Setting research priorities is critical for ensuring that healthcare resources are allocated efficiently to areas with the most significant potential to improve health outcomes. The growing complexity of healthcare challenges and constraints to research funding necessitates a structured approach to prioritize research. Systematic methods emphasize evidence-based criteria, transparency, and active stakeholder engagement to ensure research aligns with health system needs.1–3 Key criteria-such as disease burden, potential health impact, and feasibility-help guide research toward areas with the greatest benefit.4
Despite these metrics, no universally accepted method for setting research priorities exists. The absence of standardization has led to inconsistent processes, often relying on subjective judgment, which may fail to address key health system needs adequately. Additionally, the limited integration of real-world data, such as electronic health records (EHR), into research prioritization frameworks reduces the applicability of findings to actual clinical and operational challenges.5 Empirical studies suggest that context-specific adaptations and flexible, responsive approaches are necessary to address these limitations.2 Effective stakeholder engagement—involving patients, healthcare providers, policymakers, and researchers—is also a critical factor for success.3
A further challenge lies in the disconnect between academic research agendas and the priorities of healthcare service institutions. While medical research often focuses on theoretical inquiries and academic impact, healthcare service institutions prioritize practical applications to patient care and system performance.6 This misalignment can result in research that lacks direct relevance to real-world practice, creating a gap between knowledge generation and implementation. Bridging this gap requires aligning research agendas with healthcare providers’ needs, ensuring that research is both innovative and directly relevant to improving healthcare outcomes and operational efficiency.
Globally, research agendas are developed to enhance healthcare delivery and address systemic inefficiencies. High-income countries prioritize health systems research to improve equitable and effective resource allocation.7 In the Middle East, efforts focus on addressing region-specific challenges such as non-communicable diseases (NCDs), health system performance, and population health.8 In Oman, research prioritization aims to maximize impact by directing funding toward strategically significant areas, considering factors such as disease burden, population-specific health needs, and societal impact.9,10 Oman’s Health Vision 2050 for Health Research seeks to position Oman as a regional leader by setting clear priorities, strengthening research capacity, producing high-quality research, and translating findings into policy.11
Our study aims to bridge the gap between academic research and healthcare service priorities by identifying clinical and health service research needs for the Royal Hospital, a tertiary care facility in Muscat, Oman. This novel approach integrates real-world EHR data with stakeholder engagement, balancing immediate clinical needs with strategic health system objectives. This approach provides a roadmap for research funding and initiatives that support patients, clinicians, and policymakers, contributing to a more efficient and equitable healthcare system.
Methods
Our study was conducted at the Royal Hospital, a tertiary healthcare facility and a leading referral center in Oman operating independently under the Ministry of Health. The hospital offers a comprehensive range of services, including internal medicine, pediatrics, surgery, obstetrics and gynecology, as well as specialized centers in genetics, oncology, cardiology, endocrinology, diabetes, and hyperbaric medicine. It is equipped with advanced diagnostic and therapeutic technologies, three intensive care units, and three emergency departments (adult, pediatric, and obstetric/gynecology). Paramedical services, such as physiotherapy and nutrition, are also provided.
A multi-step approach was used to establish a comprehensive list of research priorities at the Royal Hospital, integrating retrospective EHR analysis with stakeholder consultations. This method combined historical data and expert input to ensure robust, data-driven outcomes.
Inpatient EHR data from 2010 to 2023 were extracted and analyzed to identify clinical priorities based on diagnostic trends and mortality outcomes. The dataset included diagnostic information and discharge outcomes. Data cleaning involved removing duplicates and outliers to ensure accuracy. The analysis highlighted emerging health issues and areas of increasing demand, forming a preliminary list of potential clinical research priorities.
Leading causes of hospitalization were grouped using primary International Classification of Diseases, 10th Revision (ICD-10) category codes, to calculate the percentage representation of each category, with those accounting for < 2% grouped under ‘others’. The most prevalent ICD-10 codes within each category were also identified, along with their respective percentages, to determine the five most common specific diagnoses each year. Mortality trends were examined by identifying the most frequent diagnoses associated with death. Data were initially received in an Excel spreadsheet before being transferred to the R program for analysis.
Findings from the EHR analysis were validated through discussions with 10 key stakeholders, including quality department members and the hospital’s strategy committee. Stakeholders were selected for their knowledge of system challenges and their roles in quality improvement, strategic planning, research, and operational oversight. Semi-structured interviews ensured alignment between identified priorities and day-to-day clinical challenges. All departments reviewed the EHR findings to verify consistency with other hospital data sources. In addition, the clinical priorities were presented to the hospital’s director general and deputies to ensure congruity at all organizational levels.
To determine health system priorities, key domains were developed by integrating the hospital’s strategic goals, the health system’s building blocks, and the Institute of Medicine’s 1995 framework, ensuring relevance at the hospital’s operational level.12,13 These domains were introduced during a seminar with department directors and hospital administrators, with practical examples provided for clarity. Directors then facilitated brainstorming sessions within their departments, engaging researchers and decision-makers to identify specific research needs. A structured template, validated through expert review, was used to systematically collect input during this process.
