|
Abstract
Objectives: On June 6th 2007, a tropical Cyclone Gonu striked the coastline of Oman. The purpose of this study is to compare number of patients and pattern of illnesses between disaster (June 2007) and peace times (June 2006/2008).
Methods: Descriptive comparative analysis of all patients who visited primary health centers in Wilayat A’Seeb during the index days. Electronic database collected from the Health Centers (HC) were grouped into four groups; infection-related, trauma-related, acute non trauma-related, and miscellaneous group. Data were analyzed to find difference of patient influx and disease patterns between disaster and peace times.
Results: HC visits during the index days decreased from 9006 in 2006 to 8687 in 2007 then increased to 8786 in 2008. Neither between years variation nor between disaster and peace times difference was found to be statistically significant. The proportion of patient visited the HC due to infection-related illnesses changed from 30% in 2006, 31% in 2007, and 24% in 2008 (p<0.0001). The proportion of patients visited the HC due to trauma-related illnesses had changed from 4% in 2006, to 6.7% in 2007, and to 4.4% in 2008. (p<0.0001). Proportions for acute non trauma-related visits were 27% in 2006, 24% in 2007, and 23% in 2008 (p<0.0001). Miscellaneous group accounted for 38% in 2006, 37% in 2007, and 47% in 2008 (p<0.0001).
Conclusion: Tropical Cyclone Gonu caused statistically significant increase in percentages of infectious and trauma-related visits. The overall ratios of total visits did not differ from peace times.
Keywords: Natural disasters; Tropical cyclone; Oman; A’Seeb; Gonu; Pattern of illnesses.
Introduction
On June 1st 2007, a super cyclonic storm (hurricane) called Gonu developed in the Arabian Sea. On June 3rd, the storm rapidly intensified to attain peak winds of 240 km/h. Upon reaching the Omani coast on June 5th, it weakened into winds of 150 km/h, becoming the strongest tropical cyclone to hit the Arabian Peninsula.1
The Sultanate of Oman, located in the south east of the Arabian peninsula, consists of eight regions (Muscat, Batinah, Musandam, Dhahira, Dhofar, Dakhiliyah, Sharqiyah, and Wusta) and has more than 2000 km of coast line. Based on 2007 estimates, the total population of Oman was slightly more than 2.7 million and most of them live in the coastal area (mainly in Muscat and Batinah regions).2
Muscat, the capital of Oman, consists of six wilayats; city of Muscat, Mutrah, Bowshar, A’Seeb, Al Amerat, and Quriyat .It has a total population of 664,826 (2004 estimates), about one third of them live in wilayat A’Seeb.1
In Muscat and the coastal areas, flooding and mudflows from Gonu severely damaged local infrastructure, including bridges, roads, electricity, and telephone networks. Omanis and expatriates living in low-lying areas in the path of flood waters were most severely impacted by the storm. This disaster killed 49 people and caused 4 billion US$ worth of damage.3 However, the actual impact on the healthcare system was not well studied.
Disasters in general are uncommon events in Oman. In 1977, a storm hit the country taking 105 lives and injuring 5000 victims. In June 2010, tropical cyclone Phet occurred, which killed 24 persons and injured 10,000 others.4
Wilayat A’Seeb, because of its dense population and well-built health infrastructure, was chosen for this study to represent Muscat region. Around the world, primary care health centers (HC) play important role in maintaining and promoting good status of health during peace time. Following disasters, if not directly affected, HC should be the first to resume function to speed disaster recovery efforts.
Disaster research in Oman has attracted little attention to date. One newsletter, issued by the ministry of health (MOH) in Oman, summarized the actions taken by the ministry in response to national cyclone warning. MOH preparedness focused on making the hospitals in the cyclone path ready to receive major traumas and mass causalities. It also included providing the hospitals and health centers with generators, food, fuel, blood and pharmaceutical supplies.1 An article by Al-Shaqsi found deficiencies in the healthcare system in dealing with the tropical cyclone Gonu.4
Measuring the effect of this disaster on the healthcare system in Oman is important. Such process could give the policy makers valid statistical information, so appropriate preventive and corrective actions could be taken to face future incidents. For example, if post disaster surveillance showed an increase in the number of diarrheal diseases, then future disaster preparedness should include providing HC with more oral rehydration solutions and intravenous fluids supplies.
