, and she was not in respiratory distress. Her pharynx was hyperemic and her neck was tender. She had restricted neck movements. Flexible nasopharyngoscopy revealed a swelling in the nasopharynx extending towards the oropharynx. Her remaining physical examination was unremarkable. Her white cell count was normal and C-reactive protein was 39. A contrast-enhanced computed tomography (CECT) scan and a magnetic resonance imaging (MRI) were performed. The findings of the CT and MRI scans are shown in Figure 1 and 2.
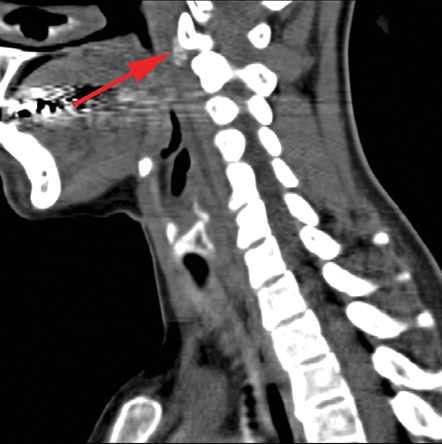
Figure 1: Sagittal contrast-enhanced computed tomography scan of neck.

Figure 2: Sagittal T2-weighted magnetic resonance imaging scan of the neck.
Questions
- What is the abnormality in the CECT scan as shown in Figure 1?
- What is the abnormality in the MRI scan as shown in Figure 2?
- What is your diagnosis?
- What is the treatment of choice?
Answers
- The sagittal CECT scan of the neck shows amorphous calcification of the longus colli muscle and a retropharyngeal effusion (red arrow).
- The sagittal T2-weighted MRI scan shows expansion of the retropharyngeal space with effusion (red arrow).
- Acute calcific tendinitis of the longus colli muscle.
- Non-steroidal anti-inflammatory drugs.
Discussion
Acute calcific tendinitis of the longus colli muscle is a rare self-limiting condition. Awareness of this condition is crucial, as it mimics other serious conditions like retropharyngeal abscess, cervical disc herniation, and meningitis. Early and appropriate diagnosis is vital to avoid unnecessary and potentially risky invasive procedures.
The longus colli muscle is one of the anterior cervical muscles, along with the longus capitis, rectus capitis anterior, and rectus capitis lateralis. Acute calcific tendinitis of the longus colli muscle is known by many names including prevertebral calcific tendinitis and retropharyngeal calcific tendinitis, and it remains an underdiagnosed disease.1 It was first described in a case report by Hartley in 1964.2
Symptoms develop acutely and patients often present to the emergency department with debilitating symptoms. Patients present with acute neck pain and stiffness, low-grade fever, odynophagia, and dysphagia.3 The neck may be tender on examination, with restricted movements. Most patients have a posterior pharyngeal wall swelling, as demonstrated in our patient.3 There may be a slight elevation in the white cell count and inflammatory markers.3
The most common cause of widening of the retropharyngeal space on imaging is retropharyngeal abscess.1 In this patient, although the retropharyngeal space was widened, with evidence of fluid collection, there was no peripheral rim enhancement as seen in an abscess. The calcification of the superior tendon of the longus coli, on CT scan (Figure 1, red arrow), confirms the diagnosis of calcific tendinitis.2 MRI scan reveals the effusion, as shown Figure 2 (red arrow), but is not the gold standard as the calcification may be missed.1
Calcific tendinitis occurs due to an inflammatory response to the deposition of calcium hydroxyapatite crystals in the tendons of the longus colli muscle.4 It is considered to be a part of the spectrum of calcium hydroxyapatite deposition disease (CHAD), which has been described in larger joints of the body.4
The management of this condition is conservative, as it is self-limiting. Administration of a potent non-steroidal anti-inflammatory drug is considered to be the mainstay of management.1–3 It is suggested that the treatment should be continued for two to three weeks.1 The use of muscle relaxants has also been advocated.1 A short course of steroids can provide rapid symptomatic relief.3 The use of narcotics is discouraged and patients are advised to avoid strenuous activities and neck movements that aggravate symptoms.3 A follow-up is recommended after one week, with further follow-up appointments in cases of patients with persistent symptoms.3 Symptoms usually improve after one to two weeks.5 Since this a self-limiting inflammatory condition, antibiotics are not necessary. Our patient improved dramatically within a few days of appropriate therapy and was discharged with no long term sequelae.
In conclusion, acute calcific tendinitis of the longus colli muscle is a self-limiting condition. Clinicians should be aware of this clinical entity as it often masquerades as a retropharyngeal abscess. CT scan will help clinch the diagnosis and avoid unnecessary use of antibiotics and potentially risky, invasive procedures.
Disclosure
The authors declared no conflict of interest.
references
- 1. Silva CF, Soffia PS, Pruzzo E. Acute prevertebral calcific tendinitis: a source of non-surgical acute cervical pain. Acta Radiol 2014 Feb;55(1):91-94.
- 2. Hartley J. Acute cervical pain associated with retropharyngeal calcium deposit: A case report. J Bone Joint Surg Am 1964 Dec;46(8):1753-1754.
- 3. Horowitz G, Ben-Ari O, Brenner A, Fliss DM, Wasserzug O. Incidence of retropharyngeal calcific tendinitis (longus colli tendinitis) in the general population. Otolaryngol Head Neck Surg 2013 Jun;148(6):955-958.
- 4. Chung T, Rebello R, Gooden EA. Retropharyngeal calcific tendinitis: Case report and review of literature. Emergency Radiology 2005 Nov;11(6): 375-380.
- 5. Southwell K, Hornibrook J, O’Neill-Kerr D. Acute longus colli calcific tendonitis causing neck pain and dysphagia. Otolaryngol Head Neck Surg 2008 Mar;138(3):405-406.