Subsequently, individual unstructured interviews were conducted with the hospital’s quality director and strategy committee chairperson to refine and expand the identified priorities. This iterative process ensured that research priorities reflected both immediate clinical challenges and broader mortality and morbidity trends. The final list of priorities was reviewed by department directors to confirm accuracy and resolve of any remaining concerns.
A two-round Delphi method was employed to refine and validate the research priorities, involving 10 key decision-makers and subject matter experts. Participants included three senior researchers, the hospital’s strategy chairperson, the heads of the quality department and performance improvement unit, the hospital’s director general and deputies, and two experts from the Ministry of Health specializing in healthcare policy, clinical practice, and operational management.
The main ICD categories, the top three conditions under each, and a compiled list of 30 health service priorities were shared during the first round of the Delphi process.
In the first round, participants completed an online survey in which they rated each preliminary research priority on a 5-point Likert scale ranging from 1 (irrelevant) to 5 (highly relevant). They also provided open-ended feedback on feasibility, completeness, prioritization, and overall alignment (Appendix 1). To ensure content validity, the questionnaire underwent expert review.
In the second round, a revised list incorporating feedback from the first round was shared with participants for re-evaluation. Consensus was defined as ≥ 80% agreement on a rating of 4–5. Any divergent views were addressed through face-to-face interviews involving the research team and the hospital’s strategy committee chairperson.
The study was approved by the Royal Hospital’s Scientific Research Committee (#MOH/CSR/21/24494) and adhered to ethical standards, including the Declaration of Helsinki and institutional policies. All EMR data were anonymized to protect patient confidentiality, and no identifiable patient information was included in the study.
Results
The EHR analysis examined 652 567 admissions from January 2010 to December 2023. The top 10 most frequent ICD-10 codes highlighted key clinical priorities [Table 1]. Among these, pregnancy and childbirth-related conditions accounted for 25.0% of cases, with spontaneous vertex delivery and perineal laceration being the most common. Circulatory system diseases represented 10.4%, with atherosclerotic heart disease as the leading diagnosis. Neoplasms constituted 8.6% of all diagnoses, with breast cancer being the most prevalent within this category (22.6%). Diseases of the genitourinary system accounted for 7.3%. Mortality was recorded in 1.8% of admitted cases, with the most common underlying causes including septicemia, pneumonia, cardiogenic shock, myocardial infarction, and respiratory failure.
Table 1: Distribution of main International Classification of Diseases, 10th Revision (ICD-10) categories and subcategories by percentage.
|
1. Pregnancy, childbirth, and the puerperium (O00–O99) (25.0%)
|
O80.0: Spontaneous vertex delivery (27.0%)
O70.9: Perineal laceration during delivery, unspecified (15.6%)
O70.0: First-degree perineal laceration during delivery (10.2%)
|
|
2. Diseases of the circulatory system (I00–I99) (10.4%)
|
I25.1: Atherosclerotic heart disease (34.0%)
I50.9: Heart failure, unspecified (5.1%)
I21.9: Acute myocardial infarction, unspecified (4.0%)
|
|
3. Neoplasms (C00–D48) (8.6%)
|
C50.9: Breast, unspecified (22.6%)
C18.9: Colon, unspecified (6.9%)
C67.9: Bladder, unspecified (4.3%)
|
|
4. Diseases of the genitourinary system (N00–N99) (7.3%)
|
N39.0: Urinary tract infection, site not specified (11.0%)
N18.0: Chronic kidney disease (10.0%)
N20.0: Calculus of kidney (8.2%)
|
|
5. Diseases of the digestive system (K00–K93) (6.5%)
|
K35.9: Acute appendicitis (15.7%)
K40.9: Unilateral or unspecified inguinal hernia, without obstruction or gangrene (8.25%)
K80.2: Calculus of gallbladder without cholecystitis (4.9%)
|
|
6. Diseases of the respiratory system (J00–J99) (4.4%)
|
J18.9: Pneumonia, unspecified (17%)
J21.9: Acute bronchiolitis, unspecified (11.9%)
J45.9: Asthma, unspecified (9.2%)
|
|
7. Diseases of the blood, blood-forming organs, and certain disorders involving the immune mechanism (D50–D89) (4.3%)
|
D57.0: Sickle-cell anemia with crisis (39.9%)
D56.1: Beta thalassemia (15.0%)
D50.9: Iron deficiency anemia, unspecified (9.0%)
|
|
8. Congenital malformations, deformations, and chromosomal abnormalities (Q00–Q99) (3.7%)
|
Q53.1: Undescended testicle, unilateral (9.3%)
Q21.1: Congenital malformations of cardiac septa (6.8%)
Q21.0: Congenital malformations of cardiac septa (6.7%)
|
|
9. Endocrine, nutritional, and metabolic diseases (E00–E90) (3.3%)
|
E10.1: Diabetes mellitus with ketoacidosis (7.2%)
E87.1: Hypo-osmolality and hyponatremia (6.8%)
E30.1: Precocious puberty (5.2%)
|
|
10. Certain conditions originating in the perinatal period (P00–P96) (2.7%)
|
P59.9: Neonatal jaundice, unspecified (25.6%)
P07.1: Disorders related to short gestation and low birth weight, not elsewhere classified (11.3%)
P22.1: Transient tachypnoea of newborn (6.5%)
|
|
11. Certain infectious and parasitic diseases (A00–B99) (2.0%)
|
A09: Other gastroenteritis and colitis of infectious and unspecified origin (40.0%)
A41.9: Sepsis, unspecified (10.8%)
|
Specific ICD-10 codes were examined each year to identify recurring and emerging conditions, excluding pregnancy and childbirth-related cases [Table 2]. Cardiovascular diseases, particularly atherosclerotic heart disease, were consistently reported annually. Genetic disorders, such as sickle-cell anemia, appeared regularly, while beta-thalassemia emerged from 2022 onwards. Oncology-related conditions, including breast cancer, showed increasing prevalence, particularly in 2023, while colorectal cancer was noted in 2022 and 2023. Respiratory and infectious diseases, including pneumonia and acute bronchiolitis, remained common, as did acute appendicitis and urinary tract infections. Emerging conditions, including iron deficiency anemia and sleep apnea, were observed in later years. Chronic conditions such as heart failure and kidney disease also showed a steady presence in recent years.