The primary objective of this study is to compare the number of patients who visited the primary HC in 2007 (disaster time) versus 2006/2008 (peace time). The secondary objective is to compare the pattern of illnesses among these patients.
Method
This study is a descriptive, comparative analysis of patients visited the primary care HC during disaster and peace times. The study population comprised of all patients seen at the primary care HC in A’Seeb area between June 1st to 15th in 2006, 2007, and 2008. Patients who visited the emergency departments were not included.
Wilayat Al Seeb occupies a narrow strip of coastline along the rim of the Gulf of Oman for a distance of 50 km/s. Its population is around 232,947 persons distributed among 24 villages and townships.5 It has six health centers equipped with primary care supplies including X-rays, labs, family medicine clinics, dental clinics, and pharmacies. Public health sector is the main source for healthcare services in Oman with some contribution from private clinics and hospitals.
The ICD (International Statistical Classification of Diseases and Related Health Problems) database of all patients visited the HC in the study area during the study period were reviewed and classified into 4 groups. Approval to conduct the study was obtained from the ethics committee in the directorate general of health services, government of Muscat (DGHSGM).
Data classification: ICD diagnosis from the electronic data base were classified into the following four groups:
Infection-related group included patients with fever, respiratory infections, diarrheal diseases, skin infections or infestations, measles, malaria, and other. These are group of illnesses that require vector control, control of oro-fecal or person to person spread, use of antimicrobials, or vaccination.
Trauma-related diseases include fractures, sprains, strains, lacerations, stings and bites, burns, poisoning, electrocutions, falls, car accidents, and drowning. These are group of diseases that require wound-care supplies, splints, and immobilization equipment.
Acute non-trauma disorders include acute medical or surgical conditions in addition to acute psychiatric, obstetric and gynecologic, ENT, dental, and ophthalmic diseases. These are diseases that require efficient strategies for treatment of daily emergencies.
Finally, the miscellaneous group includes diseases not included in the previous 3 groups (e.g. Follow-up for prescription refill, antenatal visits, and routine childhood care, and immunization).
Data were entered into spreadsheet using Microsoft Excel 2007, and then tested for the difference of patient influx between the 3 years as well as patient influx between disaster (2007) and peace (2006+2008) times. Similarly, the differences of disease patterns in each year and between disaster and peace times were tested.
The null hypothesis of this study stated there is no difference present in the patient influx nor in the disease patterns between disaster and peace times. For statistical analysis, we used chi-square test. Graph Pad software® (Graphpad.com) was used to calculate the p value. Differences were considered significant at the p=0.05 level.
Results
A total of 26,479 patients-visit encounter occurred between June 1st to 15th in 2006, 2007, and 2008. Assuming the total population (in A’Seeb area) remained constant at 232,947 throughout the study period, and each patient visited the health center one time only, approximately 3.8% the population visited the health center during peace and 3.7% during disaster time. Individual measures for each year are shown in Table 1 and for disease category in Table 2, while disease pattern among years are shown in Fig. 1.