Table 2: Yearly trends in prevalence of top disease International Classification of Diseases, 10th Revision.
|
1
|
D57.0 (564)
|
I25.1 (531)
|
I25.1 (751)
|
I25.1 (1035)
|
I25.1 (1210)
|
I25.1 (1853)
|
I25.1 (1683)
|
I25.1 (2148)
|
I25.1 (2148)
|
I25.1 (2569)
|
I25.1 (2229)
|
C50.9 (3068)
|
C50.9 (3197)
|
C50.9 (3197)
|
|
2
|
I25.1 (458)
|
K35.9 (495)
|
K35.9 (507)
|
D57.0 (486)
|
D57.0 (497)
|
D57.0 (477)
|
D57.0 (1237)
|
D57.0 (1595)
|
D57.0 (1535)
|
D57.0 (1793)
|
D57.0 (1106)
|
I25.1 (2084)
|
I25.1 (1271)
|
D56.1 (1229)
|
|
3
|
K35.9 (453)
|
D57.0 (495)
|
D57.0 (509)
|
K35.9 (480)
|
D57.0 (522)
|
K35.9 (479)
|
N39.0 (572)
|
N39.0 (586)
|
J18.9 (590)
|
J18.9 (591)
|
D57.0 (851)
|
D57.0 (1295)
|
D57.0 (1103)
|
D57.0 (1138)
|
|
4
|
K40.9 (363)
|
K40.9 (316)
|
K40.9 (383)
|
N39.0 (281)
|
K40.9 (332)
|
N39.0 (462)
|
K35.9 (481)
|
K35.9 (485)
|
K35.9 (486)
|
K35.9 (499)
|
K35.9 (393)
|
K35.9 (481)
|
K35.9 (498)
|
K35.9 (495)
|
|
5
|
I20.9 (284)
|
N39.0 (277)
|
N39.0 (269)
|
K40.9 (263)
|
N39.0 (283)
|
A09 (416)
|
C50.9 (491)
|
J18.9 (409)
|
J18.9 (439)
|
N39.0 (559)
|
N18.9 (502)
|
N18.0 (1064)
|
C18.9 (891)
|
C18.9 (869)
|
|
6
|
A09 (237)
|
J18.9 (261)
|
I21.9 (321)
|
A09 (257)
|
A09 (280)
|
A09 (463)
|
J21.9 (375)
|
J21.9 (441)
|
J21.9 (441)
|
J21.9 (490)
|
A09 (397)
|
A09 (976)
|
N18.0 (949)
|
D50.9 (692)
|
|
7
|
N40 (208)
|
J18.9 (224)
|
J18.9 (300)
|
N40 (250)
|
N40 (283)
|
N40 (284)
|
I21.9 (375)
|
I21.9 (471)
|
I21.9 (485)
|
A09 (429)
|
A09 (325)
|
D57.0 (666)
|
D57.0 (644)
|
D57.0 (644)
|
|
8
|
T82.4 (207)
|
T82.4 (222)
|
T82.4 (258)
|
T82.4 (263)
|
N18.9 (332)
|
J18.9 (328)
|
J18.9 (392)
|
J45.9 (403)
|
J45.9 (441)
|
J45.9 (429)
|
J45.9 (361)
|
J18.9 (593)
|
J18.9 (573)
|
J18.9 (573)
|
|
9
|
J18.9 (202)
|
N20.0 (227)
|
A09 (203)
|
J21.9 (213)
|
A09 (284)
|
N18.0 (332)
|
I50.9 (390)
|
J21.9 (346)
|
J45.9 (355)
|
J45.9 (333)
|
C73 (234)
|
I50.9 (528)
|
I50.9 (558)
|
I50.9 (558)
|
A09 : infectious gastroenteritis and colitis, unspecified; C18.9: malignant neoplasm of colon, unspecified; C50.9: malignant neoplasm of breast, unspecified; D50.9: iron deficiency anemia, unspecified; D56.1: beta thalassemia; D57.0: sickle-cell anemia (with crisis); G47.3: sleep apnea, unspecified; I25.1: atherosclerotic heart disease of native coronary artery; I50.9: heart failure, unspecified; J18.9: pneumonia, unspecified organism; J45.9: asthma, unspecified; K35.9: acute appendicitis, unspecified; N18.0: end-stage renal disease; N20.0/N20.1: calculus of kidney/ureter; N39.0: urinary tract infection, site not specified; T82.4: mechanical complication of vascular grafts.
Research priorities identified through stakeholder consultations were categorized into five key domains based on the hospital’s strategic goals, the health system’s building blocks, and the Institute of Medicine’s 1995 framework: patient-centered care, access to care and integrated care, innovation and research, operational excellence and sustainability, and healthcare workforce development and engagement [Figure 1].
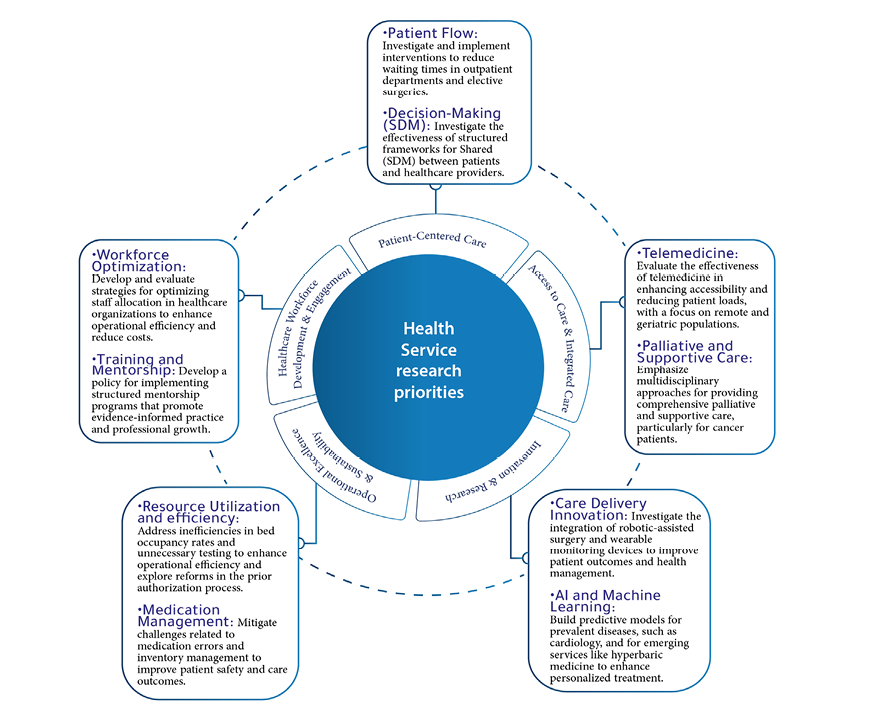 Figure 1: Themes and topics identified as health service priorities.
Figure 1: Themes and topics identified as health service priorities.
Within the patient-centered care, priorities included improving patient flow by reducing waiting times in outpatient departments and elective surgeries, alongside implementing structured frameworks for shared decision-making between patients and healthcare providers. The access to care and integrated care domain emphasized evaluating the effectiveness of telemedicine in improving accessibility, especially for remote and geriatric populations, and adopting multidisciplinary approaches to palliative and supportive cancer care. Under operational excellence and sustainability, key priorities included optimizing bed occupancy rates, minimizing unnecessary testing, reducing medication errors, and managing inventory to improve patient safety.
The innovation and research domain prioritized investigating robotic-assisted surgery and wearable monitoring devices, as well as developing predictive models using artificial intelligence (AI) and machine learning for prevalent diseases such as cardiovascular conditions and emerging services such as hyperbaric medicine.
Lastly, healthcare workforce development and engagement focused on optimizing staff allocation to enhance operational efficiency and reduce costs, and on implementing structured mentorship programs to foster evidence-based practice and professional growth. The final list of priorities was validated through two Delphi rounds and refined following a final workshop with key stakeholders.
Participants evaluated the clinical and health service research priorities using a 5-point Likert scale. Overall, 80% of respondents rated the priorities as relevant (scores ≥ 4). However, feedback highlighted two key areas for improvement: the need to broaden the inclusion of preventive measures for NCDs and to integrate patient experience metrics for a more patient-centered approach. These recommendations were incorporated before proceeding to the second round.