Table 1: Total number of patients visited the health centers from June 1st to 15th in the three years.
|
Year
|
Total patients visited the HC
|
|
2006
|
9006
|
|
2007
|
8687
|
|
2008
|
8786
|
Table 2: Disease patterns during the three years.
|
Disease
|
2006
|
2007
|
2008
|
p-value
|
|
Infection
|
2730 (30.1%)
|
2733 (31.4%)
|
2182 (24.9%)
|
0.000001
|
|
Trauma
|
373 (4.3%)
|
583 (6.7%)
|
389 (4.5%)
|
0.000001
|
|
Acute non-trauma
|
2424 (27%)
|
2094 (24.2%)
|
2073 (23.2%)
|
0.000002
|
|
Misc.
|
3479 (38.6%)
|
3277 (37.7%)
|
4142 (47.2%)
|
0.000001
|
A total of 8687 encounters occurred in 2007 as compared to 9006 in 2006 and 8786 occurred in 2008 (p=0.0488). In comparison, the sum of 2006 and 2008 years (peace time) versus 2007 (disaster time) gave p value of 0.0697. In 2007, 2,733 (31%) infection-related visits occurred compared to 2730 (30%) in 2006 and 2,182 (24%) in 2008 (p<0.0001) Comparing infection-related visits between peace versus disaster time gave p<0.0001.
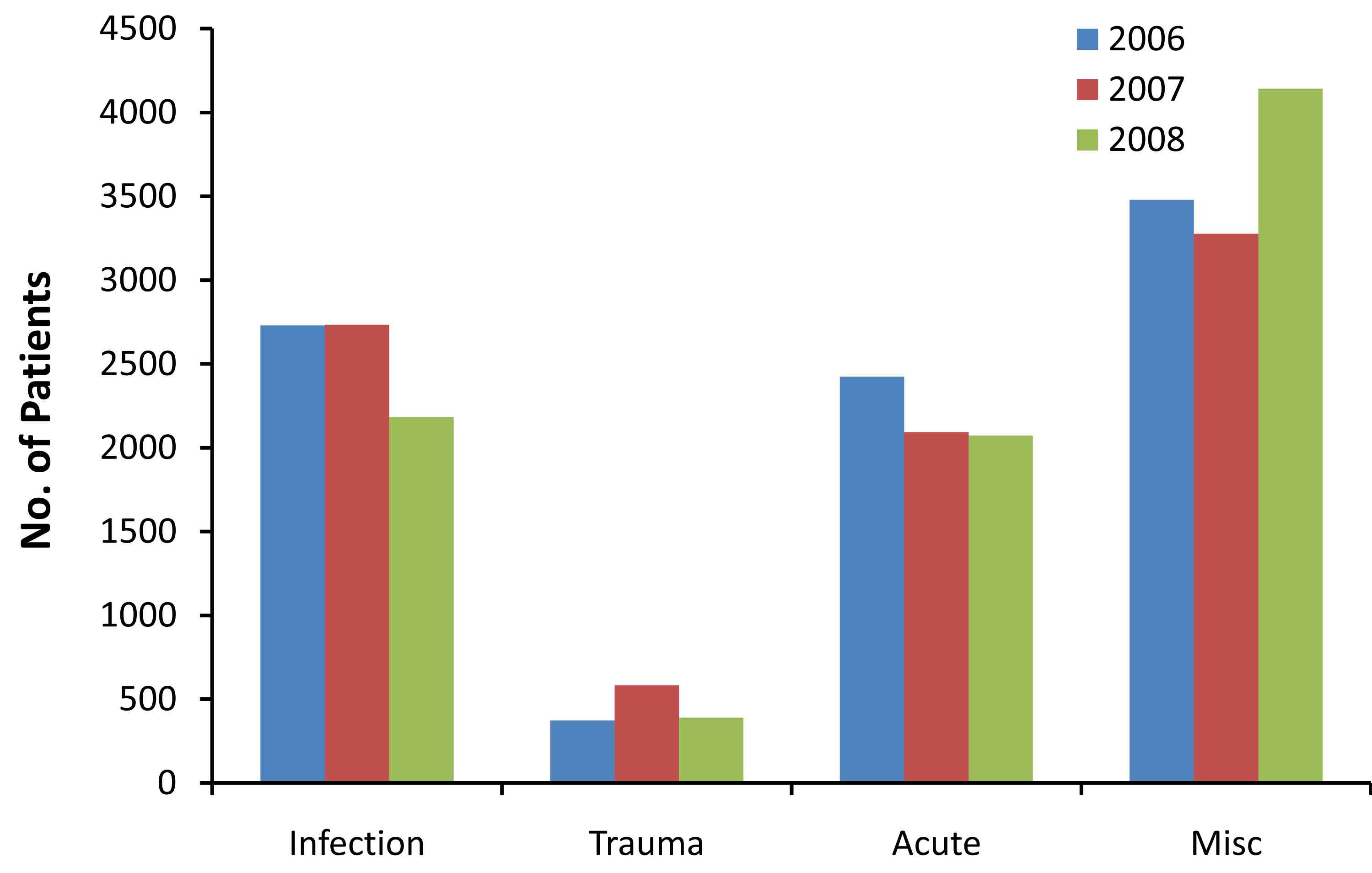
Figure 1: Disease pattern by year.