In the second round, nine respondents reassessed the revised priorities. All priorities received ratings of 4 or 5, confirming a strong consensus that the final priorities were aligned with the hospital’s strategic objectives and national healthcare goals. While relevance was widely acknowledged, feasibility concerns emerged, particularly regarding information technology infrastructure, financial constraints, and workforce capacity. Resource allocation was emphasized, especially for research focusing on high-burden conditions.
Participants agreed on the comprehensiveness of the research priorities but recommended further integration of patient experience research and cost-effectiveness analyses. The most critical research areas identified were improving access to care, particularly for underserved populations, addressing healthcare disparities, and advancing telemedicine to enhance remote healthcare access. A phased implementation strategy was recommended, prioritizing the top three research areas within the first few years. The final list of priorities was presented as clinical priorities and health service priorities.
Discussion
Systematic reviews on research priority setting underscore the importance of evidence-based criteria, flexible processes, and stakeholder engagement. Evidence-informed frameworks emphasize disease burden, potential health impact, and feasibility.4 Empirical studies further highlight the need for context-specific adaptations to balance technical and ethical considerations and achieve equitable health outcomes.2 The Reporting Guideline for Priority Setting of Health Research reinforces the necessity of inclusive stakeholder participation to align research priorities with community needs.3 Additionally, the World Health Organization (WHO) stresses the value of a systematic, replicable, and transparent approach to maintain integrity and accountability in priority setting.1
Our findings highlighted the intersection of clinical needs and health service research. Despite a global emphasis on patient-centered care and operational efficiency, research prioritization in the Gulf Cooperation Council (GCC) region remains underexplored, with limited frameworks integrating robust data analytics and stakeholder consensus. Addressing this gap, our study presents a replicable model for aligning research priorities with real-world health needs, ensuring clinical relevance and operational feasibility.
The high percentage related to pregnancy- and childbirth-related conditions is attributed to the absence of a designated delivery center in Muscat. Consequently, the Royal Hospital and Khoula Hospital, handle the majority of maternity cases in the governorate. In contrast, analysis of EHR data revealed that other leading causes of morbidity included atherosclerotic heart disease, cancers (notably breast and colon), and chronic conditions such as sickle cell disease and chronic kidney disease are prevalent in the Omani population. These findings align with broader trends in the GCC, where NCDs are leading health concerns.14,15 The WHO reports that NCDs account for a significant proportion of morbidity and mortality in the Middle East, with cardiovascular diseases and cancers being the primary causes of death.16
Notably, NCDs are increasingly linked to chronic inflammatory or infectious processes, challenging traditional distinctions between infectious and non-infectious diseases.17 This evolving understanding necessitates an integrated research agenda that addresses NCDs while exploring their multifactorial etiologies, including infectious origins. Given the region’s rapid urbanization and lifestyle changes, a focused research agenda is essential to address the burden of NCDs in Oman.18
Furthermore, the persistence of infectious diseases despite advancements in healthcare infrastructure, particularly pneumonia and septicemia, underscores the need for ongoing research and intervention strategies.19,20,21 Kuate Defo critiques the epidemiological transition theory for inadequately addressing such dual disease burdens, advocating for revised frameworks that recognize the coexistence of non-communicable and infectious diseases in transitional health systems.21 Research initiatives should integrate strategies for managing both disease types, ensuring a comprehensive approach that reflects the population’s diverse needs.
Beyond clinical priorities, our study identified key health service research priorities, including improving patient flow, enhancing shared decision-making, and leveraging telemedicine to improve healthcare access. These priorities align with global trends emphasizing patient-centered care and technology integration. The WHO has advocated adopting telehealth solutions, particularly in response to the COVID-19 pandemic, which accelerated innovative approaches to healthcare delivery.22,23 Other GCC countries have also recognized the potential of telemedicine to enhance access to healthcare, particularly for remote and underserved populations.24
Operational inefficiencies in resource utilization and medication management emerged as another critical research area. Studies highlight the importance of operational excellence in improving patient safety and care outcomes.25,26 Mercer suggests that integrating socio-ecological approaches into healthcare operations can address broader determinants of health, enhancing the impact of these priorities.17 Similarly, AI and machine learning offer promising avenues for improving healthcare efficiency and patient outcomes.27 Mackenbach further emphasizes that understanding transitions in healthcare priorities requires examining systemic adaptations, including the adoption of advanced technologies.28 Our study reflects this transition, highlighting the potential of digital innovations to transform healthcare delivery in the region.
Comparing our findings with regional and global research priorities reveals both similarities and distinctions [Figure 2]. Cancer research is a common priority in high-income countries, where breast and colon cancers are also emphasized.29,30 However, the high prevalence of sickle cell disease in the GCC necessitates tailored research initiatives addressing region-specific health concerns.31,32 Defo and Mercer caution against universalizing frameworks that overlook regional disease profiles, advocating for localized models that incorporate unique epidemiological and socio-ecological dynamics.17,21 Additionally, integrating health service research into priority setting reflects a growing recognition of the need for balanced approaches that encompass both clinical and health systems research.33,34 Our study contributes to this discourse by emphasizing the interconnection between clinical and operational priorities, advocating for a holistic approach to health research and service delivery.
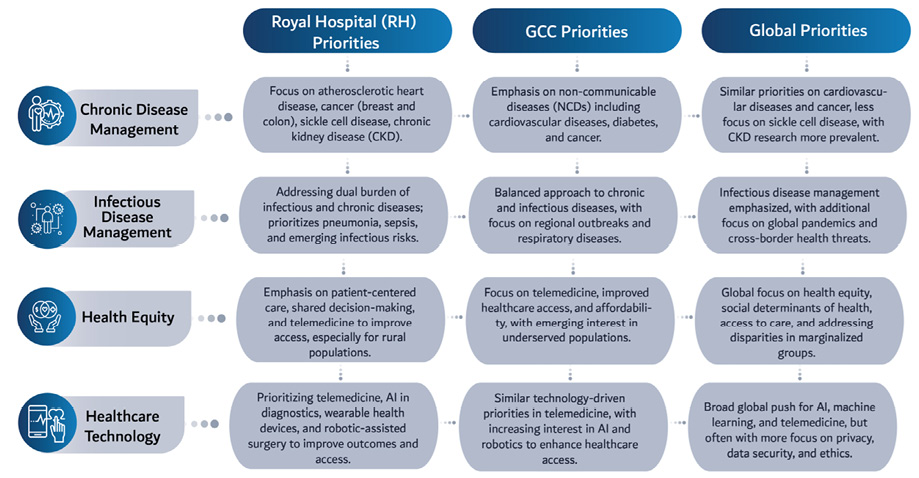 Figure 2: Comparative analysis of research priorities: hospital vs. national, Gulf Cooperation Council, and global perspectives.
Figure 2: Comparative analysis of research priorities: hospital vs. national, Gulf Cooperation Council, and global perspectives.
The research priorities identified in this study provide a framework for guiding future research initiatives at the Royal Hospital and within the broader GCC context. Aligning research efforts with clinical realities and health service challenges enhances relevance and impact. Stakeholder engagement further underscores the importance of collaborative approaches in shaping research agendas responsive to the needs of patients and healthcare providers alike. Moving forward, prioritizing these identified areas will facilitate the transplantation of research findings into actionable strategies, ultimately contributing to improved health outcomes and a more efficient healthcare system.
Conducting research in hospital settings presents unique challenges, particularly concerning resource allocation. Hospitals primarily focus on patient care, often limiting the availability of financial resources, infrastructure, and time for research activities.9,10 These constraints may also lead to resistance, as staff may perceive competing demand on already limited resources.9 Nonetheless, hospital-based research is crucial for enhancing healthcare quality, patient outcomes, and operational efficiency.
Government financial support, particularly in resource-limited regions, is essential for supporting public health research initiatives.35 Additionally, fostering a research-driven culture within hospitals can significantly impact healthcare quality.36 Translational research, which bridges the gap between research and practice, ensures that findings provide practical guidance for hospital practitioners and policymakers. Public-academic collaborations further enhance research capabilities, supporting operational efficiency, and enabling the development of evidence-based interventions.37 Incentivizing research through benchmarking and incorporating research productivity into hospital performance metrics can also promote research activities. A comprehensive approach that combines shared economic indicators, activity metrics, and quality measures facilitates trend analysis and benchmarking at national and international levels.38
A key strength of this study was the robust stakeholder engagement process, which played a critical role in validating and refining research priorities. By incorporating input from clinicians, researchers, and policymakers, the identified priorities were grounded in both evidence-based practices and the real-world needs of healthcare stakeholders. This inclusive approach aligns with global best practices emphasizing inclusivity and transparency in research priority setting, ensuring that the findings are both relevant and actionable.
Despite these strengths, the study had some limitations. While the Delphi method effectively facilitated consensus, the relatively small participant group may have constrained the diversity of perspectives and introduced bias. Participants were purposively selected based on their roles in research and strategy; however, the lack of representation from frontline staff and patients may have limited inclusiveness. Broader feedback was sought through consultations with the hospital director and section heads, and discrepancies were addressed in a live workshop, but a larger panel could have provided additional insights. Another limitation was the reliance on inpatient EHR data, which excluded outpatient. This may have limited the study’s ability to capture healthcare needs beyond inpatient settings.
Additionally, while using ICD-10 codes are systematic, they may have overlooked emerging clinical trends or nuanced diagnoses. Future research could address these limitations by involving a broader range of stakeholders and integrating outpatient data, patient-reported outcomes, and complementary methodologies to further refine the Royal Hospital’s research agenda.
Conclusion
This study established research priorities for the Royal Hospital by integrating real-world clinical data with stakeholder engagement. Using EHR analysis alongside a Delphi consensus approach, the study identified critical clinical and health service research priorities aligned with institutional needs and Oman’s Health Vision 2050. These priorities help bridge the gap between academic research and practical healthcare challenges, ensuring that research efforts are targeted, impactful, and aligned with national and global health objectives.