Among the infection-related visits, diarrheal diseases accounted for 2.2% of total visits in 2007, 1.6% in 2006, and 1.3% in 2008. Respiratory infections accounted for 18.5% of total visits in 2007, 19.7% in 2006, and 15% in 2008. A total of 583 (6.7%) trauma-related visits occurred in 2007 compared to 373 (4%) in 2006 and 389 (4.4%) in 2008 (p<0.0001). Comparing trauma-related visits between peace versus disaster time gave p<0.0001. Among trauma-related visits, lacerations accounted for 2.1% of total visits in 2007, 1.18% in 2006, and 0.7% in 2008. Musculoskeletal injuries accounted for 1.9% of total visits in 2007, 1.3% in 2006, and 1.29% in 2008.
Acute non-trauma related visits occurred 2094(24%) times in 2007 compared to 2424 (27%) in 2006 and 2073 (23%) in 2008 (p<0.0001). Comparing acute non-trauma visits between peace versus disaster time gave p value of 0.0732. Among acute non-trauma, medical disorders accounted to 18% of total visits in 2007, 16% in 2006, and 16.5% in 2008. Surgical disorders accounted for 1.3% of total visits in 2007, 1.4% in 2006, and 1.8% in 2008. Dental disorders accounted for 2% of the total visits in 2007, 4.8% in 2006, and 4.4% in 2008.
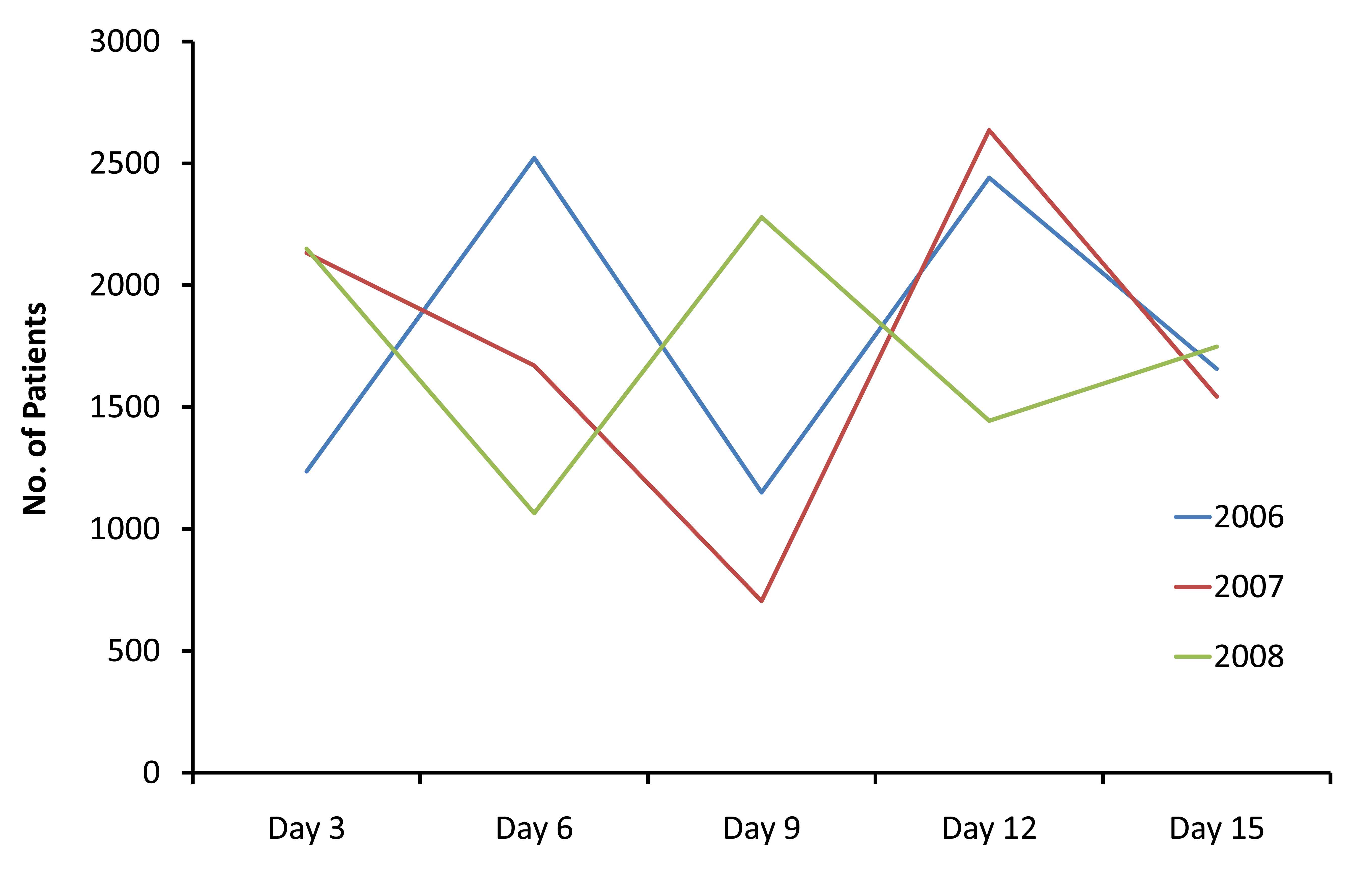
Figure 2: Number of patients visited the HC during the study period.
Table 3: Comparison of subtypes of disease patterns between years. Orthopedics injuries (fractures, sprains, contusions, and strains). Obstetrics: include all non-acute prenatal and postnatal visits. Soft misc. including visits for routine checkups, blood sampling, and post operative follow-ups.
|
Disease
|
2006
|
2007
|
2008
|
p value
|
|
Infections: (%)
|
|
|
|
|
|
Diarrhea
|
145(5.3)
|
196(7)
|
116(5.3)
|
.000001
|
|
Respiratory
|
1773(65)
|
1615(59)
|
1321(60.5)
|
.000001
|
|
Malaria
|
0
|
1
|
5
|
|
|
Others
|
812(29.7)
|
921(33.3)
|
740(34)
|
.000000
|
|
Trauma: (%)
|
|
|
|
|
|
Lacerations
|
107(28.6)
|
183(31.3)
|
63(16)
|
.000001
|
|
Orthopedics
|
117(31.3)
|
163(28)
|
114(29)
|
.000002
|
|
Others
|
149(40)
|
237(40.6)
|
212(54)
|
|
|
Acute non-trauma:(%)
|
|
|
|
|
|
Medical
|
1652(68)
|
1625(77.6)
|
1435(69)
|
.00003
|
|
Surgical
|
132(5.4)
|
115(5.5)
|
159(7.6)
|
.00002
|
|
Dental
|
437 (18)
|
179(8.5)
|
395(19)
|
.00000
|
|
Others
|
203(8.3)
|
175(8.3)
|
84(4)
|
.00004
|
|
Misc.:(%)
|
|
|
|
|
|
Vaccinations
|
135(3.8)
|
253(7.7)
|
380(9.1)
|
.000002
|
|
Obstetrics
|
283(8.1)
|
432(13)
|
624(15)
|
.000001
|
|
Child routine
|
181(5.2)
|
198(6)
|
176(4.2)
|
|
|
Soft misc.