Key clinical priorities include cardiovascular disease, oncology, and chronic kidney disease, while health service research priorities focus on patient-centered care, telemedicine, operational efficiency, and AI-driven innovation. To facilitate implementation, a hospital-wide research steering committee should oversee the execution of identified priorities and integrate them into grant funding strategies. Strengthening data-driven decision-making through real-time EHR dashboards and AI applications will enhance predictive healthcare modeling and resource allocation.
Sustaining research momentum will require ongoing stakeholder engagement. Conducting annual reviews of research priorities with hospital leadership and policymakers, alongside fostering cross-department collaborations, will ensure alignment with evolving healthcare needs. Capacity-building initiatives should also be expanded to include specialized training in evidence-based research and innovation methodologies, complemented by structured mentorship programs for early-career researchers. For long-term sustainability, securing dedicated hospital funding and exploring public-private partnerships will be essential. By continuously refining research priorities and fostering interdisciplinary collaboration, the Royal Hospital can solidify its position as a leader in evidence-based healthcare innovation in Oman.
Disclosure
The authors declare no conflicts of interest. No funding was received for this study.
Acknowledgments
The authors sincerely thank stakeholders at the Royal Hospital for their invaluable input, as well as experts from the Planning and Studies Directorate and the Research Center of the Ministry of Health for their insightful feedback. In addition, the authors extend their gratitude to the Royal Hospital’s IT team for their support in preparing the EHR data. This manuscript benefited from ChatGPT (OpenAI) and Grammarly for language enhancement and paraphrasing.
references
- 1. World Health Organization. A systematic approach for undertaking a research priority-setting exercise. Guidance for WHO staff, 1st ed. Geneva: World Health Organization; 2020.
- 2. Barasa EW, Molyneux S, English M, Cleary S. Setting healthcare priorities in hospitals: a review of empirical studies. Health Policy Plan 2015 Apr;30(3):386-396.
- 3. Tong A, Synnot A, Crowe S, Hill S, Matus A, Scholes-Robertson N, et al. Reporting guideline for priority setting of health research (REPRISE). BMC Med Res Methodol 2019 Dec;19(1):243.
- 4. Viergever RF, Olifson S, Ghaffar A, Terry RF. A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Syst 2010 Dec;8:36.
- 5. Fleurence RL, Torgerson DJ. Setting priorities for research. Health Policy 2004 Jul;69(1):1-10.
- 6. Toffel MW. Enhancing the practical relevance of research. Prod Oper Manag 2016 Jul;25(9):1493-1505.
- 7. Bryant J, Sanson-Fisher R, Walsh J, Stewart J. Health research priority setting in selected high income countries: a narrative review of methods used and recommendations for future practice. Cost Eff Resour Alloc 2014 Nov;12:23.
- 8. Nyanchoka L, Tudur-Smith C, Thu VN, Iversen V, Tricco AC, Porcher R. A scoping review describes methods used to identify, prioritize and display gaps in health research. J Clin Epidemiol 2019 May;109:99-110.
- 9. Alvaro C, Lyons RF, Warner G, Hobfoll SE, Martens PJ, Labonté R, et al. Conservation of resources theory and research use in health systems. Implement Sci 2010 Oct;5:79.
- 10. Enzinger IH. A model for clinical research: from conceptualization to dissemination. J Nurs Educ Pract 2023;13(4):58-62 .
- 11. Al Mawali AH, Al Qasmi AM, Al Sabahi SM, Idikula J, Elaty MA, Morsi M, et al. Oman vision 2050 for health research: a strategic plan for the future based on the past and present experience. Oman Med J 2017 Mar;32(2):86-96.
- 12. World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies, 1st ed. Geneva: World Health Organization; 2010.
- 13. Agency for Healthcare Research and Quality. Six domains of healthcare quality. [cited 2025 March 25]. Available from: https://www.ahrq.gov/talkingquality/measures/six-domains.html.
- 14. Bhutani M, Price DB, Winders TA, Worth H, Gruffydd-Jones K, Tal-Singer R, et al. Quality standard position statements for health system policy changes in diagnosis and management of COPD: a global perspective. Adv Ther 2022 Jun;39(6):2302-2322.
- 15. Fandim JV, Hinman RS, Øverås CK, Sharma S, Belton J, Oliveira VC, et al. One step at a time. Shaping consensus on research priorities and terminology in telehealth in musculoskeletal pain: an international modified e-Delphi study. BMC Musculoskelet Disord 2023 Oct;24(1):783.
- 16. Boutayeb A, Boutayeb S, Boutayeb W. Multi-morbidity of non communicable diseases and equity in WHO Eastern Mediterranean countries. Int J Equity Health 2013 Aug;12:60.
- 17. Mercer AJ. Updating the epidemiological transition model. Epidemiol Infect 2018 Apr;146(6):680-687.
- 18. Bretherton CP, Claireaux HA, Gower J, Martin S, Thornhill A, Johnson L, et al. Research priorities for the management of complex fractures: a UK priority setting partnership with the James Lind Alliance. BMJ Open 2021 Nov;11(11):e057198.
- 19. Munung NS, Mayosi BM, de Vries J. Genomics research in Africa and its impact on global health: insights from African researchers. Glob Health Epidemiol Genom 2018 Jun;3:e12.
- 20. Potter S, Fairhurst K, Cowan K, Vincent S, Lewis I, Cutress RI, et al. Identifying research priorities in breast cancer surgery: a UK priority setting partnership with the James Lind Alliance. Breast Cancer Res Treat 2023 Jan;197(1):39-49.
- 21. Kuate Defo B. Beyond the ‘transition’ frameworks: the cross-continuum of health, disease and mortality framework. Glob Health Action 2014 May;7:24804.
- 22. Bridges S, Fowler S, McLaughlin L, Robichaud M, Ridgway B, Reece D, et al. How should multiple myeloma research change in a patient-oriented world? Findings and lessons from the pan-Canadian myeloma priority setting partnership. Res Involv Engagem 2023 Jul;9(1):60.
- 23. Efstathiou N, Coll AM, Ameen J, Daly W. Do Greek healthcare users and healthcare providers share cancer care priorities? Analysing the results from two Delphi studies. Eur J Cancer Care (Engl) 2011 Mar;20(2):179-186.
- 24. Shippee ND, Domecq Garces JP, Prutsky Lopez GJ, Wang Z, Elraiyah TA, Nabhan M, et al. Patient and service user engagement in research: a systematic review and synthesized framework. Health Expect 2015 Oct;18(5):1151-1166.
- 25. Fun WH, Sararaks S, Tan EH, Tang KF, Chong DW, Low LL, et al. Research funding impact and priority setting - advancing universal access and quality healthcare research in Malaysia. BMC Health Serv Res 2019 Apr;19(1):248.
- 26. Peeks F, Boonstra WF, de Baere L, Carøe C, Casswall T, Cohen D, et al. Research priorities for liver glycogen storage disease: an international priority setting partnership with the James Lind Alliance. J Inherit Metab Dis 2020 Mar;43(2):279-289.
- 27. McCreaddie M, Kuzemski D, Griffiths J, Sojka EM, Fielding M, Al Yateem N, et al. Developing nursing research in the United Arab Emirates: a narrative review. Int Nurs Rev 2018 Mar;65(1):93-101.
- 28. Mackenbach JP. Omran’s ‘epidemiologic transition’ 50 years on. Int J Epidemiol 2022 Aug;51(4):1054-1057.
- 29. Boundouki G, Wilson R, Duxbury P, Henderson J, Ballance L, Wray J, et al; Northwest Breast Research Collaborative. Patient and public priorities for breast cancer research: a qualitative study in the UK. BMJ Open 2021 Jan;11(1):e036072.
- 30. Gurusamy KS, Walmsley M, Davidson BR, Frier C, Fuller B, Madden A, et al. Top research priorities in liver and gallbladder disorders in the UK. BMJ Open 2019 Mar;9(3):e025045.
- 31. Birnie KA, Ouellette C, Marianayagam J, Campbell F, Lamontagne C, Forgeron P, et al. Partnering with youth and parents for the greatest impact of top patient-oriented priorities in pediatric chronic pain research, care and policy. Healthc Q 2022 Apr;24(SP):18-23.
- 32. Crowe S, Barker E, Roberts M, Lloyd L, de Barros CM, Rebelo-Harris B, et al. Are we asking the right questions? Working with the LGBTQ+ community to prioritise healthcare research themes. Res Involv Engagem 2021 Sep;7(1):64.
- 33. McMillan SS, Kelly F, Sav A, Kendall E, King MA, Whitty JA, et al. Using the nominal group technique: how to analyze across multiple groups. Health Serv Outcomes Res Methodol 2014 Jul;14(3):92-108.
- 34. Seki RP, Hendrie D, Daire J. Evaluation of policies for free maternal healthcare in low/middle-income countries: a scoping review protocol. BMJ Open 2019 Aug;9(8):e031557.
- 35. Guo B, Feng W, Cai H, Lin J. Influence of public hospital reform on public health: evidence from a quasi-natural experiment in China. Front Public Health 2023 Mar;11:1104328.
- 36. Robert GB, Anderson JE, Burnett SJ, Aase K, Andersson-Gare B, Bal R, et al; QUASER team. A longitudinal, multi-level comparative study of quality and safety in European hospitals: the QUASER study protocol. BMC Health Serv Res 2011 Oct;11:285.
- 37. Neri EM, Ballman MR, Lu H, Greenlund KJ, Grunbaum JA. Academic-health department collaborative relationships are reciprocal and strengthen public health practice: results from a study of academic research centers. J Public Health Manag Pract 2014;20(3):342-348.
- 38. Hadji B, Meyer R, Melikeche S, Escalon S, Degoulet P. Assessing the relationships between hospital resources and activities: a systematic review. J Med Syst 2014 Oct;38(10):127.