|
1241(35)
|
1211(37)
|
1404(34)
|
.000005
|
|
Mental Health
|
30(0.8)
|
19(0.5)
|
16(0.4)
|
.000001
|
|
Others
|
1609(46)
|
1164(35.5)
|
1542(37)
|
.000001
|
A total of 3277 (37.7%) visits related to miscellaneous causes occurred in 2007 as compared to 3479 (38.6%) in 2006 and 4142 (47%) in 2008 (p<0.0001). Comparing miscellaneous-related visits between peace versus disaster time gave p<0.0001. Among the miscellaneous diseases, "soft" reasons (including general checkups, blood sampling, or adults with no acute clinical condition) accounted for 14% of total visits in 2007, 13.7% in 2006, and 16% in 2008. Non-acute obstetric visits accounted for 5% of total visits in 2007, 3% in 2006, and 7% in 2008. Routine child health visits accounted for 2.2% of the total visits in 2007, 2% in 2006 and 2008. Detailed comparison of disease subtypes between years is shown in Table 3. Comparison of daily census between years is shown in Fig. 2.
Discussion
Natural disasters may affect any part in the world. The number of victims is increasing due to increasing world population particularly in the poorer communities, and those living in areas prone for hurricanes, earthquakes, floods, and tsunamis. Very few disasters in the United States resulted in over 1000 deaths. However, the true magnitude of the disaster appears on the survivors.6
Disaster preparedness requires some background statistical information from prior similar events. Lack of such information had led to the misperception that natural disasters will lead to large number of injuries and outbreak of infections. Experience from flood-related disasters in the United States showed that most common discharge diagnosis from health facilities following disasters were mainly related to medication refill.4 This study showed similar frequency of patients visited health centers during disaster time and peace time. On average, 3.7% of the total population visited the HC during the study period. We may be able to show a significant difference if the study period was longer.
A statistically significant number of patients visited the health centers during disaster time due to infection-related illnesses. This was not reflected in the MOH registry as many patients in this study were having self-limited infections otherwise not reportable. Following hurricane Katrina, infections occurred in 7% of patients who visited the disaster health centers compared to 31% following Gonu.7 This larger difference between Gonu and Katrina studies could be attributed to the wide variety of diseases we included in this class. For example, we included patients with fever, diarrhea, and otitis media in the infection-related group.
Tropical Cyclone Gonu produced larger proportions of diarrheal diseases as compared to the peace time despite the overall rates did not exceed 2.2%. In comparison, a diarrheal disease was found in 7% of Katrina victims. On the other hand, Gonu produced smaller frequency of respiratory infections (59%) as compared to peace times (63%). This finding was similar to the reports following Katrina.7
Gonu produced significantly higher frequencies of trauma-related visits compared to peace time (6.7% vs. 4.2%). In comparison, 18% of patient encounter following Katrina were related to trauma.7 The lower rate of injuries in Gonu study is probably due to A’Seeb area was not affected by the strong cyclone winds. Figures could be much worse if this study was conducted in areas like Sur or Qurayat (both were heavily affected by the rainfalls and strong winds).
Lacerations accounted for about one third of the trauma group during Gonu time. In comparison, studies done following tropical cyclones elsewhere found that lacerations caused about 80% of the injuries.8
Acute non-trauma conditions accounted for one quarter of the cases during Gonu time. This was found to be statistically not significant when compared to peace times. Subtype analysis of the acute non-trauma category found that medical disorders occurred more frequently during disaster time (77% vs. 68% during peace time). This could be attributed to many factors, namely; patients visiting the HC before the disaster day for medications refill, sudden shortage of medical care during disaster had led to relapse of patients with chronic diseases, and population displacement with subsequent medication loss. On the other hand, surgical and dental conditions did not increase during the disaster.
About 37% of patients during Gonu period had visited the HC for miscellaneous reasons. This was found to be statistically significant when compared to peace times. A similar percentage was obtained from the study on Katrina victims.7
Miscellaneous diseases accounted for the highest numbers of patients visiting health centers during both peace and disaster times. This is due to wide variety of diseases included in this group. In addition, medication refills in the country occur mainly in the primary HC. Subtype analysis of the miscellaneous group found that higher percentages of visits during disaster time were related to vaccinations, routine child care, and soft reasons. Soft reasons include patient visiting the HC for employment check-ups, routine adult check-up, blood sampling, or post-operative follow-ups. Tropical cyclone Gonu did not cause an increase in mental health disorders or routine obstetric visits.
Opposite to what was seen from studies done elsewhere, the percentage of patients who visited the HC during disaster time did not differ from what was seen during peace time. This could be due to some of these HC were closed during the disaster. As illustrated in Fig. 2, a significant dip in the 2007 line was seen from June 6th to 9th. In fact, this was due to four of the HC being closed during these days.
One of the limitations of this study is that the exact population for A’Seeb area was unknown for the years of 2006, 2007, and 2008. Therefore, we used the 2004 estimates as the number of the total population. In addition, immediately before the disaster, unknown number of families moved into the area from other regions in the cyclone path seeking better shelter. Similarly, following the disaster unknown number of families left the area into other regions. For this reason the 2004 estimate was kept constant at 232,947 throughout peace and disaster times.
Disasters are low probability, high impact events.6 As such, disaster planning and preparedness takes lower priority in funding in lieu of other projects. In addition, disasters are considered as high demand low resource events. The following are suggestions for management of future natural disaster incidents:
1- Overall function of the primary HC
a- Creation of fast tract clinics in the primary HC to treat patients with minor injuries (like simple lacerations), these clinics could be staffed with trained nurses, and medical students with supervision of medical staff.
b- Patients with more than simple injuries should be seen by a medical staff as soon as possible. Patients with emergencies (like major trauma, cardiac, respiratory, or obstetric emergencies) should be seen by the most experienced medical staff immediately to initiate treatment and arrange transport to nearby emergency departments.
c-Restrict use of laboratory investigation and X-rays for essential tests only.
2- Shortage of staff
Many regular staff working in the primary HC are not local residents of A’Seeb area. When disasters occur, many roads get blocked and the HC become inaccessible due to surrounding flood water. To overcome this, each HC should have regularly updated list of medical/nursing/and allied health staff from all other health institutes who live in the immediate vicinity to the HC. Thus, when shortage of staff occurs during disasters, replacement can be summoned from this list using TV, radio, or regular phones.
3- Maintaining operational status and free access to the HC
During cyclone Gonu, four out of the six HC in the study areas were temporary closed for about 3-4 days due to flooding. Mitigation efforts to face future incidents should include better building codes, flood ways, installation of flood barriers, and storage of disaster and pharmaceutical supplies 1-2 feet above the floor.
In addition, disaster preparedness should provide health centers with dual emergency power supply; fuel generators and solar energy-batteries. Providing the HC with water storage containers and sanitary supplies is important so the center will be self-sufficient for 24 hrs. should the main supply get lost.
When disasters occur, regular phones, GSM, and internet services may get damaged. Communications between disaster agencies and between health facilities should rely on radios, satellite phones, and other unconventional methods. Telephone operators and administrators in each of the HC should be trained to use this equipment ahead of time prior to the disaster. Radio signals may get jammed due to overuse. We suggest that communication from the HC should only be to the MOH headquarters using pre-written script and for specific indications. These include request for patient transfer into hospital, request for water and pharmaceutical supplies, summon more staff, or evacuation.
4- Loss of computer services and electronic data
Disaster plans may include procedures to switch into paper patient records should the computer systems fail. Also, each patient with chronic diseases should have weatherproof card containing updated list of current medications and allergies.
5- Welfare of staff at work
Disaster plans should put some attention to the personnel working during disasters. During the tropical cyclone Gonu, many doctors and nurses were traumatized as they were cut-off from their families and were stranded in hospitals. In addition, there were inadequate supplies of food and water for the staff themselves.4 Some of the staff worked continuously for 24 hours in the 2 working HC during the disaster day. Table 4 include list of suggestion for welfare of the working staff.
6- Mobile medical units
During Gonu, some schools in the area were used as temporary shelter for displaced population. Creation of mobile units and opening "shelter clinic" is important to provide health support for the displaced victims without adding additional burden on the local HC.
7- Treatment strategies of specific diseases
Lacerations
- Stockpiling of disposable wound care supplies.
- Use of stables instead of stitches for wound closure.
- Update of tetanus immunization status.
- Considering all wounds are contaminated. So, should be treated as such with prescription of antibiotics and delayed closure if possible.
- All wound should be re-checked in 48 hrs. to ensure no complications.
- Delayed referral for definite tendon repair until situation improves and specialist clinics resume function.
Orthopedics
This includes sprains/strains/and simple fractures.
- Stockpile of various sizes of splints and casting materials.
- Pamphlets containing cast care instructions.
- Advise to return for reassessment in 72 hours
Diarrheal diseases
Patients with isolated gastroenteritis should be triaged and treated according to the severity of their illness. Children with gastroenteritis (if mild or moderate dehydration) could be discharged home if tolerating oral rehydration solution. If not, a single dose of oral Ondansetron (0.1 mg/kg to max 4 mg) should be given. If still not tolerating oral rehydration, start IV hydration and arrange transport to the hospital. All children with severe dehydration should have IV hydration and arranged for prompt transfer to the hospital.
Adults with gastroenteritis could be discharged home if tolerating oral hydration and have normal vital signs. Others not tolerating oral hydration could be given intramuscular antiemetic and have few hours observation to receive intravenous or oral hydration.
Table 4: Staff welfare problems and solutions.
|
Problem
|
Solution
|
|
Insufficient sleep
|
Setting a maximum work shift duration
|
|
Fatigue
|
Scheduled rest breaks throughout a work shift.
|
|
Fatigue
|
Monitoring for fatigue signs
|
|
Limited access to nutrition needs
|
Specific rest and food areas for the staff
|
|
Lack of water for toilets
|
Disposable sanitary supplies
|
|
Lack of security
|
Provide security during working hours
|
|
Lack of contact with the family
|
Assign specific phone for staff use only
|
|
Lack of contact with the family
|
Encourage family visit during breaks
|
|
Lack of transport
|
Coordinate with civil defense/Armed forces
|
Use of antibiotics should be restricted to high risk patients. These include those with HIV, chemotherapy, diabetics, neonates, young infants or organ transplant patients. The World Health Organization currently recommends empiric antimicrobial therapy in the setting of febrile acute bloody diarrhea in young children.9 All discharged pediatric patients should be reviewed in 24 hrs. by an MD to assess hydration status or development of complications. When weather conditions permit, tents could be built in the health center’s backyard to be used as an observation unit.
Conclusion
Tropical Cyclone Gonu caused significant increase in percentages of infection and trauma-related visits. Based on this, HC disaster plans need some adjustments to face future incidents. A future study with similar design in the nearby emergency departments (ED) is needed to determine whether the disaster caused an increase in ED visits or change in disease patterns.
Acknowledgements
This study would not have been possible without the support from the planning director at the directorate general of health services, governate of Muscat Dr. Qamra Al-Sariri, Dr. Alzamani M. Idrose, from the emergency department, hospital of Kuala Lambur, Malaysia, and Mr. Mustafa Salamah, from the University of Manitoba.
|